Abstract
Objectives
To assess the predictability value of Sarcopenia index((SI, serum creatinine value/cystatin C value×100) in determining potential chemotherapy-induced undesirable reactions and eventual death of older patients diagnosed with stage III or IV of non-small cell lung cancer (NSCLC).
Methods
General information was retrieved from health records and mortality data was obtained by phone interview. Serum Cr and CysC levels were measured before chemotherapy. The endpoints recorded were chemotherapy-induced undesirable reactions and mortality from any causes. Logit regression analysis was employed for the analysis of correlation between the SI and short-term adverse reactions to chemotherapy. Cox regression analysis was employed to analyze correlation between the SI and mortality.
Results
In this study, 664 NSCLC patients were enrolled. Among them, 83.13% were diagnosed with adenocarcinoma lung cancer and 16.87% with squamous cell carcinoma lung cancer. As of March 1, 2019, 486 patients died, including 361(74.28%) males and 125 (25.72%) females. After the first course of chemotherapy, the proportion of short-term adverse reactions, including bone marrow suppression, digestive reactions, all infection, liver function impairment, and other adverse reactions (non-infectious fever or rashes) was 16%, 4.7%, 7.4, %, 6.6%, and 2.11%, respectively. After adjusting for confounding factors, there was no association between the SI and adverse reactions. We found that high SI was independently associated with a lower risk of mortality after adjusting for confounding factors in females (HR=0.593,95% CI: 0.382–0.92; p=0.02). There was no marked association existed between the SI and mortality in males.
Conclusion
Among patients with stage III or IV non-small cell lung cancer, the SI is associated with mortality in females, but not in males.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A majority (57%) of the lung cancer (LC) diagnosis occurs at an advanced stage of disease (1), making surgical intervention impossible. With the progress of medical technology and the continuous optimization of chemotherapy, most patients choose chemotherapy (2). Non-small cells lung cancer(NSCLC) account for 83% of LC (1), with 53% of stage III and IV NSCLC sufferers with treated by this modality (2). Although chemotherapy shows promise in improving the prognosis of NSCLC stage III and IV sufferers, LC remains the primary factor affecting cancer-related mortality, carrying a 5-year survival rate of only 18% (3).
Several studies documented that sarcopenia correlates with worse prognosis in NSCLC patients (4–6). Sarcopenia was considered a geriatric syndrome characterized by low muscle mass and inadequate mass strength and/or physical performance (7). Low muscle mass is usually measured with dual-energy X-ray absorptiometry (DXA), bioelectrical impedance analysis (BIA), magnetic resonance imaging (MRI), and computed tomography (CT), but these techniques require specialized instruments and are expensive. Therefore, it is necessary to dig a simpler method to identify low muscle mass.
Body mass index (BMI), serum levels of albumin and prealbumin are considered indicators of nutrition and muscle mass[8], but NSCLC sufferers, having standard to increased BMI, do not necessarily have better nutrition. Verily, some morbidly overweight people have been reported to have remarkably low muscle mass, while people with small constitution were reported with muscle mass proportional to their body size (9). Alterations in serum albumin and prealbumin become evident during critical stages of illness, due to the massive inflammatory spikes in the body. Therefore, changes in serum albumin and prealbumin cannot be attributed to nutritional status alone (10). These factors may not be suitable for evaluating muscle mass among patients with NSCLC.
Serum Cr and CysC are normally employed for the measurement of the glomerular filtration rate (GFR) (11, 12), but have different characteristics. Serum Cr concentration is an endogenous GFR marker reflecting end-stage muscle degeneration. Under normal circumstances, Cr is removed from the body by the kidneys, and sometimes, by tubular secretion. In contrast, CysC is an endogenous low molecular weight protein that is secreted from all cells with nycleus. It can also be removed by the kidneys, but it is not reabsorbed into the blood or actively secreted (13). In NSCLC sufferers with normal kidney function, the Cr/CysC ratio does not depend on potential differences in renal function (10), which is a chief indicator of the variations between these two markers assessing patient muscle mass (14).
Previous studies showed that the Sarcopenia index (SI, serum creatinine value/cystatin C value × 100) may be a bio-marker for muscle mass assessment in ICU patients or patients with amyotrophic lateral sclerosis or liver cirrhosis (8, 14–16), but the role of SI in predicting chemotherapy adverse reactions and mortality in patients with lung cancer is not well understood. Based on these findings, this study assessed the prognostic values of SI in assessing the risk of chemotherapy adverse reactions and mortality in older adults with stage III and IV NSCLC.
Method
Study design and population
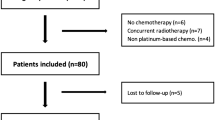
A single-institution retrospective observational study was executed at the West China Hospital, Sichuan University in Chengdu, Sichuan Province, China, between January 2010 and December 2017. The median follow-up for this sample is 28 months. For the study, we recruited stage III or IV LC sufferers, aged >60 years, who received their first course of chemotherapy for LC. The selected individuals had either adenocarcinoma or squamous carcinoma, as evidenced by histopathology. Patients with obvious renal dysfunction or with regular use of systemic corticosteroids or cyclosporin were excluded. The study was approved by the Research Ethics Committee of the West China Hospital, Sichuan University (No.2018–94).
Data collection
General characteristics (age, sex, smoking history, and number of chronic diseases), data associated with tumor (histopathology, clinical stage, metastasis, chemotherapy regimen, radiation therapy and LC surgery), blood test results before and after chemotherapy. The short-term chemotherapy-induced undesirable effects (bone marrow suppression, digestive system reactions, infection, liver function impairment), along with other undesirable effects (fever or rashes without infection) were retrieved from the anonymized electronic medical record system. Information about survival or death (all-cause mortality) as of March 1, 2019, was obtained by local government and telephone interviews. Overall survival (OS) was described as the time range between the beginning of therapy till the day of death or the last day the patient was recorded as alive.
Sarcopenia index
Experienced nurses in the geriatric ward drawn fasting (more than eight hours) vein blood in the morning before chemotherapy. Serum cystatin C concentration (mg/l) and cystatin C were measured in West china hospital lab using standard methods. We calculated the sarcopenia index using the following formula: serum creatinine value/cystatin C value × 100. According to the values of SI, all participants were separated into two groups (low or high muscle mass) according to Q3 as the cut-off value: low muscle mass from lowest to Q3 or higher muscle mass: Q3 or over (highest quantile).
Covariates
The baseline data prior to chemotherapy including age, sex, ALB level, smoking history, number of chronic diseases, data associated with tumor (histopathology, clinical stage, metastasis, chemotherapy regimen, radiation therapy and LC surgery were collected.
Statistical analysis
SPSS 26.0 (IBM Corp. Somers, NY, USA) was employed for data analysis. All information, in this paper, are presented as the mean± standard deviation (SD) or median and the interquartile range (IQR), based on distribution. For categorical variables, data were reported as numbers (percentage)for statistical description. The Rank-sum test, Student’s t test and Pearson’s chi-square test were employed for comparison of baseline features. The Logit regression analysis was employed to determine the association between the SI and short-term adverse reactions to chemotherapy. The Cox regression was employed to establish the correlation between SI and mortality. P <0. 05 was considered to indicate statistical significance.
Results
In this study, we enrolled 664 NSCLC sufferers, including 466 men and 198 women. Of them, 83.13% were diagnosed with adenocarcinoma lung cancer and 16.87% with squamous cell carcinoma lung cancer. Additionally, 229 (34.49%) were diagnosed as stage III, whereas 435 (65.51%) were stage IV. As of March 1, 2019, 468(70.48%) patients died (361 males and 125 females). Furthermore, we demonstrated differences in age, serum albumin, sex, smoking history, clinical stage, metastasis, LC surgery, infection, and other adverse reactions between the patients who died and patients who were surviving. There was no statistically significant difference in SI between the death group and the non-death group (Table 1).
After the first round of chemotherapy, the proportion of short-term adverse reactions, including bone marrow suppression, digestive reactions, all infection, liver function impairment, and other adverse reactions (non-infectious fever or rashes) were 16%, 4.7%, 7.4%, 6.6%, and 2.11%, respectively. One complication occurred in 21.99% of patients, two complications occurred in 5.27%, three complications occurred in 1.2%, and four complications occurred in 0.14% of patients. After grouping SI into two groups (as mentioned above), the incidence of short-term adverse reactions has not been statistically significant, regardless of whether it is in the total population, or among males or female, as shown in Table 2. Model1 showed there was no association between the SI and short-term adverse reactions. Model 2 showed an absence of the correlation between SI and adverse reactions (Table 3). According to Model 1 or Model 2 in the Cox regression, we found that there is no marked association existed between the SI and mortality in total or males (Table 4). Model1 showed that high SI was associated with a lower risk of mortality in females (HR=0.624, 95% CI: 0.406–0.958; p=0.031). After adjusting for confounding factors (age, sex, ALB level, smoking history, number of chronic diseases, data associated with tumor (histopathology, clinical stage, metastasis, chemotherapy regimen, radiation therapy and LC surgery)), the result also showed high SI independently associated with a lower risk of mortality in females (HR=0.593,95% CI: 0.382–0.92; p=0.02).
Discussion
The main finding of the present study is that the high SI independently associated with a lower risk of mortality in females. Therefore, the SI may provide a useful variable for predicting the risk of mortality in females with lung cancer undergoing first circle chemotherapy. In clinical practice, we can easily get the access to the SI value for inpatient admitted to hospital, which only requires a venous blood sample, which is usually covered by routine blood work. However, there was no association between the SI and the risk of short term chemotherapy adverse reactions and the predictive value of SI in predicting these outcome among the male population is unclear.
The major adverse reactions identified in the present study include bone marrow suppression, digestive reactions, all infection, liver function impairment, and other adverse reactions (non-infectious fever or rashes). However, there was no correlation between the SI and short-term adverse reactions related to chemotherapy. Suzuki and coworkers reported that a reduced proportion of Cr/CysC was related to a higher occurence of chemotherapy-induced hematotoxic undesirable reactions in NSCLC sufferers (17). The possible reason for this difference is that the severity of adverse reactions was not graded in this study, but simply the presence or absence of adverse reactions was considered.
Kashani and colleagues (8) documented that a higher SI predicted a lower mortality in ICU patients with severe disease and no renal impairment (14). However, in the latter work, after adjusting for age, sex, and gravity of disease, only the relationship between the SI and a shorter hospital stay was found to be significant. Tang TJ et al. enrolled 248 patients aged 60 years and older to analysis the correlation between SI and 3-year all-cause mortality. They reported that a higher SI was independently associated with a lower risk of 3-year all-cause mortality (18). In the present analysis, we also found that the SI is related to the mortality, with higher SI predicting a lower mortality. Although our study and that of Tang TJ and colleagues enrolled different populations, and the time during which mortality was observed was different, the results of these two investigations are similar. However, our research only found that SI is associated with all-cause mortality in females. This result needs further demonstration.
This is the first study to examine the relationship between SI and risk of chemotherapy adverse outcomes and all-cause mortality among inpatients with NSCLC population. In addition, we report sex-stratified results, Nevertheless, the present study had several limitations. First, we were unable to determine the true residual muscle mass, using the DXA or BIA procedures, owing to equipment unavailability. Therefore, the relationship between residual muscle mass and the SI in LC sufferers was not determined. Second, the baseline functional status of the included patients is also related to mortality and adverse reactions, we do not have this data and cannot be corrected. Third, the design of the present study is retrospective cohort study, which related with uncontrolled selection bias and the sample size was relatively small (n=664). Our findings need to be further confirmed by large studies with a prospective design.
Conclusion
The SI is associated with mortality of patients stage III or IV non-small cell lung cancer in females, but not in males. There was no association between the SI and adverse reactions of chemotherapy.
References
Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2012. http://seer.cancer.gov/csr/1975_2012/ (based on November 2014 SEER data submission). Bethesda, MD: National Cancer Institute, 2015.
Miller K D, Siegel R L, Lin C C, et al. Cancer treatment and survivorship statistics, 2016[J]. CA: A Cancer Journal for Clinicians, 2016, 66: 271–289.
R. Siegel, K. Miller, Jemal A. Cancer statistics, 2016. [J]. CA Cancer J. Clin, 2016, 66(1): 7–30.
Suzuki Y, Okamoto T, Fujishita T, et al. Clinical implications of sarcopenia in patients undergoing complete resection for early non-small cell lung cancer. Lung Cancer 2016; 101: 92–7.
Icard P, Iannelli A, Lincet H, et al. Sarcopenia in resected non-small cell lung cancer: Let’s move to patient-directed strategies[J]. Journal of Thoracic Disease, 2018, 10(S26): S3138–S3142.
Nakamura R, Inage Y, Tobita R, et al. Sarcopenia in Resected NSCLC: Effect on Postoperative Outcomes. J Thorac Oncol 2018; 13: 895–903.
Cruz-Jentof, A. J., Landi, F., Topinkova, E. & Michel, J. P. Understanding sarcopenia as a geriatric syndrome. Curr. Opin. Clin. Nutr. Metab. care 13, 1–7.
Kashani, Kianoush B, Frazee, et al. Evaluating Muscle Mass by Using Markers of Kidney Function: Development of the Sarcopenia Index.[J]. Critical Care Medicine, 2017, 45(1): e23–e29.
Ilich J Z, Kelly O J, Inglis J E, et al. Interrelationship among muscle, fat, and bone: Connecting the dots on cellular, hormonal, and whole body levels[J]. Agng Research Reviews, 2014, 15: 51–60.
Briskin S M, Stanford A, Davis J H, et al. Serum prealbumin: Is it a marker of nutritional status or of risk of malnutrition?[J]. Clinical Chemistiy, 2006, 52(12): 2177–2179.
Perrone RD, Madias NE, Levey AS. Serum creatinine as an index of renal function: new insights into old concepts. Clinical Chemistry, 1992; 38: 1933–1953.
Filler G, B ö Kenkamp A, Hofmann W, et al. Cystatin C as a marker of GFR—history, indications, and future research.[J]. Clinical Biochemistry, 2005, 38(1): 1–8.
Levey A S, Inker L A. Assessment of Glomerular Filtration Rate in Health and Disease: A State of the Art Review[J]. Clinical Pharmacology & Therapeutics, 2017, 102(3): 1–30.
Barreto E F, Poyant J O, Coville H H, et al. Validation of the sarcopenia index to assess muscle mass in the critically ill: A novel application of kidney function markers[J]. Clinical Nutrition, 2018, 38(2019): 1362–1367.
Tetsuka S, Morita M, Ikeguchi K, et al. Creatinine/cystatin C ratio as a surrogate marker of residual muscle mass in amyotrophic lateral sclerosis[J]. Neurology & Clinical Neuroscience, 2013, 1(1): 32–37.
Jesús Hermida, Romero R, Tutor J C. Relationship between serum cystatin C and creatinine in kidney and liver transplant patients[J]. Clinica Chimica Acta, 2002, 316(1–2): 165–170.
Kensuke, Suzuki, Hideaki, et al. Utility of creatinine/cystatin C ratio as a predictive marker for adverse effects of chemotherapy in lung cancer: A retrospective study.[J]. Journal of International Medical Research, 2015, 43: 573–582.
Tang T, Zhuo Y, Xie L, et al. Sarcopenia index based on serum creatinine and cystatin C is associated with 3-year mortality in hospitalized older patients[J]. Scientific Reports, 2020, 10(1): 1260.
Funding
Funding: 1. Collaborative Innovation Centre of Sichuan for Elderly Care and Health of China (No. YLZBZ1804) and Project of Health and family planning commission of Sichuan Province (CGY2017-101); 2. 2020 Zigong City Key Technology Support Plan (Project No. 2020YLSF19)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration of conflicting interest: The authors declare that there are no conflicts of interest.
Ethical standards: The study was approved by the Research Ethics Committee of the West China Hospital, Sichuan University (No.2018-94).
Rights and permissions
About this article
Cite this article
Chen, X., Hou, L., Shen, Y. et al. The Role of Baseline Sarcopenia Index in Predicting Chemotherapy-Induced Undesirable Effects and Mortality in Older People with Stage III or IV Non-Small Cell Lung Cancer. J Nutr Health Aging 25, 878–882 (2021). https://doi.org/10.1007/s12603-021-1633-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1633-3