Abstract
Objective
-
(1)
To establish appropriate FRAIL-NH cutoff points in nursing homes in Mainland China;
-
(2)
To compare the FRAIL-NH scale and Frailty Index in assessing frailty prevalence and associated factors in nursing homes.
Design
A cross-sectional study.
Setting
Six nursing homes in Changsha, China.
Participants
A total of 302 residents aged 60 years or older (mean aged 82.71±8.49, 71.2% female).
Measurements
Frailty was assessed using the 34-item Frailty Index and the FRAIL-NH scale.
Results
The appropriate FRAIL-NH cutoff points to classify frail status and frailest status were 1.5 (87.6% sensitivity, 63.3% specificity) and 7.5 (94.1% sensitivity, 73.4% specificity), respectively. Based on the FRAIL-NH and Frailty Index, 69.5% (48% for frail and 21.5% for frailest), and 66.5% (60.9% for frail and 5.6% for frailest) of residents were at risk of frailty, respectively. There was no statistically significant difference in the total frailty prevalence assessed by FRAIL-NH and Frailty Index (χ2=0.617, P=0.432). The FRAIL-NH Scale is significantly associated with the Frailty Index (correlation coefficient (r) = 0.74, P < 0.001), but there was a Kappa agreement of 0.39 for frailty classification between the FRAIL-NH and Frailty Index, with the Frailty Index classifying a larger number of individuals as frail. When using FRAIL-NH scale, disease and self-reported health status were associated with frail and frailest status while age was just associated with frailest status. regarding the Frailty Index, age, diseases, medications and self-reported health status were associated with frail and frailest status.
Conclusion
The FRAIL-NH is a simple and effective tool to assess the overall frailty rate in nursing homes, and the Frailty Index may be more suitable capturing the multidimensionality of frailty at an individual level. Careful consideration in the selection of a frailty instrument, based on the intended purpose, is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is an important issue in global health aging, which is characterized by a decrease in physiological reserves and an increase of vulnerability to stressors, resulting in a greater chance of adverse health outcomes such as falls, disability, hospitalization and death (1, 2). Frailty is highly prevalent among nursing home residents and has been an important indicator for nursing home placement (2, 3). Early identification of frail individuals in nursing homes can help older adults adopt timely and appropriate interventions to prevent or delay further disability and reduce health care costs. It is particularly important to nursing homes in China because nursing homes play a significant role in long-term care due to its increasing aging population and one-child policy (4). However, frailty has been underinvestigated in nursing home settings in China as assessment tool for frailty is lacking (5, 6). Research showed frailty assessment in nursing home residents differs from community-dwelling older adults (7–9). A frailty tool specific for Chinese nursing home residents is urgently needed.
The Physical Frailty Phenotype (PFF) and Frailty Index (FI) are the most commonly used frailty instruments in nursing home-related research (2). However, there are limitations in using these instruments to assess frailty in nursing homes. For example, the FI can be constructed from routinely recorded clinical data in nursing homes, but it is not brief enough to be used as a screening tool, especially when facilities do not use electronic health records (10). Although the PFF is widely recognized, it contains objective measurement indicators, such as walking speed or duration of physical activity. These indicators may be inappropriate because a substantial proportion of nursing home residents already experience dependencies (7) and there are realistic conditions and time limit (11). Other frailty instruments (e.g. Edmonton Frail Scale (12), Clinical Frailty Scale (13)) are developed for community-dwelling adults and/or hospitalized populations and may be less applicable to nursing home residents.
FRAIL-NH, adapted from the FRAIL by Kaehr et al., overcomes the limitations of the PFF and FI for the nursing home population and is a simple and easy-to-use frailty instrument specific to nursing home residents (10, 14, 15). FRAIL-NH is a combination of the initials of seven items (Fatigue, Resistance, Ambulation, Incontinence/Illness, Loss of weight, Nutritional approach, Help with dressing) (14) and includes core characteristics of the PFF and FI classification systems (15), which has been validated in different populations and countries (8, 10, 11, 15). However, to our knowledge, FRAIL-NH has never been used in Mainland China before.
Heterogeneity of frailty prevalence assessed by FRAIL-NH has been found due to different cutoff points. The original FRAIL-NH study used a score of 7 as the frailty cutoff point (14), but this may underestimate the frailty prevalence in nursing homes (10). Theou et al. showed that appropriate FRAIL-NH cutoff points classifying frailty and severe frailty were 2 and 6 in Australian long term care residents, with 37.5% of residents categorized as frail and 35.9% as frailest(10). Kaehr et al. used cutoff points of 6 and 8 in FRAIL-NH to identify pre-frail and frail residents living in long-term care facilities in the U.S. and showed a frailty prevalence of 48.7% (15). It is well known that the scales’ cutoff points are different across regions and populations (16). To our knowledge, no studies have reported an appropriate cutoff point of the FRAIL-NH scale among nursing home residents in Mainland China. The prevalence of frailty screened using FRAIL-NH in nursing homes in Mainland China has been unknown, and little information is available comparing the use of the FRAIL-NH and FI to explore associated factors of frailty in nursing homes. Therefore, the purpose of this study is to establish appropriate FRAIL-NH cutoff points and compare the FRAIL-NH scale and Frailty Index (FI) in assessing frailty prevalence and associated factors among nursing home older adults in mainland China.
Methods
Study design and population
Between July and August 2018, we conducted a crosssectional study in six nursing homes in Changsha which is a middle size provincial city with a population of eight million in central region of China. Changsha was particularly chosen for this study because of its representation in aging characteristic and physical condition of elderly people in china. Subjects were eligible for this study if they had lived in the selected nursing homes for at least 30 days at the beginning of the study, and were medically stable and able to communicate with others. Individuals who refused to participate or did not sign the informed consent were excluded. A total of 320 individuals were enrolled and 18 were excluded from the current analysis due to missing values on more than 20% of the variables.
Two student nurses administered a series of validated and widely used scales. Student nurses underwent training at a centralized location in the standard administration of the study assessment tools. All participants (or their legal representative, for those who lacked decision-making capabilities) signed the informed consent form. The study protocol was approved by the nursing and behavioral medicine research ethics committee of blinded for peer review.
Measurements of frailty and study covariates
FRAIL-NH
The FRAIL-NH includes seven items (fatigue, resistance, ambulation, incontinence, weight loss, nutritional approach, and help with dressing) (14). The range of possible total scores is between 0 and 14 (from the best to worst state). A complete description of the FRAIL-NH items is provided in Appendix 1.
Frailty Index
FI is a count of impairments and illnesses, collectively known as deficits(13). Each deficit included in the FI was coded (0 or 1 indicating absence or presence, respectively). At least 30 age-related health deficits should be included to calculate FI(17). We developed a 34-item FI based on a standard methodology (Appendix 1). The FI score of each participant was defined as the ratio between the existing deficits and the number of evaluated deficits. Thus, the FI ranged from 0–1 (no deficit present, to all deficits present) and are categorized as non-frail (0–0.10), vulnerable (0.10–0.21), frail (0.22–0.44), and frailest ( ≥ 0.45) (10, 11, 18). In this study, we have grouped non-frail and vulnerable categories to conduct three level of frailty.
Other measures
Sociodemographic data were collected (age, sex, education level and marital status). The education level was categorized into three groups (uneducated / primary, secondary, and university). Marital status was categorized into two groups (never married / widowed / divorced, and married). The Mini- Nutritional Assessment scale, the validated Chinese version of the Mini-Mental State Examination and the Chinese version of the Patient Health Questionnaire (PHQ-9) scale were applied to determine nutritional status, cognitive function and depression, respectively. Multimorbidity was defined as having two or more diseases(19).
Statistical Analysis
Data were analyzed using IBM SPSS Statistics version 18.0 (IBM Corp., Armonk, NY). Descriptive statistics were reported as means ± standard deviations (SD) or percentages. Pearson correlation analyses were used to investigate the association between the two tools. Receiver operating characteristic (ROC) curves were used to establish cutoff points for the FRAIL-NH scale, using the FI for comparison. Chi-square test was used to compare participant characteristics of the nonfrail, frail, and frailest groups. Agreement between the two tools was measured using the kappa statistic. Univariate and multivariate logistic regression analyses were used to examine the association between individual characteristics and frailty. A 95% confidence interval (CI) was reported, and the level of statistical significance was set at P < 0.05.
Results
A total of 302 individuals (mean age 82.71±8.49, range 60–100, 71.2% female) were included in this study (Table 1). The mean FI score was 0.27±0.11 (range 0–0.59), and the mean FRAIL-NH scale score was 4.11±3.65 (range 0–14). The FRAIL-NH scale was significantly associated with the FI (r=0.74, P <0.001).
In predicting frail and frailest residents based on the FI, ROC curve analysis showed that the area under the curve for the FRAIL-NH was 0.86 (95% CI = 0.82–0.90, P<0.001) for frail and 0.89 (95% CI = 0.84–0.95, P<0.001) for the frailest residents. The FRAIL-NH scores in classifying frailty and severe frailty based on the FI were 1.5 (87.6% sensitivity, 63.3% specificity) and 7.5 (94.1% sensitivity, 73.4% specificity), respectively. Based on FRAIL-NH, 69.5% of residents were considered at risk of frailty, with 48% classified as frail and 21.5% as frailest. Based on the FI, 66.5% were considered at risk of frailty, with 60.9% classified as frail and 5.6% as frailest. There was no statistical difference in the total frailty prevalence assessed by FRAIL-NH and FI (χ2=0.617, P=0.432).
The proportion of frail and frailest individuals assessing by FRAIL-NH and FI is presented in Table 2. The kappa statistic for agreement between the FRAIL-NH and FI classifying individuals was 0.392 (SE = 0.045, P < 0.001). Of participants who were classified as non-frail by the FRAIL-NH scale, 27.2% were classified as frail by the FI.
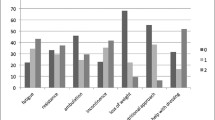
Table 3 displays participants’ demographics and health characteristics according to frailty category per screening measure. A significantly higher percentage of multimorbidity and poor self-reported health status were found in the frailest category for both measures. A larger number of those categorized as frailest are residents aged 80 and older. It appears a larger percentage of those who live with others are classified in the frailest group, according to the FI.
Table 4 and Table 5 show the results of univariate and multivariate analysis where frailty status was classified as non-frail, frail and frailest using the FRAIL-NH and FI. In multivariate analysis, multimorbidity and poor self-reported health were significantly associated with an increased risk of frail and frailest status according to both measures. Being older was associated with an increased rate risk of a FI classification of frail or frailest, but was only associated with a FRAIL-NH classification of frailest. Living alone was a significant factor associated with a decreased risk of frail status, whereas the same significant association was not shown in the frailest category.
Discussion
Assessing frailty and exploring its associated factors are useful for long-term care providers to implement appropriate and personalized interventions in nursing homes where frailty is highly prevalent. This study established FRAILNH cutoff points using the FI as a comparison. There was some heterogeneity in frailty prevalence and associated factors according to both measures due to differences in the frailty conception and theory model of two instruments.
This study shows that the prevalence of frailty ranged from 48% using FRAIL-NH, to 60.9% using the FI, which is consistent with previous studies conducted in other countries(10, 15). The prevalence of frailest status ranged from 5.6% using the FI, to 21.5% using FRAIL-NH, which is substantially lower than in other studies (FI: 24.4%-71.8 %, FRAIL-NH:35.9%-54.2%)(7, 10, 11). In those studies, residents tended to be older (87.5±6.2, 86.3±7.3), which was likely to have contributed to the higher prevalence of the frailest category. In addition, those studies adopted a FRAIL-NH cutoff point of 6 (lower than 7.5 in our study) to categorize frail status with frailest status, leading to higher prevalence of the frailest category.
We found a strong significant correlation between FRAILNH and FI scores (r = 0.743, P < 0.001). This finding is expected, as many of the FRAIL-NH variables are included in the FI. However, there was only a modest kappa score of 0.392 between these two tools in their ability to classify non-frail, frail or frailest individuals, with the FI classifying a larger number of participants as frail. This is probably because these two tools were developed based on different models (the cumulative deficits model for FI (20) and the combination of functional, deficit accumulation and biological frailty models for FRAILNH( 14, 21, 22)), and the assessment items and conceptual underpinnings differ from each other. The heterogeneity of the theory model and frailty operational conceptualizations may be important reasons for the only modest agreement(11, 23). This study showed heterogeneous results of frailty prevalence and associated factors in the same sample, which suggests that careful consideration in selecting a frailty tool is important in frailty-related clinical and research settings. Our results showed that the FI classified a larger number of individuals as frail. Of note, 27.2 % of individuals classified as non-frail by the FRAIL-NH were classified as frail by the FI. Through further statistical analysis, we found that these individuals had significantly higher rates of multimorbidity compared to those classified as non-frail according to both measures. This result suggests that as a frailty tool, the FI may be more suitable than FRAIL-NH for capturing the multidimensionality of frailty at the individual level for factors such as multiorbidities and multiple medications. In addition, there is no significant difference in the total frailty prevalence by these two tools, which suggests that FRAIL-NH may be a better tool than the FI to assess the overall frailty rate in nursing homes. Furthermore, FRAIL-NH is shorter and relies on fewer items, making data less cumbersome to collect, compared to the FI(15).
The study population in FRAIL-NH and FI showed a significant increase in frailest status in terms of multimorbidity and poor self-reported health. A larger number of those categorized as frailest are residents aged 80 and older, because frailty level increases significantly with age(24). In this study, the FI finding shows that the older adults who live with others have a significantly higher chance of being categorized as frailest, compared to older adults who live alone, which is inconsistent with other studies(25). Frailest status reflects a worse degree of psychophysical well-being and increased dependence(26). It is likely that older adults who are frailest are typically placed in a group living arrangement by care providers, in order to provide centralized service and economize on health resources.
Multivariate analysis identified that multimorbidity was significantly associated with an increased risk of frail and frailest status in both the FRAIL-NH and FI. Previous studies have shown that multimorbidity was also a significant factor for PFF and FI(25). This suggests that multimorbidity could be identified as a significant contributor to the development of frailty, regardless which tools are used for assessment. Poor self-reported health has previously been identified as a significant contributor associated with frail status and frailest status measured by PFF among community-dwelling older adults(27), which is consistent with our findings. According to the frailty identity crisis theory, older adults can perceive changes in their physical and mental functioning along with the process of their transition from self-care to loss of self-care ability(28). The worse the self-perceived health condition is, the more likely a person is to adopt negative behaviors, which could lead to a deterioration in health(28). In the FI, living alone was significantly associated with a decreased risk of frail status, and this is consistent with a previous study(26) that living alone had associated with frailty transitions. However, the same significant relationship was not shown in residents with frailest status, probably because the frailest status may be difficult to reverse.
To the best of our knowledge, this is the first study to use the FRAIL-NH in nursing homes in Mainland China. The main strength of this study was to measure frailty using both the FRAIL-NH and the FI. Moreover, participants with poor mobility and physical conditions were also included in this study. However, residents who were medically unstable were excluded from participation, which meant that frailty levels were underestimated. Only residents living in large-scale nursing homes in Changsha were investigated, due to the limited research conditions, which might affect the generalizability to all nursing home residents in China. Additionally, because of the difficulties involved in randomly selecting a sample, a convenience sampling was used in this study, which may limit the representativeness.
In conclusion, we established appropriate cutoff points for FRAIL-NH based on the FI, and investigated frailty prevalence nursing home residents in Changsha, China. There was only a modest agreement between the measures in classifying individuals as non-frail, frail or frailest, with the FI classifying a greater number of individuals as frail, and the choice of tool possibly impacting the accurate identification of frailty. The FI may be more suitable for capturing the multidimensionality of frailty at an individual level than the FRAIL-NH, which can be used to explore associated factors for frailty in order to identify intervention strategies. FRAIL-NH may be a simpler tool to assess the overall frailty rate in nursing homes than the FI, which can be widely used to understand the frail status of nursing home residents. Therefore, careful consideration in the selection of a frailty instrument, based on the intended purpose, is necessary.
Acknowledgements: The authors wish to thank student nurses, nursing home administrators and residents for their valuable support and partcipation. Besides, we thank Brain Buta, MHS for providing feedback on our manuscript draft.
Fundings: This project was supported by Summer Health Research Fellowship of Xiangya Overseas Alumni Association Yale-China Association (Grant 2018-XYOAA-1).
Conflict of interest statement: The authors declare no conflicts of interests.
Ethical standards: The study complies with the current laws of the country in which it was performed.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381:752–762.
Kojima G. Prevalence of frailty in nursing homes: a systematic review and metaanalysis. J Am Med Dir Assoc 2015; 16:940–945.
Kojima G. Frailty as a predictor of nursing home placement among community-dwelling older adults: a systematic review and meta–analysis. J Geriatr Phys Ther 2016; 41:1–7.
Li X, Fan L, Leng SX. The aging tsunami and senior healthcare development in China. J Am Geriatr Soc 2018; 66:1462–1468.
Zhao Y–Y, ·Li XW, Ding YP, Cui Y. Comparison of predictive power for disability among institutional older adults using Tilburg scale and frality phenotype. Chinese J Heal Stat 2017; 34:436–438.
Ma L, Tang Z, Zhang L, Sun F, Yun Li, Piu Chan. Prevalence of frailty and associated factors in the community–dwelling population of China. J Am Geriatr Soc 2017; 66:559–564.
Silva TR De, Theou O, Vellas B, Cesari M, Visvanathan R. Frailty screening (FRAILNH) and mortality in french nursing homes: results from the incidence of pneumonia and related consequences in nursing home residents study. J Am Med Dir Assoc 2018; 19:411–414.
Luo H, Lum TY, Wong GH, Kwan JS, Tang JY, Chi I. Predicting adverse health outcomes in nursing homes: a 9–year longitudinal study and development of the FRAIL–Minimum Data Set (MDS) quick screening tool. J Am Med Dir Assoc 2015; 16:1042–1047.
Chan TC, Shea YF, Luk KH, Chan HW, Chu L. Development and validation of a prognostic index for 2–year mortality in Chinese older residents living in nursing homes. Geriatr Gerontol Int 2012; 12:555–562.
Theou O, Tan ECK, Bell JS, et al. Frailty levels in residential aged care facilities measured using the frailty index and FRAIL–NH scale. J Am Geriatr Soc 2016; 64:e207–e212.
Martínez–Velilla N, Herce PA, Herrero ÁC, et al. Heterogeneity of different tools for detecting the prevalence of frailty in nursing homes: feasibility and meaning of different approaches. J Am Med Dir Assoc 2017; 18:898.e1–898.e8.
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton frail scale. Age Ageing 2006; 35:526–529.
Rockwood K, Song X, Macknight C, et al. A global clinical measure of fitness and frailty in elderly people. C Can Med Assoc J 2005; 173:489–495.
Kaehr E, Visvanathan R, Malmstrom TK, Morley JE. Frailty in nursing homes: the FRAIL–NH scale. J Am Med Dir Assoc 2015; 16:87–89.
Kaehr EW, Pape LC, Malmstrom TK, Morley JE. FRAIL–NH predicts outcomes in long term care. J Nutr Heal Aging 2016; 20:192–198.
Wei Z–Z, Wang WL. The cutoff point of POSM–SF questionnaire to define preoperative negative mood disorders in patients undergoing gastric cancer radical surgery. Chinese J Nurs 2011; 46:169–171.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. Bmc Geriatr 2008; 24:1–10.
Hoover M, Rotermann M, Sanmartin C, Bernier J. Validation of an index to estimate the prevalence of frailty among community–dwelling seniors. Heal Reports 2013; 24:10–17.
Vetrano DL, Palmer K, Marengoni A, et al. Frailty and multimorbidity: a systematic review and meta–analysis. Journals Gerontol 2018(in press).
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007; 62:722–727.
Malmstrom TK, Miller DK, Morley JE, Louis S, Louis S, Louis S. A comparison of four frailty models. 2015; 62:721–726.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Heal Aging 2012; 16:601–608.
Buta BJ, Walston JD, Godino JG, et al. Frailty assessment instruments: identification and systematic characterization of the uses and contexts of highly–cited instruments. Ageing Res Rev 2016; 26:53–61.
Theou O, Brothers TD, Peña FG, Mitnitski A, Rockwood K. Identifying common characteristics of frailty across seven scales. J Am Geriatr Soc 2014; 62:901–906.
Thompson MQ, Theou O, Yu S, Adams RJ, Tucker GR, Visvanathan R. Frailty prevalence and factors associated with the frailty phenotype and frailty index: findings from the North West Adelaide Health Study. Australas J Ageing 2017; 37:120–126.
Trevisan C, Veronese N, Maggi S, et al. Factors influencing transitions between frailty states in elderly adults: the Progetto Veneto Anziani Longitudinal Study. J Am Geriatr Soc 2017; 65:179–184.
Xi X, Guo GF, Sun J. Elderly frailty assessment tools and their applications. Chinese J Gerontol 2015; 35:5993–5996.
Howard Fillit MD, Butler RN. The frailty identity crisis. J Am Geriatr Soc 2010; 57:348–352.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ge, F., Liu, M., Tang, S. et al. Assessing Frailty in Chinese Nursing Home Older Adults: A Comparison between the Frail-NH Scale and Frailty Index. J Nutr Health Aging 23, 291–298 (2019). https://doi.org/10.1007/s12603-019-1156-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1156-3