Abstract
Objectives
-
(i)
To investigate serum myostatin (absolute and normalized for total body lean mass (TBLM)) and IGF-1 as biomarkers of frailty and low relative appendicular skeletal muscle mass (RASM) in older adults, and;
-
(ii)
to examine gender differences in the association of serum myostatin and IGF-1 levels with frailty and low RASM.
Design
Cross-sectional study.
Setting
The “Longitudinal Assessment of Biomarkers for characterization of early Sarcopenia and predicting frailty and functional decline in community-dwelling Asian older adults Study” (GERI-LABS) study in Singapore.
Participants
200 subjects aged 50 years and older residing in the community.
Measurements
Frailty was assessed using the modified Fried criteria. Low RASM was defined using cutoffs for height-adjusted appendicular skeletal muscle mass measured by dual-energy X-ray absorptiometry as recommended by the Asian Working Group for Sarcopenia. Comorbidities, cognitive and functional performance, physical activity and nutritional status were assessed. Blood samples collected included serum myostatin, insulin-like growth factor 1 (IGF-1) and markers of inflammation (total white cell count, CRP, IL-6 and TNFaR1). Subjects were classified into 4 groups: Frail/Prefrail with low RASM (Frail/Low RASM), Frail/Prefrail with normal RASM (Frail/Normal RASM), Robust with low RASM (Robust/Low RASM) and Robust with normal RASM (Robust/Normal RASM).
Results
63 (32%) subjects were classified as Frail/Low RASM, 53 (27%) Frail/Normal RASM, 28 (14%) Robust/Low RASM and 56 (28%) Robust/Normal RASM respectively. Frail/Low RASM subjects were older and had lower BMI compared to Frail/Normal RASM and robust subjects. Mean (SE) normalized myostatin levels were higher in Frail/Low RASM compared to Frail/Normal RASM subjects (1.0 (0.04) versus 0.84 (0.05) ng/ml/kg, P=0.01). Median (IQR) IGF-1 level was lower amongst Frail/Low RASM subjects compared to Frail/Normal RASM subjects (102.3, (77.7, 102.5) vs 119.7 (82.7, 146.0) ng/ml, P=0.046). No differences in myostatin or IGF-1 were observed among robust individuals with or without low muscle mass. In adjusted multinomial logistic regression models with Robust/Normal RASM as the reference group, myostatin (P=0.05) and IGF-1 (P=0.043) were associated with Frail/Low RASM status in the whole cohort. When stratified by gender, myostatin was significantly associated with Frail/Low RASM status in men only (P=0.03). In women, serum IGF-1 was associated with Frail/Low RASM status (P=0.046), but not myostatin (P=0.53).
Conclusion
Serum myostatin, normalized for TBLM in men and IGF-1 in women are potential biomarkers for frail individuals with low RASM, and may identify a target group for intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advancing age is associated with striking changes in body composition, with the progressive age-related decline in skeletal muscle mass and function known as sarcopenia (1). Sarcopenia is associated with a high risk of negative health outcomes such as falls, physical disability and mortality, and is a major contributor to healthcare costs (2, 3). On the other hand, frailty refers to a multidimensional syndrome characterized by reduced homeostatic reserves, increasing an individual’s vulnerability to stressors and placing the individual at risk of adverse outcomes akin to sarcopenia (4). While multiple operational definitions of frailty exist, the phenotype approach defines physical frailty as a syndrome with clinically recognizable features of weight loss, decreased grip strength, exhaustion, slowness and low physical activity (5). A decline in strength attributed to sarcopenia is hypothesized to presage frailty onset and falls into a self-perpetuating vicious cycle, leading to the notion of sarcopenia as being a biological substrate for the initiation and progression of physical frailty (6).
Whether sarcopenia is a predominant process in the pathogenesis of physical frailty may be influenced by various pathways through which an equilibrium between catabolic and anabolic processes in muscle homeostasis is maintained. For instance, myostatin, a member of the transforming growth factor β (TGF-β) superfamily is an endogenous inhibitor of myogenesis, whereas insulin-like growth factor 1 (IGF-1) is a circulating hormone with anabolic effects on muscle. However, existing studies examining the relationship between myostatin and IGF-1 with sarcopenia and frailty have yielded inconsistent results. Some studies reported the “expected” association that myostatin levels are inversely related to muscle mass (7, 8), whereas others have reported opposite findings (9–11) or a lack of association (12). Similarly, for IGF-1, results have ranged from the association of low levels with sarcopenia, frailty and disability (13–15) to the lack of association (16). While the exact mechanisms remain to be elucidated, several possibilities have been proposed. From the measurement perspective, inconsistent results in the association between myostatin with muscle mass and function typically involve studies which report absolute myostatin levels (7, 9) and may reflect the confounding influence of age and total muscle mass on circulating myostatin. To circumvent this, it is proposed that myostatin levels should be adjusted for age and normalized to total body lean mass (17). Furthermore, there is increasing attention within the field about the gender-specific modulation of sarcopenia risk by myostatin and IGF-1 signalling, such that sarcopenia is driven by the catabolic influence of myostatin in men and anabolic decline represented by reduced IGF-1 in women. It was recently reported that high myostatin levels were associated with sarcopenia in men only whereas serum IGF-1 level was significantly lower amongst female sarcopenic subjects (18); similarly, low IGF-1 levels was associated with impaired handgrip strength in women, but not in men (19). Taken together, this suggests that different pathophysiological mechanisms, some gender-specific, may underlie the development of frailty and sarcopenia, such that biomarkers may only relate to specific pathogenic pathways or phenotypes of either condition (20). In this context, we aim to examine the role of myostatin and IGF-1 as biomarkers of frailty in the presence and absence of low skeletal muscle mass in a cohort of fully independent, community-dwelling older adults, and to examine if this association is modified by gender.
Methods
Study population
The “Longitudinal Assessment of Biomarkers for characterization of early Sarcopenia and predicting frailty and functional decline in community-dwelling Asian older adults Study” (GERI-LABS) is a prospective cohort study involving cognitively intact and functionally independent adults aged 50 years and older residing within the community. Two hundred subjects were recruited between August 2013 and July 2014. The current study involves cross-sectional analysis of myostatin and IGF-1 levels with baseline clinical and blood biomarker assessments.
Ethics approval for the study was obtained from by the Domain Specific Review Board of the National Healthcare Group and informed written consent was obtained from the participant.
Inclusion and exclusion criteria
Subjects were included if they were (i) aged 50 to 99 years at study enrolment, (ii) community-dwelling, and (iii) independent in both activities of daily living (ADLs) and instrumental ADLs (IADLs). We excluded subjects with a known history of dementia or evidence of cognitive impairment using a locally-validated modified Chinese version of mini-mental state examination (CMMSE) cut-off score ≤21 (21) and subjects who were unable to walk at least 4.5 m independently (those with symptomatic heart disease, movement disorders, requiring assistance in ambulation or inability to ambulate independently with a walking aid). Residents of sheltered or nursing homes were also excluded.
Measurements
Clinical assessments
We collected demographic data and comorbid vascular risk factors, including hypertension, hyperlipidemia, diabetes mellitus, atrial fibrillation, peripheral vascular disease, stroke or transient ischemic attack and ischemic heart disease based on self-report or the use of disease-specific medications. The presence of chronic inflammatory disease and malignancy was documented. Body mass index (BMI) was calculated from measurements of standing height and body weight. Nutrition was assessed using the locally-validated Mini Nutritional Assessment (MNA) questionnaire (22). Functional performance in basic activities of daily living (ADL) was evaluated using Barthel’s index (23) and instrumental ADL using Lawton and Brody’s (IADL) index (24).
Laboratory assessments
Venous blood sample was obtained at baseline for measurement of serum albumin, C-reactive protein and full blood count, performed in the clinical laboratory of Tan Tock Seng Hospital, Singapore.
Serum obtained following centrifugation at 3000 rpm for 10 min was aliquoted and stored at −80 °C until analysis for myostatin (Immundiagnostik AG, Bensheim), insulinlike growth factor-1 (IGF-1) (BioVendor, Czech Republic), interleukin-6 (IL-6) (eBioscience, San Diego, CA, USA) and TNFa receptor-1 (TNFaR1) (R&D Systems, Minneapolis, MN, USA). All assays were performed according to the manufacturers’ recommendations and measured in duplicates, with detection limits of 0.4 ng/ml for myostatin, 5 ng/ml for IGF-1, 0.1 pg/ml for IL-6 and 15 pg/ml for TNFaR1. To interpret myostatin concentrations within the context of an individual’s lean mass, relative myostatin concentrations were calculated by normalizing to total body lean mass (TBLM) (17). The estimated marginal means of normalized myostatin levels adjusted for age were analysed, due to the significant effect of age on circulating myostatin levels (17, 25).
Assessment of frailty and muscle mass
Frailty was defined using the modified Fried criteria (5). Grip strength was measured using the hydraulic hand dynamometer (North Coast™ Hydraulic Hand Dynamometer). Two trials of grip strength were obtained for each hand with all 4 trials averaged to yield a final strength score. Gait speed was based on the time taken to walk 3 metres. Published Asian cutoffs were used to define each frailty sub-item (grip strength <26 kg for men and <18 kg for women scored as 1; and gait speed <0.8 m/s scored as 1) (26). Low physical activity was defined using the pentile cutoff of ≤29 on the Frenchay Activities Index (27). Lastly, we modified 2 questions from the Center for Epidemiologic Studies-Depression Scale (CES-D) to assess fatigue. Participants answered yes/no to the following: (a) I felt that everything I did was an effort, and (b) I could not get “going”. The frailty sub-item of fatigue was considered positive if either question was endorsed. The 5 items were summated to yield a total score (range 0–5), which corresponded respectively to frail (3–5), pre-frail (1–2), and robust (0) health status.
Lean mass measures were obtained via a dual-energy X-ray absorptiometry (DXA) system (Discovery™ APEX 13.3; Hologic, Bedford, MA, USA). Appendicular skeletal mass was derived from the summation of fat-free lean body mass in the four limbs. Relative appendicular skeletal muscle mass (RASM) was calculated using the Asian Working Group for Sarcopenia (AWGS) recommended gender specific cut-off values for height-adjusted appendicular skeletal muscle mass (ASM/height2) (26). As the AWGS definition of sarcopenia includes low muscle strength and physical performance, we only used muscle mass criteria in our study to avoid overlap with components of the modified Fried criteria (9).
Using the aforementioned criteria for frailty and low muscle mass, we classified subjects into 4 groups: Frail/Prefrail with low RASM (Frail/Low RASM), Frail/Prefrail with normal RASM (Frail/Normal RASM), Robust with low RASM (Robust/Low RASM) and Robust with normal RASM (Robust/Normal RASM). Frail (N=11) and prefrail (N=105) subjects were considered together due to small numbers of frail subjects (5.5%) in this relatively healthy community-dwelling cohort.
Statistical analysis
Continuous variables were expressed as means (standard error) or as medians (interquartile range). Categorical variables were expressed as counts and percentages. Univariate analyses were performed comparing between frailty subgroups (Frail/Low RASM versus Frail/Normal RASM and Robust/Low RASM versus Robust/Normal RASM) in baseline demographics, clinical measures of cognitive, functional and physical performance, nutritional status, comorbidities and laboratory assessments, including serum myostatin and IGF-1. Independent sample t-tests were used for parametric data and Mann-Whitney U test for non-parametric continuous variables. Chi-square tests were used for categorical variables.
Multinomial logistic regression was used to identify normalized serum myostatin, IGF-1 and clinical characteristics as independent predictors for individuals classified as Frail/Low RASM, Frail/Normal RASM and Robust/Low RASM with Robust/Normal RASM as the reference group. We then performed the regression analyses according to gender in order to further elucidate gender-specific predictors of frailty and low muscle mass. Two-sided tests with a significance level of P < 0.05 were applied. Statistical analysis was carried out using Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.
Results
Demographic and clinical characteristics
We enrolled 200 subjects with a mean age of 67.9 (7.9) years. Table 1 summarizes the demographic characteristics. One hundred and eighty-four (92%) subjects were of Chinese ethnicity and 137 (68.5%) were women. Eighty-four (42%) were robust, 105 (52.5%) pre-frail and 11 (5.5%) frail. The distribution of the four groups was 63 (31.5%) Frail/Low RASM, 53 (26.5%) Frail/Normal RASM, 28 (14.0%) Robust/Low RASM and 56 (28%) Robust/Normal RASM respectively. The proportion of frail individuals with normal RASM was 45.7%. The mean age of Frail/Low RASM subjects was older (71.7 (1.0) years) compared to Frail/Normal RASM (68.4 (1.0) years), Robust/Low RASM (66.1 (1.5) years) and Robust/Normal RASM subjects (64.3 (0.9)) (P for trend < 0.001). There were no significant differences in the medical comorbidities of hypertension, diabetes mellitus, hyperlipidemia and ischemic heart disease between the three groups. Frail/Low RASM subjects had the lowest BMI and total body lean mass along with the lowest total body fat mass and percentage body fat. Subjects with low RASM had poorer nutritional status based on MNA scores compared to subjects with normal RASM, regardless of frailty status.
Laboratory assessments
Laboratory assessments between the four groups are shown in Table 2. There were no significant differences in absolute serum myostatin between the groups. However, for a given amount of total body lean mass (TBLM), mean (SE) ageadjusted myostatin levels were higher for Frail/Low RASM subjects compared to Frail/Normal RASM subjects (1.0 (0.04) versus 0.84 (0.05) ng/ml/kg, P=0.01). Normalized myostatin levels did not differ between robust individuals regardless of muscle mass. Median (IQR) IGF-1 levels were significantly lower amongst Frail/Low RASM subjects compared to Frail/Normal RASM subjects (102.3, (77.7, 102.5) versus 119.7 (82.7, 146.0) ng/ml, P=0.046). There were no differences in IGF-1 levels between robust subjects with low or normal RASM. Levels of inflammatory markers (Total white cell count, CRP, IL-6 and TNFaR1) did not differ between the groups.
Association of myostatin and IGF-1 with frailty and muscle mass stratified by gender
In both men and women, there were no differences in absolute myostatin levels between the groups. However, normalized myostatin levels were higher in frail men and women with low muscle mass compared to frail individuals with normal muscle mass (Men: 0.81 (0.05) versus 0.65 (0.06) ng/ml/kg, P=0.01, Women: 1.09 (0.05) versus 0.93 (0.05) ng/ml/kg, P=0.01). Frail/Low RASM men also had significantly higher myostatin levels compared to Robust/Normal RASM men (0.81 (0.05) versus 0.59 (0.06) ng/ml/kg, P=0.001). There were no differences in normalized myostatin levels observed in robust subjects regardless of muscle mass status. Overall, normalized myostatin levels were higher in women compared to men. (Table 2).
IGF-1 levels were lower in Frail/Low RASM compared to Frail/Normal RASM women (100.1 (76.0, 119.2) versus 114.5 (86.6, 136.4) ng/ml, P=0.07). Frail/Low RASM women also had significantly lower IGF-1 levels compared to Robust/Normal RASM women (100.1 (76.0, 119.2) versus 117.6 (97.5, 146.0) ng/ml, P=0.02). In men, no differences were observed in IGF-1 levels between the groups (Table 2).
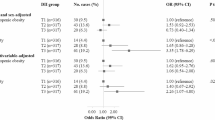
Multinomial logistic regression for frailty and muscle mass outcomes stratified by gender
In adjusted multinomial logistic regression models, myostatin normalized for total body lean mass and IGF-1 were significantly associated with Frail/Low RASM status (β: 1.7, 95% CI 0.001 – 3.5, P=0.05 and β: −0.014, 95% CI −0.027 – −0.0004, P=0.043; Table 3). These associations were not observed for subjects who were robust or with normal muscle mass. When stratified by gender, normalized serum myostatin was significantly associated with Frail/Low RASM status in men only (β: 7.2, 95% CI 0.70 – 13.7, P=0.03). In contrast, serum IGF-1 was significantly associated with Frail/Low RASM status in women (β: −0.016, 95% CI −0.033 – −0.0003, P=0.046), but not myostatin (P=0.53) (Table 4).
In the analysis of other covariates in the model, increasing age was also associated with increased risk of frailty regardless of muscle mass, but not with subjects who were robust. Higher BMI was associated with decreased risk of low muscle mass in both frail and robust subjects.
Discussion
In the present study, we identified the gender-specific association between serum myostatin and IGF-1 with coexistent frailty and low muscle mass in a group of healthy, community-dwelling older adults. While older age and lower BMI are associated with being both frail and having low muscle mass in both sexes, higher levels of myostatin normalized for total body lean mass were associated with co-existent frailty and low muscle mass only in men whereas this association was not observed in women. Conversely, lower IGF-1 levels were associated with co-existent frailty and low muscle mass only in women. These findings suggest gender-specific pathways in the development of frailty, whereby myostatin regulation of muscle mass may contribute to frailty development through sarcopenia in men. In contrast, the IGF-1-dependent anabolic pathway may predominate in women.
We adopted the approach by Bergen et al (17), analysing serum myostatin normalized for total body lean mass. This approach accounts for the age-associated decline in muscle mass, with the resultant relationship between high myostatin levels and low muscle mass concordant with the role of myostatin as a negative regulator of muscle growth. In the aforementioned study, circulating myostatin is modestly correlated with skeletal muscle mass (r = 0.24) (17). A failure to adjust myostatin levels for muscle mass may thus explain, in part, previous contradictory findings (9). Other possible explanations may include the lack of data on the biological relevance of circulating versus muscle expression of myostatin, as myostatin abundance may not reflect myostatin activity (28). Even when myostatin levels can be quantified, the activity of myostatin precursor forms may not be accounted for (29). In addition, the complex regulation of myostatin by interacting proteins such as follistatin, follistatin-related gene (FLRG) and GDF-associated serum protein-1 (GDF-1) remains to be clarified (30).
Age and gender also confounds the association of circulating myostatin with muscle mass. Our study corroborates previous findings, where higher myostatin levels are observed in older, sarcopenic women compared to younger women, whereas in men, the opposite is observed, suggesting the role of myostatin as a homeostatic regulator of muscle mass in men with aging (17). While mechanisms underlying the sexually dimorphic actions of myostatin have yet to be elucidated, lower myostatin levels are hypothesized to be protective against the loss of skeletal muscle mass and strength, possibly mediated through inflammation (31), although markers of inflammation were not associated with frailty and low muscle mass in our cohort. Other possible reasons for the age-associated decrease in myostatin in men include an adaptive response to an unfavourable metabolic state (32) or changes in sex hormones, which may regulate skeletal muscle growth mediated by the adipomyokine irisin (33).
Our results showing an association between lower IGF-1 levels with frailty and low muscle mass in older women parallel previous findings of a similar association of IGF-1 with grip strength (19) and disability (15) among women, but not in men. Lower IGF-1 levels are associated with impaired muscle strength and function, with IGF-1 mediating muscle growth and regeneration through inhibition of muscle atrophy pathways (34). In the present study, while we show a statistically significant association between IGF-1 and frailty with coexistent sarcopenia in women, the magnitude of this association is small, suggesting that that other mechanisms may be relevant in the pathogenesis pathway from sarcopenia to frailty in women.
In our cohort, the gender-specific association of myostatin and IGF-1 was observed in frail adults with low muscle mass only. This association was not present in robust adults even with low muscle mass, which may reflect either a systemic frailty-associated physiological dysregulation of skeletal muscle protein metabolism independent of age, or a later, more severe stage of sarcopenia where muscle mass, strength and performance measures are impaired, a concept which parallels contemporary definitions of sarcopenia (35). Our study thus adds to the body of knowledge on biomarkers of sarcopenia and frailty, as previous studies have only examined biomarkers related to muscle mass or physical performance in isolation.
Given the paucity of data in healthy community-dwelling older adults, further longitudinal studies are required to elucidate causal relationships between serum myostatin and sarcopenia in the pathogenesis of frailty, and to investigate the influence of inflammation, metabolic disease and sex hormones on this relationship. Understanding this relationship will have therapeutic implications in terms of the potential role of using myostatin as a blood biomarker to select the target population who will best respond to myostatin inhibitor therapy (36), for instance, pre-frail older men with dynapenia (or ‘probable sarcopenia’ based on the recent EWGSOP2 criteria (35)) who are at increased risk of adverse health outcomes without early intervention.
The strengths of this present study include a well-characterized community-based population and comprehensive evaluation with well-established definitions of frailty and sarcopenia specific to an Asian population. The use of normalized levels of myostatin also enabled us to elucidate the gender-specific association with co-existent frailty/low muscle mass despite the relatively small sample size.
Nonetheless, there are several limitations. Firstly, the cross-sectional design of the study limits the determination of causality between the clinical and biomarker characteristics with sarcopenia and frailty status. Secondly, the sample size precludes more elaborate subgroup analysis, and a type II error cannot be excluded. The small sample size also resulted in large confidence intervals if estimates of relative risk were used, thus the multinomial logit coefficient was reported as a measure of association. Thirdly, the selection of healthier cognitively intact community-dwelling adults enrolled in this study may limit the generalizability of the current results to a more heterogeneous population of frailer older adults. Fourthly, we used DXA measurements of lean mass as an estimate of appendicular skeletal muscle mass; studies suggest that DXA-derived lean mass do not correlate well with measures of muscle function such as physical performance and mobility (37). Nevertheless, the use of DXA is in line with recommendations by the International Clinical Practice Guidelines for Sarcopenia (38).
In summary, the present study showed that myostatin in men and IGF-1 in women are potential biomarkers for coexistent sarcopenia and frailty in community-dwelling older adults. Our results suggest the putative role of gender-specific catabolic and anabolic pathways in co-existent sarcopenia and frailty, and possibly pathophysiological mechanisms independent of sarcopenia in the pathogenesis of frailty. Further longitudinal studies to disentangle the underlying mechanisms of sarcopenia and frailty will be crucial in identifying appropriate biomarkers, treatment targets and developing therapeutic interventions to ameliorate frailty in older adults.
References
Rosenberg, I.H., Sarcopenia: origins and clinical relevance. J Nutr, 1997;127(5 Suppl): p. 990S–991S.
Woo, J., J. Leung, A. Sham, et al., Defining sarcopenia in terms of risk of physical limitations: a 5-year follow-up study of 3,153 chinese men and women. J Am Geriatr Soc, 2009;57(12): p. 2224–31.
Arango-Lopera, V.E., P. Arroyo, L.M. Gutierrez-Robledo, et al., Mortality as an adverse outcome of sarcopenia. J Nutr Health Aging, 2013;17(3): p. 259–62.
Clegg, A., J. Young, S. Iliffe, et al., Frailty in elderly people. Lancet, 2013. 381(9868): p. 752–62.
Fried, L.P., C.M. Tangen, J. Walston, et al., Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci, 2001;56(3): p. M146–56.
Landi, F., R. Calvani, M. Cesari, et al., Sarcopenia as the Biological Substrate of Physical Frailty. Clin Geriatr Med, 2015;31(3): p. 367–74.
Yarasheski, K.E., S. Bhasin, I. Sinha-Hikim, et al., Serum myostatin-immunoreactive protein is increased in 60–92 year old women and men with muscle wasting. J Nutr Health Aging, 2002;6(5): p. 343–8.
Leger, B., W. Derave, K. De Bock, et al., Human sarcopenia reveals an increase in SOCS-3 and myostatin and a reduced efficiency of Akt phosphorylation. Rejuvenation Res, 2008;11(1): p. 163–175B.
Peng, L.N., W.J. Lee, L.K. Liu, et al., Healthy community-living older men differ from women in associations between myostatin levels and skeletal muscle mass. J Cachexia Sarcopenia Muscle, 2018.
Arrieta, H., G. Hervas, C. Rezola-Pardo, et al., Serum Myostatin Levels Are Higher in Fitter, More Active, and Non-Frail Long-Term Nursing Home Residents and Increase after a Physical Exercise Intervention. Gerontology, 2018;p. 1–11.
Fife, E., J. Kostka, L. Kroc, et al., Relationship of muscle function to circulating myostatin, follistatin and GDF11 in older women and men. BMC Geriatr, 2018;18(1): p. 200.
Ratkevicius, A., A. Joyson, I. Selmer, et al., Serum concentrations of myostatin and myostatin-interacting proteins do not differ between young and sarcopenic elderly men. J Gerontol A Biol Sci Med Sci, 2011;66(6): p. 620–6.
Roubenoff, R., H. Parise, H.A. Payette, et al., Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham Heart Study. Am J Med, 2003;115(6): p. 429–35.
Doi, T., H. Makizako, K. Tsutsumimoto, et al., Association between Insulin-Like Growth Factor-1 and Frailty among Older Adults. J Nutr Health Aging, 2018;22(1): p. 68–72.
Doi, T., H. Shimada, H. Makizako, et al., Insulin-Like Growth Factor-1 Related to Disability Among Older Adults. J Gerontol A Biol Sci Med Sci, 2016;71(6): p. 797–802.
Harris, T.B., D. Kiel, R. Roubenoff, et al., Association of insulin-like growth factor-I with body composition, weight history, and past health behaviors in the very old: the Framingham Heart Study. J Am Geriatr Soc, 1997;45(2): p. 133–9.
Bergen, H.R., 3rd, J.N. Farr, P.M. Vanderboom, et al., Myostatin as a mediator of sarcopenia versus homeostatic regulator of muscle mass: insights using a new mass spectrometry-based assay. Skelet Muscle, 2015;5: p. 21.
Tay, L., Y.Y. Ding, B.P. Leung, et al., Sex-specific differences in risk factors for sarcopenia amongst community-dwelling older adults. Age (Dordr), 2015;37(6): p. 121.
Taekema, D.G., C.H. Ling, G.J. Blauw, et al., Circulating levels of IGF1 are associated with muscle strength in middle-aged- and oldest-old women. Eur J Endocrinol, 2011;164(2): p. 189–96.
Calvani, R., F. Marini, M. Cesari, et al., Biomarkers for physical frailty and sarcopenia: state of the science and future developments. J Cachexia Sarcopenia Muscle, 2015;6(4): p. 278–86.
Sahadevan, S., P.P. Lim, N.J. Tan, et al., Diagnostic performance of two mental status tests in the older chinese: influence of education and age on cut-off values. Int J Geriatr Psychiatry, 2000;15(3): p. 234–41.
Chan, M., Y.P. Lim, A. Ernest, et al., Nutritional assessment in an Asian nursing home and its association with mortality. J Nutr Health Aging, 2010;14(1): p. 23–8.
Mahoney, F.I. and D.W. Barthel, Functional Evaluation: The Barthel Index. Md State Med J, 1965. 14: p. 61–5.
Lawton, M.P. and E.M. Brody, Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 1969;9(3): p. 179–86.
Schafer, M.J., E.J. Atkinson, P.M. Vanderboom, et al., Quantification of GDF11 and Myostatin in Human Aging and Cardiovascular Disease. Cell Metab, 2016;23(6): p. 1207–1215.
Chen, L.K., L.K. Liu, J. Woo, et al., Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc, 2014;15(2): p. 95–101.
Schuling, J., R. de Haan, M. Limburg, et al., The Frenchay Activities Index. Assessment of functional status in stroke patients. Stroke, 1993;24(8): p. 1173–7.
Anderson, S.B., A.L. Goldberg, and M. Whitman, Identification of a novel pool of extracellular pro-myostatin in skeletal muscle. J Biol Chem, 2008;283(11): p. 7027–35.
Pirruccello-Straub, M., J. Jackson, S. Wawersik, et al., Blocking extracellular activation of myostatin as a strategy for treating muscle wasting. Sci Rep, 2018;8(1): p. 2292.
White, T.A. and N.K. LeBrasseur, Myostatin and sarcopenia: opportunities and challenges - a mini-review. Gerontology, 2014;60(4): p. 289–93.
Kim, J.K., S.R. Choi, M.J. Choi, et al., Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr, 2014;33(1): p. 64–8.
Garcia-Fontana, B., R. Reyes-Garcia, S. Morales-Santana, et al., Relationship between myostatin and irisin in type 2 diabetes mellitus: a compensatory mechanism to an unfavourable metabolic state? Endocrine, 2016;52(1): p. 54–62.
Zugel, M., S. Qiu, R. Laszlo, et al., The role of sex, adiposity, and gonadectomy in the regulation of irisin secretion. Endocrine, 2016;54(1): p. 101–110.
Stitt, T.N., D. Drujan, B.A. Clarke, et al., The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors. Mol Cell, 2004;14(3): p. 395–403.
Cruz-Jentoft, A.J., G. Bahat, J. Bauer, et al., Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing, 2019;48(1): p. 16–31.
Woodhouse, L., R. Gandhi, S.J. Warden, et al., A Phase 2 Randomized Study Investigating the Efficacy and Safety of Myostatin Antibody LY2495655 versus Placebo in Patients Undergoing Elective Total Hip Arthroplasty. J Frailty Aging, 2016;5(1): p. 62–70.
Cawthon, P.M., E.S. Orwoll, K.E. Peters, et al., Strong Relation between Muscle Mass Determined by D3-creatine Dilution, Physical Performance and Incidence of Falls and Mobility Limitations in a Prospective Cohort of Older Men. J Gerontol A Biol Sci Med Sci, 2018.
Dent, E., J.E. Morley, A.J. Cruz-Jentoft, et al., International Clinical Practice Guidelines for Sarcopenia (ICFSR): Screening, Diagnosis and Management. J Nutr Health Aging, 2018;22(10): p. 1148–1161.
Acknowledgements
We would like to thank all participants who contributed to this study. This study was supported by the Lee Foundation Grant 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards: Ethics approval for the study was obtained from by the Domain Specific Review Board of the National Healthcare Group and informed written consent was obtained from the participants.
Conflict of interest: The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Chew, J., Tay, L., Lim, J.P. et al. Serum Myostatin and IGF-1 as Gender-Specific Biomarkers of Frailty and Low Muscle Mass in Community-Dwelling Older Adults. J Nutr Health Aging 23, 979–986 (2019). https://doi.org/10.1007/s12603-019-1255-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1255-1