Abstract
Background & aims
The Global Leadership Initiative on Malnutrition (GLIM) is new criteria for diagnosing malnutrition that need validation adjusted to race. Our aim is to determine the optimal reference values of calf circumference (CC), investigate the prevalence of GLIM-defined malnutrition based on different screening tools in inpatients over 70 years old in China and assess its relationship with clinical outcomes.
Methods
We designed two continuity studies by analyzing a prospective multicenter database. First, we estimated and validated the CC cut-off values by receiver operating characteristic analyses against in-hospital mortality. Then the patients who were at risk by NRS 2002, MNA-SF and MUST were assessed by the GLIM criteria using the new CC values. Some clinical parameters and outcome data were evaluated.
Results
The optimal cut-off values of CC were 29.6 cm for male patients and 27.5 cm for female patients. The prevalence of GLIM-defined malnutrition was 27.5% by using NRS2002, 32.6% by using MNA-SF and 25.4% by using MUST. Patients with GLIM-defined malnutrition showed significantly worse values in BMI, total protein, albumin, neutrophil/lymphocyte ratio, CC, rate of complication, in-hospital mortality, length of stay, and total hospital cost than normal patients. Multivariate logistic regression showed the odds ratio of in-hospital mortality was significantly associated with GLIM defined malnutrition by using MNA-SF [OR = 1.231, 95%CI (1.022, 1.484), P = 0.029].
Conclusions
The Chinese reference values of CC for inpatients over 70 years old were validated by in-hospital mortality, which could be implemented in GLIM criteria. And this population possessed a high prevalence of nutrition risk and malnutrition. GLIM criteria with MNA-SF seems to be the first choice to diagnose malnutrition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malnutrition is a critical problem related to many adverse clinical outcomes, especially in the elderly (1). However, till now, there are no unified assessment/diagnosis criteria of malnutrition worldwide. Recently, a consensus statement about assessment criteria for malnutrition named “Globe Leadership Initiative on Malnutrition (GLIM)” was published by several major organizations in 2019 (2). It aims to establish a global consensus for diagnosing malnutrition in clinical care settings for adults and contains two steps: the first step is risk screening by any validated screening tool and the second step is assessment of malnutrition. As a professional consensus, GLIM criteria need further validation.
NRS2002, MNA-SF and MUST were all validated screening tools recommended by ESPEN (3) and the former two were also recommended by the Geriatric Study Group from Chinese Society for Parenteral and Enteral Nutrition (CSPEN) (4). However, different screening tool may lead to different result of risk of malnutrition possessing different clinical significance (5). Definitely, it will lead to different prevalence of GLIM defined malnutrition. No research has been published that focused on how to choose the optimal screening tool.
GLIM contain two criteria with five items: phenotypic (weight loss, low BMI, and reduced muscle mass) and etiologic criteria (reduced intake or assimilation, and inflammation). There are many methods to estimate muscle mass and different method may also result in different prevalence of malnutrition (6). In GLIM criteria, anthropometry is recommended if measurement of muscle mass or its estimation by BIA is not possible or feasible and the thresholds need to be adjusted to race. However, the optimal cut-off values for CC in Chinese elderly populations were unclear.
This research consisted of two studies: (1) Study 1: determine the optimal reference values of CC in inpatients over 70 years old in China; (2) Study 2: investigate the prevalence of GLIM-defined malnutrition based on the new cut-off value of CC and different screening tools, validate its relationship with clinical outcomes and choose a screening tool for the first step of GLIM.
Materials and Methods
Participants
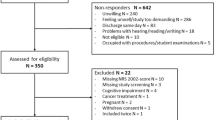
Between 1 March 2012 and 15 May 2012, a prospective multicenter cross-sectional nutrition survey was performed in consecutive geriatric inpatients in 7 major departments in 14 major hospitals in China. The original inclusion criteria included: (1) age ≥ 65 years old, (2) hospitalized overnight, (3) no emergency surgery, (4) conscious, (5) willing to collaborate and signed an informed consent. Based on the original database, we selected a part of patients to participate in this study. Besides the previous criteria, the newly added inclusion criteria were: (1) age≥70years old, (2) complete history record of weight loss, intake reduction, calf circumference (CC), BMI and diagnosis, and (3) length of stay more than 48 hours. All data extraction, analysis and examination were done by the authors and all authors were members of the establishment of the original database. Two separate studies were designed in this research.
Study 1 - Estimation and Validation of the Cut-off Values of Calf Circumference
In order to determine the cut-off value of calf circumference in Chinese population, we designed study 1 which consisted of two steps: estimation and validation (Figure 1).
In the first step, depending on the recruiting date, we selected the first one thousand males and one thousand females to form the estimation groups and performed receiver operating characteristic (ROC) curve analysis by taking in-hospital mortality as an indicator for predictive validity. In the second step, we validated the newly estimated cut-off values in comparing outcome measurements between two cohorts that fulfilled the new value or not. The participants in the validation step were all patients over seventy years old in the original database.
Study 2 - Nutrition Screening and Assessment by GLIM
A two-step model of malnutrition diagnosis was recommended in GLIM criteria, which were screening and assessment. In the first step, we used three screening tools respectively within 24 hours after admission. NRS2002 score≥3, MNA-SF scores≤11 and MUST≥2 were considered to be at risk, and the patients who fulfilled these criteria would undergo nutrition assessment by GLIM (7–9). The patients who were not at nutritional risk by any tool would be excluded to do the second step of GILM.
GILM criteria contain two parts, phenotypic criteria (three components) and etiologic criteria (two components), and fulfilling at least one component in each part is necessary to diagnose malnutrition. In phenotypic criteria, weight loss >5% within past 6 months was considered to be positive. BMI was retrieved from the original database. According to the GLIM criteria, BMI<20 was treated positive because the patients recruited in this study were all older than 70 years old. Reduced muscle mass was determined based on calf circumference (CC) and we used the newly validated cut-off values in study 1.
In etiologic criteria, food intake and assimilation reductions were reanalyzed with original data by our study group and ≤50% of requirement more than 1 week, or any reduction for more than 2 weeks were treated as positive. For disease burden or inflammation, as it was recommended in the original article that « Clinical diagnosis provides an approach to recognition of severe, chronic or frequently recurrent inflammation», the members in our study group retraced the original database and the severity of the disease in this study depended on the clinical diagnosis. Major infection, acute diseases like pancreatitis and trauma were associated with acute disease/injury-related inflammation. Chronic disease-related inflammation is found in chronic obstructive pulmonary disease, congestive heart failure, chronic renal disease, cancer and any disease with chronic or recurrent inflammation. Transient inflammation of a mild degree does not meet the criteria like minor operation.
After screening and assessment, both nutritional risk and malnutrition could be diagnosed. The patients could be divided into four cohorts depending on the pathway of diagnosing malnutrition (Figure 2): GLIM defined malnutrition using NRS2002 cohort, GLIM defined malnutrition using MNA-SF cohort, GLIM defined malnutrition using MUST cohort, and total GLIM defined malnutrition cohort.
Laboratory, Anthropometric Parameters and Outcomes
Lymphocyte count, neutrophil/lymphocyte ratio (NLR), proteins (total protein and albumin) were recorded within 72 hours after admission. The reference ranges were compiled according to the relevant provisions of the Clinical Laboratory Center, the Ministry of Health, China.
The anthropometric parameters included height, weight, and calf circumference. Standard methods of measurement were defined as follows: (1) height: measured without shoes at admission (using a scale that was corrected to ±0.5 cm); (2) weight: measured under fasting conditions wearing a hospital gown without shoes and with a corrected scale (corrected to 0.2 kg); (3) calf circumference (CC): the patient was instructed to sit to make a supine position with 90 degrees of knee flexion. The calf was measured at its strongest position using a ruler on the right leg (accurate to 0.1 cm).
Clinical outcomes were extracted from medical records including in-hospital mortality, total complications, infectious complications, length of hospital stay (LOS) and total hospital cost. Complication were defined according to the Claviene-Dindo classification system (10) and the definition of infectious complication was followed American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (11).
Statistical Analyses
SPSS21.0 software (SPSS Inc., Chicago, IL, USA, 2012) was used for the statistical analyses. The quantitative data with a normal distribution were described using means±standard deviations and tested by using t-test or Wilcoxon rank sum test. The count and the ranked data were described by using the number of cases and percentages and tested using χ2 test or Fisher’s exact test. Multivariate logistic regression models were designed. The dependent variable was in-hospital mortality and the confounding variables were different nutritional status (malnutrition determined by GLIM criteria using NRS2002, MNA-SF, MUST and that in total), diagnosis and NLR. Since BMI was a part of all tools, CC was a part of MNA-SF and GLIM, and age was a part of NRS2002, we did not treat them as confounding variables in order to prevent incorporation bias. All of the tests were two-sided, and p<0.05 was considered to indicate statistical significance.
Ethics
The original study was approved by the ethics committee of Beijing Hospital which was the leader hospital of this study (approve number: LLKYPJ2012002A), and the researcher obtained a written informed consent before the trial from every participant, and in the consent they were informed that their data could have been used for subsequent trails. The ethical principles stated in the latest revision of the Declaration of Helsinki and good clinical practice standards were applied.
Results
Study 1
Step 1 - Estimation of the Cut-off Values of CC
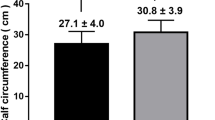
Totally, 10,184 cases from 10 major hospitals in China were enrolled between March to May 2012, among which 7,311 were over 70 years old. According to recruited date, the first 1,000 consecutive males and the first 1,000 consecutive female cases were selected to form estimation groups. In the male group, 23 (2.3%) cases had no records of CC and in the female group, the number was 21 (2.1%). So the effective cases were 977 in male group and 979 in female group, respectively. Table 1 and Figure 3 displayed the results of ROC analysis that a CC of 29.6cm for male patients and 27.5cm for female patients aged>70 years were the optimal cut-off points for predicting in-hospital mortality with statistical significance.
Step 2 - Validation of the Cut-off Values of CC
We validated the estimated cut-off values in the total database containing 7,311 cases over 70 years old. In the male group, 283 (6.4%) cases had no records of CC and in the female group, the number was 198 (6.8%). So the effective cases were 4,134 in male group and 2,696 in female group, respectively. Table 2 displayed the validation of the values. We used clinical and financial measurements and found that the newly estimated cut-off values of CC were effective to distinguish subjects with and without adverse outcomes. So, the cut-off values of CC were accepted and used in the following study.
Study 2
Basal Data of Study 2
According to the inclusion criteria of study 2, 6,519 cases were selected from the original database and figure 3 showed the detailed flow chart. Their mean age was of 78.0 ± 5.7 years, and 60.8% were male. A total of 974 (14.9%) were malignancies, among which 690 (70.8%) cases were malignance in digestive system and 195 (20.2%) cases of pulmonary cancer. The other were benign (85.1%), listing as follows: 1,113 (17.1%) were digestive diseases, 1,044 (16.0%) were respiratory diseases, 1,489 (22.8%) were cardiovascular diseases, 1,184 (18.2%) were neurologic diseases, 348 (5.3%) were orthopedic diseases, 243 (3.7%) were renal and urinary diseases, and 124 (1.9%) were other diseases. 1,448 (22.2%) cases underwent operation during their hospital stay.
Nutritional screening was performed at admission according to three different tools and different results of risks were diagnosed. Then patients at risk were assessed by GLIM. The prevalence of nutritional risk and malnutrition was displayed in table 3. The cohort that was not at risk by any screening tool contained 2,371 cases (36.4%).
Comparisons between Different Cohorts in Study 2
The comparisons of basal data, laboratory parameters, and outcomes between study groups and relative control groups were displayed in table 4. Neutrophil/lymphocyte ratio, rate of infectious and total complication, length of stay and total hospital cost were significantly higher and BMI, total protein, albumin, and CC were significantly lower in malnutrition groups. In-hospital mortality was significantly higher in the groups of GLIM defined malnutrition using NRS2002 and MNA-SF, but not in the MUST group.
Logistic Regression in Study 2
The univariate and multivariate logistic regression results for the risk of in-hospital mortality were shown in table 5. After adjusting for confounding variables like diagnosis and NLR, the odds ratio of in-hospital mortality was significantly associated with GLIM defined malnutrition by using MNA-SF [OR = 1.231, 95%CI (1.022, 1.484), P = 0.029] and NLR [OR = 1.052, 95%CI (1.037, 1.067), P = 0.000].
Discussion
In this research, we designed two studies. One was about the reference value of CC and the other was about GLIM. We discussed in details as follows.
Discussion of study 1
In the GLIM criteria, the assessment of muscle mass played an important role. The methods varied from radiologic test to anthropometry. Since the DXEA and BIA are not commonly available in hospital, we need some simple and validated methods in the clinical practice (12). CC is a good choice as it not only presents muscle mass but also bone, subcutaneous adipose, and skin. CC was proved to associate with malnutrition (13), but no cut-off value was published in Chinese inpatients. In this study, we analyzed a prospective database and estimated the reference values of CC in 2000 Chinese hospitalized elderly patients over 70 years old. Cut-off values of CC≤27.5 cm for females and ≤29.6 cm for males were determined. They were a little higher than the Japanese values, which were ≤26 cm for females and ≤28 cm for males (14) and lower than the European value in MNA-SF, which is 31cm (15). Maybe this is due to the difference between races which was emphasized in the GLIM criteria. As in a published Japanese study, we also confirmed the predictive validity against in-hospital mortality (14). What’s more, we validated the values in 7,311 consecutive cases of inpatients over 70 years old by comparing several clinical and financial outcomes between groups fulfilling the values or not. The results showed significant difference in rate of infectious complication, length of stay and total hospital cost. Therefore, we propose that the cut-off values of CC determined in study 1 would be used in Chinese hospitalized patients over 70 years old and we took it as the method to assess the muscle mass in the further research of GLIM in study 2.
Discussion of Study 2
As far as we know, this is the first research focused on the malnutrition defined by GLIM in Chinese population. In this study, we got the prevalence of malnutrition in the Chinese elderly inpatients over 70 years old which were 25.4% to 32.6% depending on different screening tools. The prevalence was similar with a Japanese cohort over 70 years old, which was 25.7% and also assessed by GLIM using MNA-SF but different CC values (16).
This is also the first research discussing the value of different screening tools in GLIM criteria. GLIM criteria consists of two steps: screening and assessment. Screening is the initiative step of nutrition support and solve the problem of whether to start nutrition care (17). The ESPEN guidelines advised to use any validated tool as the first step of GLIM but did not provide the further recommendation (2). Many studies were published to discuss the difference, indication, and effectiveness of the tools but no consensus were reached (18). In current published paper, MNA-SF and MUST were used (6, 16, 19), no one used NRS2002 and even some paper skipped the step of screening (20, 21). However, in our opinion, the nutrition assessment using GLIM should be implemented in the patients at nutritional risk screened by any tool in order to solve the problem of how to provide nutrition care and whether malnutrition exist and need to be treated (22, 23).
So in this study, we used three screening tools respectively. The rate of nutritional risk by NRS2002 was the highest among the three tools and MUST was the lowest. Meanwhile, the rate of malnutrition was highest in the MNA-SF cohort and the MUST cohort was still the lowest. By analyzing the items in the tools, MUST contains only three items: BMI, weight loss and intake reduction. Since GLIM was designed for adults in the clinical settings, we must emphasize the pathophysiology of malnutrition and the core role of disease burden and inflammation (24, 25). So no wonder MUST fail to show association with in-hospital mortality in logistic regression.
Besides weight loss, declined intake and low BMI, both NRS2002 and MNA-SF possess the items of disease burden and inflammation. In NRS2002, age more than 70 years contributed one extra score to the final result. As all the cases recruited in this study were beyond 70 years old, it was easy to reach three score of NRS2002 and the prevalence of risk looked higher. MNA-SF seemed to be more comprehensive when considering the nutrition problem in the elderly, because it contained anthropometry (calf circumference) and function evaluation like disability of daily activity and psychological problems. So it might detect more malnourished patients after GLIM assessment.
No one screening tool could pick out all cases at risk and every tool is defective (18, 26). There were overlap between cohorts and there were patients meeting all three screening criteria, meeting two criteria and meeting only one criteria. So the total malnutrition cohort was larger than any one cohort of a single screening tool. All the tools classified malnutrition were associated with worse values (BMI, total protein, albumin, and neutrophil/lymphocyte ratio), more complications, prolonged length of stay and higher hospital cost. So all the three tools could be treated as the validated tools measuring up to the GLIM recommendations. But when considering all outcomes especially in-hospital mortality in the hospitalized elderly over 70 years old, the best tool was GLIM criteria using MNA-SF, which might also find out more patients who were undernutrition.
There are some limitations in our study. (1) It was a multicentre observational study, so the difference among centres, inclusion of patients with a variety of departments and diagnosis may contribute to the heterogeneity of the study population; (2) though the original database was set up prospectively in 2012, not all the criteria of GLIM were directly contained. Our study group retraced the original data and took the items in the screening tools as reference. It may lead to some subjective bias.
In conclusion, the Chinese reference values of CC for inpatients over 70 years old were validated by in-hospital mortality, which could be implemented in GLIM criteria. And this population possessed a high prevalence of nutrition risk and malnutrition. GLIM criteria with MNA-SF seems to be the first choice to diagnose malnutrition.
References
Crichton M, Craven D, Mackay H, Marx W, de van der Schueren M, Marshall S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: associations with geographical region and sex. Age Ageing 2019; 48:38–48.
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition — A consensus report from the global clinical nutrition community. Clin Nutr 2019; 38:1–9.
Kondrup J, Alison SP, Elia M, Vellas B, Plauth M; Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN Guidelines for Nutrition Screening 2002. Clin Nutr 2003,2:415–421.
Wei J, Chen W, Zhu M, Cao W, Wang X, Shi H, et al. Guidelines for Parenteral and Enteral Nutrition Support in Geriatric Patients in China. Asia Pac J Clin Nutr 2015;24:336–346.
Xu J, Jiang Z. Different risk scores consider different types of risks: the deficiencies of the 2015 ESPEN consensus on diagnostic criteria for malnutrition. Eur J Clin Nutr 2018; 72:936–941.
Contreras-Bolívar V, Sánchez-Torralvo FJ, Ruiz-Vico M, González-Almendros I, Barrios M, Padín S, et al. GLIM Criteria Using Hand Grip Strength Adequately Predict Six-Month Mortality in Cancer Inpatients. Nutrients 2019;11:2043.
Kondrup J, Rasmusen HH, Hamberg O, Stanga Z; Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003, 22: 321–336.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNASF). J Gerontol A Biol Sei Med Sei 2001;56:M366–372.
Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr 2004; 92:799–808.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definitions for sepsis and organ failure for the use of innovative therapies in sepsis. Crit Care Med 1992;20:864–873.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 2014; 15:95–101.
Bonnefoy M, Jauffret M, Kostka T, Jusot JF. Usefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly people. Gerontology 2002; 48:162–169.
Maeda K, Koga T, Nasu T, Takaki M, Akagi J. Predictive accuracy of calf circumference measurements to detect decreased skeletal muscle mass and European society for clinical nutrition and metabolism-defined malnutrition in hospitalized older patients. Ann Nutr Metab Tab 2017; 71:10–15.
Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc 2010; 58:1734–1738.
Maeda K, Ishida Y, Nonogaki T, Mori N. Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr 2020; 39:180–184.
Mueller C, Compher C, Ellen DM; American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr 2011; 35:16–24.
van Bokhorst-de van der Schueren MA, Guaitoli PR, Jansma EP, de Vet HC. Nutrition screening tools: does one size fit all. A systematic review of screening tools for the hospital setting. Clin Nutr 2014; 33:39–58.
Matsumoto Y, Iwai K, Namikawa N, Matsuda S, Wakano C, Heya H, et al. The relationship between existing nutritional indicators and Global Leadership Initiative on Malnutrition (GLIM) criteria: A one-institution cross-sectional analysis. Clin Nutr 2020 Jan 31. pii: S0261-5614(20)30039-X.
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A. Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections e Results from a National Quality Registry. Clin Nutr 2019 Jul 20. pii: S0261-5614(19)30285-7.
Karavetian M, Salhab N, Rizk R, Poulia KA. Malnutrition-Inflammation Score VS Phase Angle in the Era of GLIM Criteria: A Cross-Sectional Study among Hemodialysis Patients in UAE. Nutrients 2019 Nov 14; 11(11). pii: E2771.
Cederholm T, Bosaeus I, Barazoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition: An ESPEN Consensus Statement. Clin Nutr 2015,34:335–340.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 2017;36:49–64.
Soeters P, Bozzetti F, Cynober L, Forbes A, Shenkin A, Sobotka L. Defining malnutrition: A plea to rethink. Clin Nutr 2017; 36:896–901.
White JV, Guenter P, Jensen G, Malone A, Schofield M; Academy of Nutrition and Dietetics Malnutrition Work Group; A.S.P.E.N. Malnutrition Task Force; A.S.P.E.N. Board of Directors. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr 2012; 36:275–283.
Probst P, Haller S, Bruckner T, Ulrich A, Strobel O, Hackert T, et al. Prospective trial to evaluate the prognostic value of different nutritional assessment scores in pancreatic surgery (NURIMAS Pancreas). Br J Surg 2017; 104:1053–1062.
Acknowledgements
The authors thank the support of members of Geriatric Study Group and [Nutritional screening — Undernutrition — Support — Outcome — Cost/effectiveness ratio (NUSOC) multicenter data sharing cooperative group] from Chinese Society for Parenteral and Enteral Nutrition (CSPEN).
Funding
Funding sources Statement: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest: The authors have no conflict of interest issue with this study.
Additional information
Statement of authorship: (I) Conception and design: JM Wei, JY Xu; (II) Administrative support: JM Wei; (III) Provision of study materials or patients: JM Wei. MW Zhu; (IV) Collection and assembly of data: JY Xu, H Zhang, L LI, PX Tang; (V) Data analysis and interpretation: JY Xu, W Chen, H Zhang, L Li; (VI) Manuscript writing: All authors; (VI) Final approval of manuscript: All authors.
Rights and permissions
About this article
Cite this article
Xu, JY., Zhu, MW., Zhang, H. et al. A Cross-Sectional Study of Glim-Defined Malnutrition Based on New Validated Calf Circumference Cut-Off Values and Different Screening Tools in Hospitalised Patients over 70 Years Old. J Nutr Health Aging 24, 832–838 (2020). https://doi.org/10.1007/s12603-020-1386-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1386-4