Abstract
Previous studies have investigated the association between cognitive frailty and falls among older adults in community; however, no study investigated this relationship among older patients living in hospital. This study aimed to examine the relationship of cognitive frailty with falls among older inpatients in Chinese hospital. Methods: This analysis consisted of 9192 older inpatients aged 65 years or over from six hospitals in China. We used FRAIL scale and Mini-Cog to assess frailty and cognitive impairment, respectively. A generalized estimating equation was used to examine the relationship between cognitive frailty and falls at 30-day follow-up. Results: Among 9192 older inpatients enrolled in this present study, the mean (SD) age was 72.40(5.72) years, with 3850(41.88%) women. The cross-sectional analysis found that after controlling for variables (age, gender, education, depression, and hospital ward cluster effect), hospitalized patients with cognitive frailty, frailty only, or cognitive impairment only at baseline were all associated with history of falls (P<0.05). At 30-day follow-up, generalized estimating equation with full-adjustment showed that inpatients with cognitive frailty were at greater risk of falls than those of non-frail and cognitive intact (OR=3.0,95%CI:1.32–6.83). This association was also observed in individuals with frailty only (OR=2.11,95%CI:1.04–4.27) but not for patients with cognitive impairment only((OR=1.11,95%CI:0.43–2.85). Conclusion: Our study suggested that hospitalized Chinese older adults with cognitive frailty were independently associated with falls. Early screening frailty and cognitive impairment were significant for older patients by clinicians, and corresponding interventions, exercise training and nutritional programs, should be implemented to prevent falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are an important serious public health problem for older adults. It is estimated that about 30% of older adults aged 65 or more fall each year globally, and the incidence of falls rose with age and frailty levels (1). Older adults with falls were associated with the risk of adverse clinical outcomes such as fracture (2), lower quality of life (3), hospitalization (4), post-fall syndrome (5), and mortality (6). With the rising population of older adults globally, prevention and management of falls have become a challenge for society.
Early identification of the risk related to falls and taken intervention were essential for the elderly. Previous studies summarized several factors contributing to falls, such as vision impairment (7), sarcopenia (8), environmental factor, and other health-related characteristics (9, 10). Frailty is a geriatric syndrome with characteristics of declined function ability and more vulnerability to stressors. A meta-analysis indicated that frailty could increase the risk of falls with the OR of 2.50(95%CI:1.58–3.96) among older people living in community (11), and a similar result was found among hospitalized patients (12). Recently, a study reported that frail older people were often coexisting cognitive impairment, a new concept of cognitive frailty, introducing by the international consensus group (13). Given previous research indicated that older people with global cognition impairment was at greater risk of falls than those with cognitive intact (14). Therefore, it is essential to understand whether the individual with cognitive frailty could have a cumulative risk of falls..
Five studies investigated the relationship between cognitive frailty and falls. The earliest cross-sectional study was performed by Tsutsumimoto et al. (15) with 10,202 older adults, reporting that older adults with cognitive frailty not only had a higher risk of falls but also fractures, compared to those with not frailty and cognitively intact. Whereas, we need to be cautious because this study was cross-sectional and unable to make a causal inference. Later, Zhao et al. (16) reported that older adults from a rural community with cognitive frailty were associated with the risk of falls. In contrast, Brigola et al (17) also conducted a cohort study with 405 older adults; the author did not find an association between cognitive frailty and falls at the four-year follow-up (OR=1.44,95%CI:0.51–4.05). We suspected the reasons might not be a larger sample size. Recently, two prospective cohort studies had investigated the relationship between cognitive frailty and falls or recurrent falls, both indicating that older inpatients with cognitive frailty were at greater risk of falls when not frailty with cognitively intact was considered as reference (18, 19). However, these above-mentioned studies were all focused on community-dwelling older people. Hospitalized older inpatients usually experienced worse health conditions. Yet, the relationship between cognitive frailty and fall risk at hospital setting is unknown.
Considering the different populations and controversial results, we believe that it is critical to explore the relationship between cognitive frailty and falls among older inpatients in a multiple-center study. We aim to examine:(a) the relationship between cognitive frailty and history of falls in the last one years); (b) the relationship of cognitive frailty with the risk of 30-day falls.
Methods
Participants and study design
This study initially was about investigating the prevalence of frailty in Chinese hospitalized inpatients aged 65 and over from multiple centers of tertiary hospitals. The original cohort study was established between October 2018 and February 2019 for the baseline survey. Six hospitals were included in this initial cohort study. Detailed study design and data collection were published before (20). In brief, we included older adults aged 65 or older with Informed consent obtaining by patients and excluded those who cannot communicate with investigators or suffer from a long-period unconsciousness. The ethics review board of Peking union medical college hospital have approved this study with the number of S-K540 and per-protocol had registered in the Chinese Clinical Trial Registry with the number of ChiCTR1800017682.
Study outcome: falls incident were obtained at baseline and during the 30-day follow-up. Investigators asked the participants about the question: Have you ever fallen in the last one year. We defined the falls as a person who was unbalanced and landed on the floor, ground, or other lower level without any intentions. We did not obtain the specific number of falls, and anyone even fallen was defined as a fall incident, and frequency of falls was categorized as no falls, and≥one fall Operationalization of frailty.
The FRAIL scale was adopted to assess the status of frailty. This frail scale consisted of five components: fatigue, weight loss, ambulation, resistance, and illness (21). The total score ranges from 0 to 5 points and categorized participants as frailty (3–5) and non-frailty (0–2).
Operationalization of cognitive impairment
Based on the hospital setting’s busy and inconvenient setting, we used a simple but reliable cognitive impairment screening tool named Mini-Cog (22). This tool integrates two parts: words memory test and clock drawing test, with the total scores ranging from 0 to 5. Older adults with the point (0–2) indicate cognitive impairment.
Definition of cognitive frailty: according to the international consensus, an individual who coexisted with frailty and cognitive impairment was considered as cognitive frailty.
Covariates
We collected the demographic characteristics, lifestyle variables, and geriatric syndrome, and other health-related factors. Demographic characteristics included age, gender (female and male), education (Illiterate, Primary, Middle, University), ethnicity (Han and others), marital status (marriage and divorced or widowed), smoking status (never smoking, current smoking and smoking before), alcohol (never, current, and quit). We classified BMI with the formula (weight-to-height ratio) as underweight (BMI<18.5kg/m2), normal (18.5 kg/m2<=BMI<24 kg/m2), overweight (BMI>=24 kg/m2), obesity (BMI>=28 kg/m2). Depression assessment was conducted by a Chinese version of the Geriatric Depression Scale-15 (GDS-15) with the total point ranging from 0 to 15, with greater scores revealing more severe depression (23). Depression was defined when the value was five or more. We also evaluated handgrip strength and nutritional status by a dynamometer and Mini Nutritional Assessment-short form (24), respectively. Low handgrip strength (<28 kg for men or <18 kg for women) was confirmed based on the criteria of the Asian Working Group for Sarcopenia (25). Nutritional status was defined into three classifications (malnutrition being 0–7, risk of malnutrition being 8–11, and no malnutrition being 12–14)..
Statistical analysis
We classified the total sample into four groups: frailty only, cognitive impairment only, cognitive frailty, and neither frailty nor cognitive impairment. Data were displayed as two types with continuous data and categorical data. We compared the difference between these four groups in terms of different variables by using Chi-square tests and one-way analysis of variance (ANOVA). Considering older patients from the same department are more likely to have similar disease conditions, we used a generalized estimating equation to adjust for the clustering effect of hospital ward and living area to examine the relationship between cognitive frailty and falls. We estimated the association by odds ratios (OR) and corresponding 95% confidential intervals (CI). Different adjusted models were listed (Model1: unadjusted; Model2: controlled for age, gender, education; Model3: controlled for age, gender, education, and hospital ward cluster effect). The data analysis was performed by SAS 9.4 software (SAS Institute Inc., Cary, NC, USA), and a 2-sided p-value <0.05 indicated statistically significant difference.
Results
Baseline Characteristics of participants
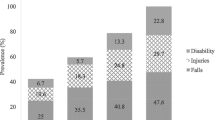
Of 9192 hospitalized patients, 498(5.42%) were cognitive frailty, 1053 (11.45%) were frailty only, 1387(15.08%) for cognitive impairment, and 6254(68.03%) were not frailty and no cognitive impairment. Overall, the mean age for this cohort group was 72.40(SD=5.72), with 3850(41.88%) women; 8683 patients (94.46%) were Han. 71.25% of the older adults aged 65–74 years. Other baseline characteristics are shown in Table 1. Compared with inpatients without frailty and cognitive impairment, those with cognitive frailty were older, had a higher proportion of underweight (12.53%) and more female, presented a higher proportion of illiterate (38.15%). The prevalence of depression (41.97%), lower handgrip strength (83.73%) and malnourished (39.96%) in cognitive frailty group were the highest among these four frailty and cognitive impairment categories, respectively. 1290(14.03%) individuals experienced at least one fall event in the last years before baseline. The prevalence of fall history among these four categories was 23.09% for cognitive frailty, 20.42% for frailty alone, 15.14% for cognitive impairment alone, and 11.99% for adults without frailty and cognitive impairment, respectively.
The cross-sectional association between frailty and cognitive impairment categories and history of fall at baseline
The results of this cross-sectional association between history of falls and categories of frailty and cognitive impairment were shown in Table 2. In the unadjusted model, older inpatients with cognitive frailty were associated with a greater risk of falls when compared to neither group (OR=1.79,95%CI:1.49–2.16). Similar findings were indicated in the frailty only group and cognitive impairment group only, with the OR of 1.67(95%CI:1.46–1.91) and 1.21(95%CI:1.04–1.41), respectively. After controlling for age, gender, and education, these mentioned-above associations were diminished. In addition, after controlling for confounding factors (age, gender, education, depression, and hospital ward cluster effect), the OR for cognitive frailty, frailty only, cognitive impairment only was 1.58(95%CI:1.29–1.92), 1.49(95%CI:1.30–1.72),1.18(95%CI:1.01–1.38), respectively.
Longitudinal association between 30-day fall and cognitive frailty categories
Table 3 presents the relationship between cognitive frailty categories and falls at 30-day follow-up. In the unadjusted model, frailty or cognitive frailty was associated with a greater risk of 30-day falls than neither (cognitive frailty: OR=3.93,95%CI:1.76–8.77; frailty only: OR=2.38,95%CI:1.16–4.89), but not for cognitive impairment (OR=1.24,95%CI:0.52–2.96). After adjusted for age, gender, and education, these mentioned-above associations were decreased. In the final adjusted model (age, gender, education, depression, and hospital ward cluster effect), the associations still significant existed with the OR of 3.0(95%CI:1.32–6.83) for cognitive frailty, 2.11(95%CI:1.04–4.27) for frailty only. However, compared with those with robust and cognitively intact, individuals with cognitive impairment only still not associated with greater risk of 30-day falls (OR=1.11,95%CI:0.43–2.85).
Discussion
Our present study was, to be the best of our knowledge, a first study that nationally represents a large-scale sample of older inpatients to examine the relationship between cognitive frailty and falls based on cross-sectional design and follow-up cohort study in China. Our research suggested that older Chinese adult inpatients with cognitive frailty were at increased risk of falls, compared to those with robust and cognitively intact, suggesting that screening frailty and cognitive impairment together was important for preventing falls among hospitalized older adults.
Several observational studies had investigated the relationship of cognitive frailty with falls among community-dwelling older adults. Regarding cross-sectional design, Tsutsumimoto et al (15). conducted a study with Japanese older adults and reported that there was a significant relationship between cognitive frailty and the history of falls, as well as frailty and cognitive impairment alone, which is compatible with our study. Recently, one study from Chinese community-dwelling older adults also showed that cognitive frailty was associated with a higher risk of history of falls compared to those who were robust participants (OR=3.51,95%CI:1.18–10.44) (18). Taken together, our study and other previous studies suggested that cognitive frailty was a risk factor that can increase the likelihood of falls. Although cross-sectional studies indicated the stronger association between cognitive frailty and falls, some recall bias might influence these results. In addition, we cannot completely decide whether cognitive frailty or fall event was the first stimulative factor based on the cross-sectional study because those older adults who experienced falls might develop frailty or cognitive impairment due to inactivity caused by fear of recurrent falls.
Recently, some prospective cohort studies focused on this topic with mixed results. Brigola et al (17). conducted a four-year follow-up study and reported that cognitive frailty increases hospitalization risk (OR=6.5,95%CI:2.20–19.60) but not falls (OR=1.44,95%Ci:0.51–4.05). In contrast, other new article of a population-based longitudinal study showed that community-dwelling older adults, with cognitive frailty, increased the risk of falls (OR=3.41,95%CI:1.11–10.50). Our study showed similar results that cognitive frailty increased the risk of falling compared to those without cognitive frailty (18). In addition, another new study also reported frailty with or without cognitive impairment is both stronger risk factor of recurrent Falls (19). Based on the previous and our studies, we believe that older adults with cognitive frailty have a higher risk of falls than those without cognitive frailty. However, this present study only focused on older inpatients that were largely different from community-dwelling older people, accompanying more severe diseases. At the same time, falls have become a serious problem for older adults living in hospitals. Once patients are fallen, fall-related injury, prolonged hospital stay, and delays in functional recovery were happened, which might lead to increased health system costs and lower quality of life (26). Our study extended the evidence that cognitive frailty was a risk factor for falls among hospitalized patients, which stresses the importance of early screening this high-risk group and implementing interventions to prevent falls.
The mechanism between cognitive frailty and falls was complex and had multiple aspects. Frailty was geriatric syndrome indicating a worse function ability of older adults. A systematic review and meta-analysis had shown that frailty was an independent risk of falls among older adults living in community (11). Meanwhile, older people with cognitive impairment were also confirmed to have an increased risk of falls (14). Therefore, when older adults suffered from these two geriatric syndromes, they were more vulnerable to adverse events. Some hypotheses believed that frailty and cognitive impairment were a reciprocal relationship, which results in a series of adverse outcomes such as mortality, disability, and dementia (27). Regarding falls, serval factors such as older age, functional impairment, poor balance, and muscle weakness were associated with falls (9, 28, 29). These factors mentioned above are some domains of frailty and cognitive impairment. Therefore, cognitive frailty might aggravate these associations between individual factors and falls, finally increasing the risk of falls. In addition, frail older adults coexisting with cognitive frailty are prone to older, possibly have a visual impairment, unable to react as quickly as young adults. When they enter a new environment, they fail to respond promptly, resulting in falls.
Our study has multiple clinical implications. To the best of our knowledge, this was the first research to explore the relationship between cognitive frailty and falls among older inpatients. Previous studies focused on community-dwelling older people, which was relatively heathier than hospitalized patients. Our study found that the association of cognitive frailty with falls were still existed among hospitalized older patients, implying that clinicians need early screening cognitive frailty and implementing corresponding intervention for falls. A published study found physical activity could mediate the relationship of cognitive frailty with falls (16). In addition, an interventional program including exercise training, nutritional program, and memory training was reported to reverse frailty measures (30). Therefore, appropriate exercise training and nutritional intervention need to be considered together with fall-related education in inpatients at discharge to reduce the fall incident.
Our study involved some strengths and limitations. First, compared to other studies with community-dwelling older adults, our study focused on unhealthy older adults (hospitalized patients), which added new evidence to this important issue. Second, we had examined the relationship between cognitive frailty and falls with a cross-sectional and longitudinal design, which help us better discern this association. Third, we adopted a generalized estimating equation to examine the relationship of cognitive frailty with falls after controlling the cluster effect of hospital wards. However, some limitations should be described. First, although we have conducted a longitudinal study, the period of follow-up was short, which might underestimate or overestimate our results. Second, the outcome of falls was measured via a questionnaire survey reported by participants, producing potential recall bias. Third, we did not use multidimensional measures to assess frailty and cognitive impairment, which might not completely reflect the overall picture of older adults. Fifth, some potential confounding factors that were not collected, which could influence our results.
Conclusion
Our study indicated that hospitalized patients with cognitive frailty had a higher risk of falls than those with robust and cognitively intact, implying the importance of early screening of cognitive frailty and implementing intervention for preventing falls.
References
Ye P, Liu Y, Zhang J, et al. Falls prevention interventions for community-dwelling older people living in mainland China: a narrative systematic review. BMC health services research 2020; 20: 808. doi: https://doi.org/10.1186/s12913-020-05645-0
Ambrose AF, Cruz L, Paul G. Falls and Fractures: A systematic approach to screening and prevention. Maturitas 2015; 82: 85–93. doi: https://doi.org/10.1016/j.maturitas.2015.06.035
Stenhagen M, Ekström H, Nordell E, Elmståhl S. Accidental falls, health-related quality of life and life satisfaction: A prospective study of the general elderly population. Archives of Gerontology and Geriatrics 2014; 58: 95–100. doi: https://doi.org/10.1016/j.archger.2013.07.006
Morris R, O’Riordan S. Prevention of falls in hospital. Clinical medicine (London, England) 2017; 17: 360–62. doi: https://doi.org/10.7861/clinmedicine.17-4-360
Mathon C, Beaucamp F, Roca F, Chassagne P, Thevenon A, Puisieux F. Post-fall syndrome: Profile and outcomes. Annals of physical and rehabilitation medicine 2017; 60: e50–e51. doi: https://doi.org/10.1016/j.rehab.2017.07.102
Burns E, Kakara R. Deaths from Falls Among Persons Aged ≥65 Years — United States, 2007–2016. MMWR Morbidity and mortality weekly report 2018; 67: 509–14. doi: https://doi.org/10.15585/mmwr.mm6718a1
Hong T, Mitchell P, Burlutsky G, Samarawickrama C, Wang JJ. Visual impairment and the incidence of falls and fractures among older people: longitudinal findings from the Blue Mountains Eye Study. Investigative ophthalmology & visual science 2014; 55: 7589–93. doi: https://doi.org/10.1167/iovs.14-14262
Zhang X, Huang P, Dou Q, et al. Falls among older adults with sarcopenia dwelling in nursing home or community: A meta-analysis. Clinical nutrition (Edinburgh, Scotland) 2020; 39: 33–39. doi: https://doi.org/10.1016/j.clnu.2019.01.002
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013; 75: 51–61. doi: https://doi.org/10.1016/j.maturitas.2013.02.009
Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2014. MMWR Morbidity and mortality weekly report 2016; 65: 993–98. doi: https://doi.org/10.15585/mmwr.mm6537a2
Cheng MH, Chang SF. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis. Journal of nursing scholarship: an official publication of Sigma Theta Tau International Honor Society of Nursing 2017; 49: 529–36. doi: https://doi.org/10.1111/jnu.12322
Lan X, Li H, Wang Z, Chen Y. Frailty as a predictor of future falls in hospitalized patients: A systematic review and meta-analysis. Geriatric nursing (New York, NY) 2020; 41: 69–74. doi: https://doi.org/10.1016/j.gerinurse.2019.01.004
Mantovani E, Zucchella C, Schena F, Romanelli MG, Venturelli M, Tamburin S. Towards a Redefinition of Cognitive Frailty. Journal of Alzheimer’s disease: JAD 2020; 76: 831–43. doi: https://doi.org/10.3233/jad-200137
Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age and ageing 2012; 41: 299–308. doi: https://doi.org/10.1093/ageing/afs012
Tsutsumimoto K, Doi T, Makizako H, et al. Cognitive Frailty is Associated with Fall-Related Fracture among Older People. The journal of nutrition, health & aging 2018; 22: 1216–20. doi: https://doi.org/10.1007/s12603-018-1131-4
Zhao D, Li J, Fu P, et al. What Role Does Activity Engagement Play in the Association between Cognitive Frailty and Falls among Older Adults? Evidence from Rural Shandong, China. Gerontology 2020; 66: 593–602. doi: https://doi.org/10.1159/000510639
Brigola AG, Ottaviani AC, Alexandre TDS, Luchesi BM, Pavarini SCI. Cumulative effects of cognitive impairment and frailty on functional decline, falls and hospitalization: A four-year follow-up study with older adults. Archives of gerontology and geriatrics 2020; 87: 104005. doi: https://doi.org/10.1016/j.archger.2019.104005
Ma Y, Li X, Pan Y, et al. Cognitive frailty and falls in Chinese elderly people: a population-based longitudinal study. European journal of neurology 2021; 28: 381–88. doi: https://doi.org/10.1111/ene.14572
Ge ML, Simonsick EM, Dong BR, Kasper JD, Xue QL. Frailty, with or without Cognitive Impairment, is a Strong Predictor of Recurrent Falls in a US Population-Representative Sample of Older Adults. The journals of gerontology Series A, Biological sciences and medical sciences 2021; glab083. doi: https://doi.org/10.1093/gerona/glab083
Jiao J, Wang Y, Zhu C, et al. Prevalence and associated factors for frailty among elder patients in China: a multicentre cross-sectional study. BMC Geriatr 2020; 20: 100. doi: https://doi.org/10.1186/s12877-020-1496-1
Woo J, Yu R, Wong M, Yeung F, Wong M, Lum C. Frailty Screening in the Community Using the FRAIL Scale. Journal of the American Medical Directors Association 2015; 16: 412–9. doi: https://doi.org/10.1016/j.jamda.2015.01.087
Zhang XM, Jiao J, Zhu C, et al. Cognitive Frailty and 30-Day Mortality in a National Cohort of Older Chinese Inpatients. Clinical interventions in aging 2021; 16: 389–401. doi: https://doi.org/10.2147/cia.S294106
Xu T, Jiao J, Zhu C, et al. Prevalence and Potential Associated Factors of Depression among Chinese Older Inpatients. The journal of nutrition, health & aging 2019; 23: 997–1003. doi: https://doi.org/10.1007/s12603-019-1270-2
Wang X, Liu M, Li Y, Guo C, Yeh CH. Community canteen services for the rural elderly: determining impacts on general mental health, nutritional status, satisfaction with life, and social capital. BMC public health 2020; 20: 230. doi: https://doi.org/10.1186/s12889-020-8305-9
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. Journal of the American Medical Directors Association 2020; 21: 300–07.e2. doi: https://doi.org/10.1016/j.jamda.2019.12.012
Hoffman GJ, Tinetti ME, Ha J, Alexander NB, Min LC. Prehospital and Posthospital Fall Injuries in Older US Adults. JAMA network open 2020; 3: e2013243. doi: https://doi.org/10.1001/jamanetworkopen.2020.13243
Yu R, Morley JE, Kwok T, Leung J, Cheung O, Woo J. The Effects of Combinations of Cognitive Impairment and Pre-frailty on Adverse Outcomes from a Prospective Community-Based Cohort Study of Older Chinese People. Frontiers in medicine 2018; 5: 50. doi: https://doi.org/10.3389/fmed.2018.00050
Van Ancum JM, Pijnappels M, Jonkman NH, et al. Muscle mass and muscle strength are associated with pre- and post-hospitalization falls in older male inpatients: a longitudinal cohort study. BMC geriatrics 2018; 18: 116. doi: https://doi.org/10.1186/s12877-018-0812-5
Lim GRS, Ng CH, Kwan YH, Fong W. Prevalence and risk factors for falls in patients with spondyloarthritis: A systematic review. International journal of rheumatic diseases 2021; 24(5):623–632. doi: https://doi.org/10.1111/1756-185x.14092
Romera-Liebana L, Orfila F, Segura JM, et al. Effects of a Primary Care-Based Multifactorial Intervention on Physical and Cognitive Function in Frail, Elderly Individuals: A Randomized Controlled Trial. The journals of gerontology Series A, Biological sciences and medical sciences 2018; 73: 1688–74. doi: https://doi.org/10.1093/gerona/glx259
Acknowledgment
We sincerely thank the staff charged for collecting data and thanks for all the individuals who participated in this study.
Funding
Funding: Peking Union Medical college have supported this study with the grant number 2018PT33001by fund.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure: All authors declare no conflicts of potential interest for this work.
Ethics and Consent Statement: Ethical approval for this study was obtained by the Ethics Committee of Peking Union Medical College Hospital [number of ethics documents: S-K540]. Patients signed this written informed consent before they participated in this study. We declared that this study was conducted to conform to the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Zhang, XM., Yuan, L., Quo, N. et al. Cognitive Frailty and Falls in a National Cohort of Older Chinese Inpatients. J Nutr Health Aging 25, 993–998 (2021). https://doi.org/10.1007/s12603-021-1670-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1670-y