Abstract
Background
Mild cognitive impairment (MCI) is a transitional stage of cognitive function between normal aging and dementia. Substantial variations in the prevalence of MCI in different countries have been studied including China. In this study, we established a prediction system to assess the risk of MCI among the elderly in China.
Methods
The Rothman-Keller model was conducted on the basis of the risk factors of MCI obtained by the combined results of a meta-analysis. The accuracy of the model was verified using actual population data.
Results
A total of 1826 subjects as a verification set were enrolled in this study in February 2019. There were statistically significant differences in the combined results of 10 risk factors including hypertension, diabetes, educational level, hyperlipidemia, smoking, physical exercise, living alone, stroke, drinking and heart disease (P<0.05). The area under the curve (AUC) of the actual data and the predictive results of this model was 0.859 (95%CI: 0.812–0.906, P<0.05), the sensitivity was 86.6% and the specificity was 76.5%.
Conclusions
This model performs an effective prediction that may be applied to the primary prevention for patients with MCI, helping to reduce the risk of MCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With rapid changes in the demographic structure, the proportion of the elderly is gradually increased especially in developing countries that will lead to more the older adults being at risk of dementia. Mild cognitive impairment (MCI), a transitional stage of cognitive function between normal aging and dementia (1), is characterized by cognitive decline exceeded the expectation of age and education level without obvious functional limitations (2). As a heterogeneous disease, MCI is diverse in etiology, clinical manifestation and prognosis. Compared with the healthy individuals, patients with MCI may have several troubles in completing complex daily works in spite of functional independence. Studies have demonstrated that MCI was often discovered among the older adults in clinic. Previous reporters showed that the occurrence of MCI would increase risk of dementia (3).
At present, evidences indicate that the incidence of MCI has wide differences (4, 5), which may be correlative with diverse diagnostic criteria applied (6–8). Recent researches have mentioned that the prevalence of MCI is ranged from 6.5%–39.1% among the older adults in America, Australia, Bulgaria, Mexica and Japan (9–15). It is estimated that the number of the elderly in China will reach a peak of 487 million, accounting for 34.9% of the total population in 2050 (16). Therefore, it is crucial to identify the prevalence of MCI that assesses the potential disease burden in China, and presents the interventions to prevent or alleviate the development of dementia. Early protocols suggested that the cognitive impairment was screened using the Mini-Mental State Examination (MMSE) (17–19) or the Montreal Cognitive Assessment (MOCA) (20–22) which were lack of standard definitions of test failure. It is necessary to understand the etiologies of MCI, and to the best of our knowledge, the risk of MCI is closely associated with the age, education and chronic diseases. The Rothman-Keller model applied for evaluating the risk of chronic diseases was proposed by Rothman and Keller (23) in 1972, and this model is a common multiple-factor disease prediction model utilized for individuals in recent years, which considers the independent and interactive effects of influence factors. However, the prediction of MCI risk among elderly Chinese based on Rothman-Keller model has never been reported.
Accordingly, we established a prediction system to assess the risk of MCI among the elderly in China, which would conduct early interventions to improve the independence, cognitive function and quality of life in individuals with MCI.
Methods
Patients
Cluster random sampling method was used to select four community health service centers from Baoshan District of Shanghai. This research was approved by the Institutional Review Board (IRB) of Shanghai First People’s Hospital Baoshan Branch (approval number: 2016Y02). People over 60 years old were included in this study. The exclusion criteria were as follows: (1) patients with malignant tumors; (2) patients with dysaudia or visual impairment; (3) patients with a history of psychosis, hepatic encephalopathy and post-traumatic stress disorder. Finally, a total of 1826 people as a verification set were enrolled in this research on February 2019.
Diagnostic criteria
The diagnostic criteria of MCI were based on Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-V) published by American Psychiatric Association (2013) (24): (1) MCI with subjective and objective examinations; (2) cognitive decline in one or more domains including complex attention, executive function, learning and memory, language, perception-activity and social cognition; (3) unaffected daily living ability; (4) failing to meet the diagnostic criteria for dementia; (5) excluding other systemic diseases that may cause brain function decline; (6) MOCA scores at 22–26.
Data extraction
The risk factors of MCI were confirmed on the basis of a meta-analysis. All the patients’ information including basic characteristics (age and educational level), lifestyle (smoking, drinking, physical exercise and living alone) and disease history (hypertension, diabetes, hyperlipidemia, stroke and heart disease) were noted in the present study.
Rothman-Keller model
The predictive system of MCI was based on Rothman-Keller model (23). The previous research suggested that the incidence of MCI in the elderly was 2.17% (25). The odds ratio (OR) could estimate the relative ratio (RR) with low incidence of MCI.
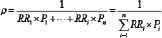
The calculation methods of Rothman-Keller model are as follows:
- (1)
The baseline incidence ratio (ρ)
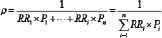
Or
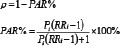
Pi: the exposure rate of a risk factor in the whole population; RRi: the relative risk of a risk factor; PAR%: the percentage of population attributable risk.
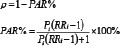
- (2)
Risk score (S)

- (3)
Total score (T)

Mi: the risk score of S≥1; Ni: the risk score of S<1.
- (4)
Individual risk of MCI (R)

MMC[: the incidence of MCI.
Statistical analysis
The statistical analysis was performed by STATA 14.0 software (Stata Corporation, College Station, TX, USA) and R software (version 3.5.0). Association between MCI and risk factors was reported as odds ratios (ORs) and 95% confidence intervals (CIs) by the fixed effect model and the random-effects model. Publication bias was performed with Begg’s test and Egger’s test (n≥10). The receiver operating characteristic (ROC) curves were conducted to assess the performance of the risk prediction Rothman-Keller model and the multivariate Logistic regression model. P<0.05 was considered as significant.
Results
The risk factors of MCI
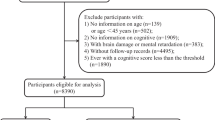
A total of 4329 citations were screened in this study. 38 articles were fully evaluated for eligibility after removing duplications, laboratory studies, reviews and meta-analyses, including 4 cohort researches and 34 case-control studies from 2006 to 2018 (26–63). The subjects were all from China, containing 21741 cases and 41924 controls. The flowchart of the study selection process was exhibited in Fig. 1.
As shown in Table 1, there were statistically significant differences in the combined results of 10 risk factors including hypertension, diabetes, educational level, hyperlipidemia, smoking, physical exercise, living alone, stroke, drinking and heart disease, and the values of combined OR were 1.880, 1.627, 2.068, 1.764, 1.950, 2.282, 2.052, 3.165, 1.897 and 2.407, respectively (P<0.05). Through the sensitivity analysis which the fixed effect model transfused to the random-effects model, the combined effect of age was unstable, and the combined results of the fixed effect model were statistically significant (OR=2.389, 95%CI: 2.088–2.726, P<0.001). while the merged results of the random-effects model were no statistical differences (OR=1.633, 95%CI: 0.737–3.618, P=0.227). Thus, the age was excluded in the model. Four factors containing hypertension, diabetes, educational level and smoking which the included studies were no less than 10, performed the publication bias using Begg’s test and Egger’s test. Our results showed that no publication bias was discovered in these four factors.
The parameters of Rothman-Keller model
The exposure levels of these pathogenic factors were respectively obtained to calculate the average exposure rate (Pi) through various studies. The combined OR values (presented as RRi) of each risk factor were assessed via merging the risk value of risk factors. The parameters of Rothman-Keller model for elderly Chinese with MCI were shown in Table 2.
The risk calculation of individuals
On the basis of the risk scores in Table 2, the combined risk scores were obtained according to the individuals’ situation (referring to Formula 3). For example, a 65-year-old people (subject A) without hyperlipidemia, living alone and heart disease, had several characteristics including hypertension, educational level >middle school, smoking, regularly physical exercise and drinking. The risk scores of these mentioned risk factors in Table 3 were 0.8262, 0.855, 0.722, 1.4086, 0.5284, 1.5674, 1.627 and 0.6751, respectively. Therefore, the combined risk score of subject A= (1.4086-1) + (1.5674-1) + (1.627-1) + 0.8262, 0.855, 0.722, 0.5284, 0.6751= 1.784. The previous study revealed that the incidence of MCI in the elderly was 2.17% (24). Thereby, the MCI risk of subject A= 2.17% x 1.784= 0.0387.
Model verification
In the present study, 1826 elderly Chinese as a verification set were screened by a random sample survey. Of these subjects, 442 cases were diagnosed as MCI containing 195 males and 247 females, and the average age was 78.22±6.64 years. 1384 normal persons (606 males and 778 females) were included, with the mean age of 71.39±4.90 years. The risk grades of the elderly with MCI were verified using the predictive results of Rothman-Keller model. The factor of onset risk over the median was defined as a high-risk factor with assignment 1, and the factor below the median was defined as a low-risk factor with assignment 0. The predictive analysis of Rothman-Keller model for MCI among the elderly was depicted in Fig. 2A. The area under the curve (AUC) of the actual data and the predictive results of this model was 0.859 (95%CI: 0.812–0.906), the sensitivity was 86.6% and the specificity was 76.5%. As shown in Fig. 2B, the AUC of multivariate Logistic regression model was 0.770 (95%CI: 0.745–0.791), the sensitivity and specificity were 86.7% and 56.1%, respectively. There were significant differences between the two models (Z=2.005, P<0.05). Our findings demonstrated that the predictive performance of Rothman-Keller model outperformed the multivariate Logistic regression model for MCI among the elderly Chinese.
Discussion
In the present study, we established a risk assessment model (Rothman-Keller model) of MCI for elderly Chinese based on a meta-analysis, and the actual data were conducted to validate the effects of this model. To the best of our knowledge, however, the prediction model has been never applied for predicting MCI among elderly Chinese, and we supposed it may be effective for the elderly to prevent the occurrence of MCI as early as possible.
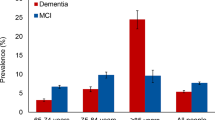
MCI is a common symptom among old adults in clinic, and the prevalence of MCI in the elderly over 65 years old is 10%–20% (64). More than half of MCI patients will progress to dementia within 5 years, and only the minority of patients can maintain stable or even normal cognitive function (2). The previous study reported that approximately 10% of MCI patients were converted to Alzheimer’s disease (AD) every year, and MCI was 10 times more likely to develop dementia than healthy people (65). Early researches suggested that the occurrence of MCI was closely associated with the age, education and chronic diseases (9, 11, 66). In the presented research, the main factors included characteristics, lifestyles and current diseases. The data from our study demonstrated that multiple indicators including hypertension, diabetes, educational level, hyperlipidemia, smoking, physical exercise, living alone, stroke, drinking and heart disease, can serve as the risk factors to predict MCI among Chinese elderly population. It is an approach of the causal prophylaxis for MCI patients to intervene unhealthy lifestyles and dietary habits. In this study, our findings found that the predictive performance of Rothman-Keller model was superior to the multivariate Logistic regression model for MCI among the elderly Chinese. The risk calculation of individuals was conducted based on the risk scores of Table 2. According to the Rothman-Keller model, the risk of MCI was obtained among the elderly. It is of clinical significance to improve the development of MCI among elderly Chinese. We suggested that high-risk groups should strengthen physical exercises, reduce the intake of high-fat, high-cholesterol and high-carbohydrate food, take regularly antihypertensive and antidiabetic drugs, and quit smoking and drinking. Furthermore, this prediction model may be used to assess the risk of the MCI elderly after intervention.
In addition, we evaluated the quality of 38 literatures according to the modified Newcastle-Ottawa Scale (NOS) score in this study, of which included 19 high quality researches and 19 low-and-moderate quality articles. It is indicated that large-scale and well-designed cohort studies should be investigated in the future, meanwhile be focused on several factors which may be greatly contributed to the prediction model, to explore the MCI risk. Then new high quality studies included in the model will be analyzed to further improve and increase the applicability of the model. Rothman-Keller model, however, is merely appropriate for the Chinese elderly, whether it can be extrapolated to other people needs further verification.
MMSE is the most widely used cognitive function assessment scale which is not sensitive to MCI. Nasreddine et al (67) finalized the MOCA scale through partially modifying the MMSE scale, which was more sensitive and specific for rapid screening of MCI patients than the MMSE scale. However, there are several differences in cultural backgrounds and living habits between the East and the West. The scale is indigestible to the Chinese people due to unfamiliar words, strange illustrations and not easily acceptable for the subjects, and the specific operations are controversial and difficult so as to affect the testing results. Furthermore, the scale is also influenced by various factors, including educational levels, skills and experience of examiners, checked environment, as well as emotional and mental state of the subjects. The RothmanKeller model as a multiple-factor disease prediction model, is also applied for individuals in recent years, which considers the independent and interactive effects of influence factors. Our investigation extracted 10 pathogenic factors, of which 4 factors containing hypertension, diabetes, educational level and smoking were predominantly considered in diverse protocols, and our research validated the prediction model with actual data to judge the predictive power and accuracy of the model.
The advantages of this study were included as follows: Firstly, we established a risk assessment model for the Chinese elderly with MCI based on a meta-analysis. Secondly, Rothman-Keller model was first applied for predicting MCI among the elderly. Additionally, the limitation of this study was that the local population were collected to verify the efficiency of the risk assessment model. Thus, it needs multi-center, large-scale and well-designed studies to further evaluate the prediction model.
Conclusion
In summary, we established a risk assessment model to predict the risk of MCI that may be applied to the primary prevention for the elderly in China, helping to reduce the occurrence of MCI.
References
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment-clinical characterization and outcome. Archives of Neurology 1999;56(3):303–308.
Gauthier S, Reisberg B, Zaudig M et al. Mild cognitive impairment. Lancet 2006;367(9518):1262–1270.
Petersen RC, Thomas RG, Grundman M et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. New England Journal of Medicine 2005;352(23):2379–2388.
Boyle PA, Buchman AS, Wilson RS, Leurgans SE, Bennett DA. Physical frailty is associated with incident mild cognitive impairment in community-based older persons. Journal of the American Geriatrics Society 2010;58(2):248–255.
Prestia A, Caroli A, van der Flier WM et al. Prediction of dementia in MCI patients based on core diagnostic markers for Alzheimer disease. Neurology 2013;80(11):1048–1056.
Petersen RC, Lopez O, Armstrong MJ et al. Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology 2018;90(3):126–135.
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment a clinical review. Jama-Journal of the American Medical Association 2014;312(23):2551–2561.
Cheng YW, Chen TF, Chiu MJ. From mild cognitive impairment to subjective cognitive decline: conceptual and methodological evolution. Neuropsychiatric Disease and Treatment 2017;13:491–498.
Petersen RC, Roberts RO, Knopman DS et al. Prevalence of mild cognitive impairment is higher in men the Mayo clinic study of aging. Neurology 2010; 75(10):889–897.
Katz MJ, Lipton RB, Hall CB et al. Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and Alzheimer dementia in blacks and whites: A report from the Einstein aging study. Alzheimer Disease & Associated Disorders 2012;26(4):335–343.
Yaffe K, Middleton LE, Lui LY et al. Mild cognitive impairment, dementia, and their subtypes in oldest old women. Archives of Neurology 2011;68(5):631–636.
Sachdev PS, Lipnicki DM, Crawford J et al. Risk profiles for mild cognitive impairment vary by age and sex: the sydney memory and ageing study. American Journal of Geriatric Psychiatry 2012;20(10):854–865.
Dimitrov I, Tzourio C, Milanov I, Deleva N, Traykov L. Prevalence of dementia and mild cognitive impairment in a Bulgarian urban population. American Journal of Alzheimers Disease and Other Dementias 2012;27(2):131–135.
Juarez-Cedillo T, Sanchez-Arenas R, Sanchez-Garcia S et al. Prevalence of mild cognitive impairment and its subtypes in the Mexican population. Dementia and Geriatric Cognitive Disorders 2012;34(5–6):271–281.
Wada-Isoe K, Uemura Y, Nakashita S, Yamawaki M, Tanaka K, Nakashima K. Prevalence of dementia and mild cognitive impairment in the rural island town of Amacho, Japan. European Journal of Neurology 2011;18:545–545.
China home to 241 million people aged 60 or above. Chinadaily 2018. Available at: http://www.chinadaily.com.cn/a/201802/26/WS5a940fb4a3106e7dcc13e2a1.html
Honig LS, Vellas B, Woodward M et al. Trial of solanezumab for mild dementia due to Alzheimer’s disease. New England Journal of Medicine 2018; 378(4):321–330.
Fox C, Richardson K, Maidment ID et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. Journal of the American Geriatrics Society 2011;59(8):1477–1483.
Visser PJ, Verhey F, Knol DL et al. Prevalence and prognostic value of CSF markers of Alzheimer’s disease pathology in patients with subjective cognitive impairment or mild cognitive impairment in the DESCRIPA study: a prospective cohort study. Lancet Neurology 2009;8(7):619–627.
Carson N, Leach L, Murphy KJ. A re-examination of Montreal Cognitive Assessment (MoCA) cutoff scores. International Journal of Geriatric Psychiatry 2018;33(2):379–388.
Nazem S, Siderowf AD, Duda JE et al. Montreal Cognitive Assessment performance in patients with Parkinson’s disease with “normal” global cognition according to Mini-Mental state examination score. Journal of the American Geriatrics Society 2009;57(2):304–308.
Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology 2011;77(13):1272–1275.
Rothman K, Keller A. The effect of joint exposure to alcohol and tobacco on risk of cancer of the mouth and pharynx. Journal of chronic diseases 1972; 25(12):711–716.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn. American Psychiatric Association 2013.
Zhuo CJ, Huang YQ, Liu ZR et al. A five-year follow-up study of mild cognitive impairment incidence in two urban and rural communities in Beijing. Chinese Mental Health Journal 2012;26(10):754–760.
Tan JP, Wang LN, Wang W. A case-control study of risk factors in mild cognitive impairment. Chinese Journal of Epidemiologyl 2006;27(1):55–57.
Sun ZW, Zhu XQ, Zhou JN. Vascular risk factors and cognitive impairment of mild cognitive impairment. Acta Universitatis Medicinalis Anhui 2007; 42(3):313–316.
Chang Q. Epidemiology and genetic background of cognitive impairment in the elderly in Beijing. Military Medical College of the Chinese people’s Liberation Army; 2007.
Xue ZL. The study of risk factors of mild cognitive impairment in community. Master. Shanxi Medical University; 2007.
Wang R. A case-control study on risk factors for mild cognitive impairment of veterans in certain selected Shaanxi areas. Master. Xi’an Jiaotong University; 2007.
Jiao FB, Tan JP, Wang LN. A case-control study on psychosocial risk factors for mild cognitive impairment in elders. Chinese Journal of Contemporary Neurology and Neurosurgery 2010;10(2):203–207.
Arsian B. A case-control study of risk factors in mild cognitive impairment. Master. Xinjiang Medical University; 2008.
Arsian B, Feng L. A comparative study on marriage and education level between Uygur elderly patients with mild cognitive impairment and normal elderly population. Xinjiang Medical Journal 2008;38(10):77–79.
Wang QQ. Effect of metabolic syndrome on mild cognitive impairment in the elderly. Master. Guizhou Medical University; 2010.
Chen SF. The relationship of plasma homocysteine, mild cognitive impairment and Alzheimer’s disease in Chenzhou. Master. University of South China; 2010.
Abdulwak A. Study of relationship between xinjiang uygur and han elderly mild cognitive impairment and plasmahomeyteine level. Master. Xinjiang Medical University; 2011.
Dong LM. The correlation between mild cognitive impairment and thyroid function in Xinjiang Uyghur and han population. Master. Xinjiang Medical University; 2011.
Jia HL, Song M, Yu L et al. Study on risk factors and protective factors of mild cognitive impairment in the elderly in Shijiazhuang community. The 9th National Symposium on Psychiatry of the Chinese Medical Association. Guangzhou; 2011:126–127.
Hui XP, Xu Y. A logistic regression analysis of risk factors for mild cognitive impairment in urban community of Suzhou. Journal of Clinical Medicine in Practice 2011;15(5):49–51.
Luo QQ. The relationship between MTHFR C677T gene polymorphism and vascular factors in the incidence of MCI. Master. Guizhou Medical University; 2011.
Lv XR. The effect of ApoE polymorphism in mild cognitive impairment. Master. Shanghai Jiao Tong University; 2011.
Wang QQ. Prevalence and risk factors of mild cognitive impairment in the elderly in Tianjin Community. Master. Tianjin Medical University; 2012..
Hai S, Dong B, Liu Y, Zou Y. Occurrence and risk factors of mild cognitive impairment in the older Chinese population: a 3-year follow-up study. International Journal of Geriatric Psychiatry 2012;27(7):703–708.
Zhong XL, Zhang ZY, Miao HJ, Zou T, Ailikemu, Zhou XH. Association between mild cognitive impairment and hypersensitive C reactive protein, interleukin-1 B and interleukin-6 in Xinjiang, China. Chinese Journal of Neurology 2013;46(11):763–768.
Lian GM, Zhu WB, Zhou DS, Liu WB, Xu Y, Chen ZM. Correlation between lifestyle factors and mild cognitive impairment in old adults. Chinese Journal of Rehabilitation Theory and Practice 2013(5):465–468.
Zeng YQ, Li LX, Wang Y. Related factors of mild cognitive impairment in elderly person: a case-control study. Hainan Medical Journal 2014(10):1427–1428.
Keyimu K, Zhou XH, Miao HJ, Zou T. Mild cognitive impairment risk factor survey of the Xinjiang Uyghur and Han elderly. International Journal of Clinical and Experimental Medicine 2015; 8(8):13891–13900.
Wang Y, Song M, Yu L et al. Mild cognitive impairment: vascular risk factors in community elderly in four cities of Hebei province, China. PLoS One 2015; 10(5):e0124566.
Xu SS, Tian XW. Risk factors of cognitive impairment in elderly patients with MCI. Chinese Journal of Practial Nervous Diseases 2015(7):49–50.
Chu ZH, Wang WJ, Han LZ, Wu L. The relationship between serum albumin, bilirubin and cognitive impairment in patients with mild cognitive impairment. The Journal of Practical Medicine 2015(17):2818–2821.
Xiao BC. Related factors of mild cognitive impairment occurrence. Journal of Clinical Research 2015; 32(12):2394–2396.
Wu TF. on Risk factors of mild cognitive impairment and folic acid intervention among the elderly in Tianjin communities: a case-control study. Master. Tianjin Medical University; 2016.
He Q, Li Q, Zhao J et al. Relationship between plasma lipids and mild cognitive impairment in the elderly Chinese: a case-control study. Lipids in Health and Disease 2016;15(1):146.
Wang F, Zhao M, Han Z et al. Association of body mass index with amnestic and non-amnestic mild cognitive impairment risk in elderly. BMC Psychiatry 2017;17(1):334.
Wang L, Wang F, Liu J, Zhang Q, Lei P. Inverse relationship between baseline serum Albumin levels and risk of mild cognitive impairment in elderly: a seven-year retrospective cohort study. The Tohoku Journal of Experimental Medicine 2018;246(1):51–57.
Feng X, Jiang FW, Ba XH. Correlation between normal thyroid function and mild cognitive impairment in the elderly. Chinese Journal of Gerontology 2017; 37(8):1904–1906.
Gao HH. Correlation between human plasma lipoprotein-associated phospholipase A2 (Lp-PLA2) and mild cognitive impairment. Master. Xi’an Jiaotong University Health Science Center; 2017.
Liu JX, Yang Q, Sun F, Wang SQ, Hu W, Liu R. Risk factors and multivariate analysis of elderly patients with MCI. Stroke and Nervous Diseases 2018; 25(2):197–199.
Ran F, Sun WM, Wang LY, Wang HG, Zhang Y. Correlation between serum uric acid level and mild cognitive impairment. Modern Instruments 2018;24(1):84–85, 94.
Shi Y. Study on the prediction model for influence factors of mild cognitive impairment. Master. Qingdao University; 2018.
Tang YL, Wei W, Wei J et al. Study on risk factors of mild cognitive impairment in Dahua Yao nationality. Clinical Research and Practice 2017;2(33):115–116.
Hu MY. The correlation between tobacco intake and mild cognitive impairment in the elderly. Master. Jilin University; 2018.
Wang H. Influence factors of mild cognitive impairment in urban of Northern China. Master. Chinese Center For Disease Control And Prevention; 2017.
Petersen RC. Mild cognitive impairment. New England Journal of Medicine 2011;364(23):2227–2234.
Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JPG, Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Annals of Neurology 2008;63(4):494–506.
Afgin AE, Massarwa M, Schechtman E et al. High prevalence of mild cognitive impairment and Alzheimer’s disease in Arabic villages in Northern Israel: impact of gender and education. Journal of Alzheimers Disease 2012; 29(2):431–439.
Nasreddine ZS, Phillips NA, Bedirian V et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society 2005;53(4):695–699.
Acknowledgement
This work was supported by Fund Project of Shanghai Science and Technology Commission (No. 16411972900).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This research was approved by the Institutional Review Board of Shanghai First People’s Hospital Baoshan Branch (approval number: 2016Y02).
Additional information
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, B., Shen, T., Mao, L. et al. Establishment of a Risk Prediction Model for Mild Cognitive Impairment Among Elderly Chinese. J Nutr Health Aging 24, 255–261 (2020). https://doi.org/10.1007/s12603-020-1335-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1335-2