Abstract
Objectives
In China, few studies reported the disability situation and the association between disabilities with chronic conditions in aged people. This study investigates the cross-sectional trends of prevalence and severity of activities of daily living disability (ADL) in Chinese oldest-old people from 1998 to 2008, and identified the potential risk factors of disability.
Design
A combination of population-based longitudinal prospective study and probabilistically sampling cross-sectional studies.
Setting
The Chinese Longitudinal Healthy Longevity Survey (CLHLS) was based on a random sampling of aged people from twenty-two provinces in China.
Participants
A total of 52,667 participants aged from 80 years old to 105 years old sampled in the year of 1998 (n=8,768), 2000 (n=10,940), 2002 (n=10,905), 2005 (n=10,396) and 2008 (n=11,658) were analyzed respectively.
Results
The prevalence of ADL disability decreased from the year of 1998 (18%) to 2008 (12%). The disability prevalence significantly increased in 2002 and decreased in 2008 (P<0.001) in total participants than the year of 1998. The prevalence trends of low ADL disability level were almost identical with that of the total ADL disability. Stroke/cerebrovascular disease (CVD) and cognitive impairment were the strongest risk factors of disability. Vision impairment became less associated with ADL disability (P=0.045), while the association between multimorbidity and ADL disability became stronger (P=0.033).
Conclusions
The prevalence of ADL disability declined among the oldest-old population in China from the year of 1998 to 2008 without obeying a linear pattern. Temporal trends of ADL disability mainly attributed to the change of low disability level prevalence. Stroke/CVD and cognitive impairment were the most common risk factors of disability. Vision impairment caused disability has become less common, while risks of multimorbidity related disability increased.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
China has substantial proportion of aged population (1) and is facing the challenge of rapid aging (2), which is because of the declines in fertility and increases in life expectancy (3). Moreover, China also has the largest number the oldest-old population aged more than 80 years old in the world, and the amount is still rapidly growing (1). Physical limitation prevalence increases with age, especially in people aged more than 80 years old (4-6), because disability onset is postponed in late life due to the improvement of quality of life (7).
Studies on temporal trend in prevalence of late-life ADL disability have been carried in many developed countries. In the U.S., the prevalence of ADL disability declined during the middle and late of 1990s and flatted through 2000s among people aged 65 years and more (8, 9), whereas, in Australia and Japan, ADL disability prevalence increased during the period of 1990s (10). In addition, there were mixed time trends of prevalence in ADL disability in European countries in the past 30 years (11-13). Obviously, most studies of disability trends tended to focus on younger aged population due to the difficulties in recruiting people at older age (14). In China, limited reports about change in disability trend over time of the aged population at national level (15, 16) came out. Furthermore, nearly none of the studies focused on the older elderly as data in this age group are scarce (17).
Late-life functional disability is associated chronic conditions (18-22). However, there are still knowledgeable gaps about whether, and to what extent, these factors works in the people aged 80 years old or older, since almost all the current studies in aging had limited power to evaluate the risk factors appropriately and sufficiently (23).
The oldest-old have the highest risk of disability, which causes big economic and social burden (24), especially in China, when it is facing the rapid aging challenge in the coming decades. It is therefore crucial and urgent to examine the trend of prevalence in disability and the potential factors in Chinese oldest-old people, in order to provide scientific evidence for health-care policy.
A previous study has just reported the overall prevalence in ADL disability declined from 1998 to 2008 using CLHLS data (25). However, the prevalence trend varies among different groups. Analyzing and reporting these trends are necessary and important for government to make policy decision. In our study, we will present the ADL disability prevalence more comprehensively and detailed in multiple dimensions (gender, age group, region, and living situation).
The aim of this study is to (a) investigate the time trend of prevalence in ADL disability among people aged 80 years or older in Mainland China from 1998 to 2008 stratified by age group, gender, region and living situation, respectively, and (b) to explore the association of chronic conditions with the ADL disability in these people.
Methods
Data
The study was based on the Chinese Longitudinal Healthy Longevity Survey (CLHLS), which is the first nationally longitudinal survey on determinants of health aging of the largest sample of oldest-old individuals in China. Details of the survey design have been described before and data quality was reported to be generally good (23). Briefly, the CLHLS was based on a randomly selected sample of elderly people from 22 of 31 provinces in China, and the sampling frame covered about 85% of the total population and represented eastern area, central area, and western area of China. The survey was firstly launched in 1998, and then followed in 2000, 2002, 2005, 2008 and 2011. At each follow-up wave, surviving participants were tracked, and new participants with the same age, gender, and residence were recruited to make up for attrition from loss of follow-up or death. With this sampling strategy, 52.9%, 22.6%, 12.1%, 7.5% and 4.9% participated in 1, 2, 3, 4 and all 5 waves of the survey, respectively. Cross-sectional weights were calculated on the basis of the age-gender-region distribution of the older population to generate nationally representative estimates. The CLHLS study was approved by the research ethnics committees at Duke University and Peking University.
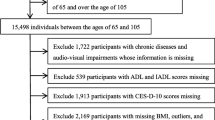
Study participants
The present study focused on 52,667 participants aged 80 years to 105 years old in the waves of 1998 (n=8,768), 2000(10,940), 2002(n=10,905), 2005(n=10,396), 2008(n=11,658), respectively. The participants older than 105 years old were not included because of unreliability in age reporting (26). The wave of 2011 was excluded in this study because it just followed included participants without updating recruitment, which was not consistent of sampling design. We regarded the prevalence of ADL disability in 2011 not comparable with others. Written informed consent was obtained from every participant or a proxy.
Data collection and definitions
The survey was administered in the participants’ homes by trained interviewers from the local centers of disease prevention and control for undergraduates.
ADL was measured by participant’s self-reported results in six self-care tasks consisting of bathing, dressing, eating, indoor transferring, toileting, and continence based on the Katz index scale (27). Disability was defined as a need for assistance or a difficulty in one or more activities of the six items (28, 29).
Low-level disability was defined as study participants needed for assistance in 1 to 4 ADL items; and high-level disability was defined as study participants needed for assistance in 5 to 6 ADL items (30).
In this analysis, the independent variables are classified as socio-demographics, lifestyle and chronic conditions. Socio-demographics include age, gender, region (urban/rural), living situation (community/institution), marital status (currently married/ divorced, widowed, never married), and education length (0 year/1-6 years/7+ years of schooling). Lifestyle includes ever smoking (yes/no), ever drinking (yes/no), physical exercise (e.g. walking, running, dancing) (yes/no). Chronic conditions include cognitive impairment (yes/no), and self-reported hypertension (yes/no/uncertainty), diabetes mellitus (yes/no/uncertainty), heart disease (yes/no/uncertainty), respiratory disease (yes/no/uncertainty), stroke/cerebrovascular disease (CVD) (yes/no/uncertainty), vision impairment (yes/no/uncertainty), and Parkinson’s disease (yes/no/uncertainty). Cognitive impairment was assessed by the Chinese version of the Mini-Mental State Examination, which score ranges from 0 to 30, and the score <18 was defined as cognitive impairment (31). The simultaneous presence of two or more chronic conditions above was defined as multimorbidity.
Statistical analysis
Descriptive analyses were performed for distribution of baseline characteristics of the study participants across 5 survey time points. The temporal trends in prevalence of ADL disability were assessed using generalized estimating equation (GEE) models with a logistic link and binominal distribution in order to address the correlation of repeated measurements within the same participants in waves. The odds ratio and 95% confidence interval of ADL disability were estimated in each time point of the year of 2000, 2002, 2005 and 2008, compared with time point the year of 1998 as referent, after adjusting for age, gender, region or living situation. The time trends in ADL disability severity were also performed by GEE models. The association of ADL disability with chronic condition factors was tested in model1-4 adjusting for incremental covariates. In model 5, the time trend in the strength of associations between ADL disability and chronic conditions was conducted with the interaction term of ADL disability and each chronic condition and multimorbidity. These analyses were also conducted by GEE models. Although the weight which was derived from the corresponding Chinese census or mini-census was constructed based on age-gender-region distribution of the older population, multivariate analyses were not weighted as a result of adjusting for age, gender and region variables as covariates in all models, which is a common and acceptable approach (32).
Sensitive analyses were conducted for association between ADL disability and chronic conditions, where missing data and chronic conditions data coded “uncertainty” were imputed using multiple imputation methods (33). For all analyses, P value <0.05 was considered as statistically significant. SAS (Version 9.2; SAS Institute Inc., Cary, North Carolina, USA) was used for modeling analyses and statistical tests.
Results
Characteristics of study participants
Table 1 presents the distribution of descriptive characteristics of the study participants across five waves. In sociodemographics, the participants’ mean age was 92 years old, the proportion of female, urban residence, community dwelling, currently married and being educated were 60%, 47%, 95%, 18% and 32%, respectively. The means or distributions of all the above factors were nearly consistent or not clinically significant difference across all five surveys.
Trend in prevalence of ADL disability
Figure 1 shows weighted prevalence (weight based on age-gender-region distribution derived from the corresponding Chinese census or mini-census) of ADL disability in total study participants and in subgroups including age, gender, region and living situation groups. Overall, ADL disability prevalence increased from 18% in 1998 to 22% in 2002, and then decreased to 12% in 2008. In addition, risks of having higher ADL scores increased as age increased, living in urban, being female and in institution in each wave of survey.
Table 2 presents the GEE models results of trends in ADL disability from the year of 1998 to 2008 after adjusting for age, gender, region and living situation. Compared with the year of 1998, ADL disability prevalence was 21% (P<0.001) higher odds in 2002, and had 34% (P<0.001) lower odds in 2008 respectively in total sample. The similar trends in ADL disability were also in all subgroups, except for institutionalized older adults.
Trend in severity of ADL disability
Table 3 demonstrates the adjusted trends of ADL disability severity stratified by low level and high level from 1998 to 2008 after adjusting for age, gender, region and living situation. Compared with prevalence of low ADL level in 1998 in total sample, 21% (P<0.001) odds ratio increased in 2002, and 14% (P<0.001) in 2005 and 32% (P<0.001) in 2008 decreased. At the meantime, the trend in prevalence of high ADL level flatted among 1998 to 2005 (P=0.128-0.263), and decreased in 2008 (P<0.001).
Association between ADL disability and chronic conditions
Table 4 lists the association of ADL disability with each chronic condition and multimorbidity. The association of stroke/CVD (OR=3.37-4.95) and cognitive impairment (OR=3.22-5.03) with ADL disability were of the highest. Hypertension was not related to ADL disability in all models. Vision impairment became less associated with ADL disability decreased (OR=0.82, P=0.045), while the association between multimorbidity and ADL disability became stronger (OR=1.21, P=0.033)
Sensitive analyses
The result of multiple-imputation analyses for the association of ADL disability with chronic conditions were similar with the main analyses, (see supplementary Table S1).
Discussion
This study provided updated information in the trends of prevalence and in different levels of, and risk factors for functional disability in ADLs in the population aged 80 years old and elder in Mainland China. To analyze trends in prevalence and in severity of ADL disability, we just adjusted for basic variables (age, gender, region, and living situation) in order to reflect the real condition of disability (34).
It is difficult to make comparisons with other studies nationally and internationally, since most previous studies in ADL disability trends were based on younger-old people or without reporting the ADL disability trends in the age group of 80 years old and older specifically. The Medicare Current Beneficiary Survey (MCBS) in the U.S. found that ADL disability trend declined 0.71 percent per year in subgroup of 85 years old and older during 2000-2008 (9), and The China Health and Nutrition Survey (CHNS) in mainland China reported that the trend also declined 1.05 percent annually from 1997 to 2006 in subgroup aged 80 and over (16). Both prior studies reported a downtrend monotonically during the period, whereas, in our study, ADL prevalence increased and then decreased over time, and the year of 2002 was the turning point. Compared with the CHNS study, a possible explanation for this difference was that the survey time points were not the same. If we chose the time point as prior study, we would get the similar trend without identifying the turning point. The declining prevalence of ADL disability might be attributed to decreased incidence of and increased recovery from ADL disability (35). However, the exact reasons for the favorable trend of late-life ADL disability from 2002 are not fully understood. If this trend continued, the proportion of oldest-old people with ADL disability will decline continuously and the burden of geriatric care and elder social services might be alleviated. It is important to note that although odds of ADL disability decreased more in rural area (table 2), the absolute value of decline in ADL disability was bigger in urban area (figure 1) over time; because the prevalence rate in 1998 was much higher in urban than that in rural. Additionally, the disparities of ADL disability between genders also have dwindled among this period. It is possible that, as the urbanization in China, the difference between urban and rural had gradually diminished in many aspects such as lifestyle and socioeconomic status (36); female are easier to get economic income and medical service at present than in the past (18). All of these reasons might contribute to diminish of the gaps in ADL prevalence.
The trends of low level and high level of ADL disability were completely different in total participants. The high disability level was at a trend of slow and gradual decline over time, whereas the trend in low disability level rose and declined from the year of 1998 to 2008. It was noteworthy that the trends in ADL disability and in low disability level were extremely similar. That might mean the change of overall disability prevalence mainly resulted from the change of low disability level during this period. Furthermore, the improvements in both disability levels might be primarily attributed to developments of environment and improvements in assistive devices (30).
Chronic conditions have been confirmed as the main causes to disability (29), so identifying and preventing specific medical diseases that would lead to ADL disability is critical for reducing the burden of disability in Chinese oldest-old people. Our study suggested that cerebrovascular diseases and cognitive impairment were the main contributors to disability as reported in most previous reports (19-22). The results also implied that the strength of association between vision impairment and ADL disability was becoming weaker. It may because of the severity of disability induced by vision impairments got reduced by early diagnosis, enhanced risk managements, and appropriate medical treatment (37). In the contrary, disabling effects of multimorbidity rose in ADL disability, which is to opposite to CHNS study (16). The reason might be we selected different chronic conditions than other studies. In CHNS study, they just focused on multiple cardiometabolic diseases, but we chose more extensive chronic conditions besides cardiometabolic diseases.
This study has several strengths. To the best of our knowledge, the CLHLS has the nationally largest sample of the oldest old population in China Mainland. Unlike many other studies, this survey included both community-based and institutionalized persons that provided more extensive and completed information in ADL disability situation. Another strength is that the current study contained relatively more survey time point, which presented more accurate prevalence trends. In addition, the approaches of data collection and survey items in this study seldom changed over time. Nevertheless, this research also has limitations. First, the measures of chronic medical diseases and disability were based on self-reported methods, which might misestimate the prevalence and the associations of diseases with functional disability. Second, the association of some important chronic diseases such as arthritis and depression symptom, and the effects of severity of diseases on functional disability were not examined because of the limited data quality or the absence of specific information. Finally, the cause-effect relationships were not demonstrated for the association between diseases and ADL disability.
In conclusion, this study showed that the prevalence of ADL disability declined in Chinese adults aged 80 years old and elder from the year of 1998 to 2008, but not following linear trend. Moreover, the change of low disability level was the main contributor to the time trend of ADL disability during this period. The presence of Stroke/CVD and cognitive impairment were the greatest risk factors of disability in Chinese oldest-old people. In addition, vision impairment might cause less disability, while multimorbidity might cause more disability over time. Finally, these findings from this study could provide information to develop preventive strategies and specific interventions for the reduction of disability in Chinese oldest-old population.
Acknowledgments: Data used in this current study was supported by the NIA/NIH, China Natural and Social Sciences Foundations, the UNFPA and the RGU. We thank Professors Zeng Yi, Gu Danan (Duke University Center for Study of Aging and Human Development/Medical School and Peking University Center for Healthy Aging and Family Studies/China Center for Economic Research), and Liu Yuzhi (Center for Healthy Aging and Family Studies and Institute of Population Research, Peking University) to provide us with the data set.
Funding: This work was supported by The Program of Beijing municipal science & technology commission (D121100004912002); and Young core personal project & Beijing outstanding talent training project (Serial Number: 2014000020124G150).
Conflict of Interest: Authors declare no conflicts of interest.
Ethical standard: Each wave of the CLHLS was approved by the research ethics committees of Duke University and Peking University. Written informed consent was obtained from every participant or a proxy.
References
UN. World population Ageing 2013. UN.
The L. Ageing in China: a ticking bomb. Lancet. 2016;388:2058. doi:10.1016/S0140-6736(16)32058-X
Peng X. China’s demographic history and future challenges. Science. 2011;333:581–587. doi:10.1126/science.1209396
Diehr PH, Thielke SM, Newman AB, Hirsch C, Tracy R. Decline in health for older adults: five-year change in 13 key measures of standardized health. J Gerontol A Biol Sci Med Sci. 2013;68:1059–1067. doi:10.1093/gerona/glt038
McLaughlin SJ, Jette AM, Connell CM. An examination of healthy aging across a conceptual continuum: prevalence estimates, demographic patterns, and validity. J Gerontol A Biol Sci Med Sci. 2012;67:783–789. doi:10.1093/gerona/glr234
McLaughlin SJ, Connell CM, Heeringa SG, Li LW, Roberts JS. Successful aging in the United States: prevalence estimates from a national sample of older adults. J Gerontol B Psychol Sci Soc Sci. 2010;65B:216–226. doi:10.1093/geronb/gbp101
Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi:10.1056/nejm198007173030304
Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–3146. doi:10.1001/jama.288.24.3137
Freedman VA, Spillman BC, Andreski PM, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50:661–671. doi:10.1007/s13524-012-0167-z
Robin JM, Michel JP. Looking forward to a general theory on population aging. Tijdschr Gerontol Geriatr. 2006;37:209–217. doi:10.1007/BF03074801
Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208. doi:10.1016/S0140-6736(09)61460-4
Hoeymans N, Wong A, van Gool CH, et al. The disabling effect of diseases: a study on trends in diseases, activity limitations, and their interrelationships. Am J Public Health. 2012;102:163–170. doi:10.2105/AJPH.2011.300296
van Gool CH, Picavet HS, Deeg DJ, et al. Trends in activity limitations: the Dutch older population between 1990 and 2007. Int J Epidemiol. 2011;40:1056–1067. doi:10.1093/ije/dyr009
Berlau DJ, Corrada MM, Kawas C. The prevalence of disability in the oldest-old is high and continues to increase with age: findings from The 90+ Study. Int J Geriatr Psychiatry. 2009;24:1217–1225. doi:10.1002/gps.2248
Gu D, Dupre ME, Warner DF, Zeng Y. Changing health status and health expectancies among older adults in China: gender differences from 1992 to 2002. Soc Sci Med. 2009;68:2170–2179. doi:10.1016/j.socscimed.2009.03.031
Liang Y, Song A, Du S, Guralnik JM, Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997-2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci. 2015;70:739–745. doi:10.1093/gerona/glu204
Vaupel JW. Biodemography of human ageing. Nature. 2010;464:536–542. doi: 10.1038/nature08984
Feng Q, Zhen Z, Gu D, Wu B, Duncan PW, Purser JL. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998-2008. J Gerontol B Psychol Sci Soc Sci. 2013;68:476–485. doi:10.1093/geronb/gbt012.
Sousa RM, Ferri CP, Acosta D, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. doi:10.1016/S0140-6736(09)61829-8
Griffith L, Raina P, Wu H, Zhu B, Stathokostas L. Population attributable risk for functional disability associated with chronic conditions in Canadian older adults. Age ageing. 2010;39:738–745. doi:10.1093/ageing/afq105
Wang L, van Belle G, Kukull WB, Larson EB. Predictors of functional change: a longitudinal study of nondemented people aged 65 and older. J Am Geriatr Soc. 2002;50:1525–1534. doi:10.1046/j.1532-5415.2002.50408.x
Valderrama-Gama E, Damian J, Ruigomez A, Martin-Moreno JM. Chronic disease, functional status, and self-ascribed causes of disabilities among noninstitutionalized older people in Spain. J Gerontol A Biol Sci Med Sci. 2002;57:M716–M721.
Zeng Y. Towards Deeper Research and Better Policy for Healthy Aging—Using the Unique Data of Chinese Longitudinal Healthy Longevity Survey. China Economic J. 2012;5:131–149. doi:10.1080/17538963.2013.764677
Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17:25–46. doi:10.1146/annurev. pu.17.050196.000325
Martin LG, Feng Q, Schoeni RF, Zeng Y. Trends in Functional and Activity Limitations among Chinese Oldest-Old, 1998 to 2008. Popul Dev Rev. 2014;40:475–495. doi.org/10.1111/j.1728-4457.2014.00694.x
Zeng Y, Vaupel JW. Functional Capacity and Self-Evaluation of Health and Life of Oldest Old in China. J Soc Issues. 2002;58:733–748. doi:10.1111/1540-4560.00287
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffee MW. Studies of illness in the aged: The index of ADL, a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–191. doi:10.1001/jama.1963.03060120024016
Angleman SB, Santoni G, Von Strauss E, Fratiglioni L. Temporal trends of functional dependence and survival among older adults from 1991 to 2010 in Sweden: toward a healthier aging. J Gerontol A Biol Sci Med Sci. 2015;70:746–752. doi:10.1093/gerona/glu206
Su P, Ding H, Zhang W, Duan G, Yang Y, Chen R, et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016;16:178. doi:10.1186/s12877-016-0352-9
Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006;103:18374–18379. doi:10.1073/pnas.0608483103
Zhang Z, Gu D, Hayward MD. Early life influences on cognitive impairment among oldest old Chinese. J Gerontol B Psychol Sci Soc Sci. 2008;63:S25–S33. doi:10.1093/geronb/63.1.s25
Winship C, Radbill L. Sampling weights and regression analysis. Sociol Methods Res. 1994;23:230–257. doi:10.1177/0049124194023002004
Rubin D B. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 2004.
Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, Minkler M. Unadjusted prevalence rates: why they still matter for older adults’ disability rates. J Gerontol A Biol Sci Med Sci. 2010;65:545–546. doi:10.1093/gerona/glq031
Liang Y, Welmer AK, Wang R, Song A, Fratiglioni L, Qiu C. Trends in Incidence of Disability in Activities of Daily Living in Chinese Older Adults: 1993-2006. J Am Geriatr Soc. 2017; 65:306–312. doi:10.1111/jgs.14468
Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet. 2012;379:843–852. doi:10.1016/S0140-6736(11)61878-3
Hung WW, Ross JS, Boockvar KS, Siu AL. Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatr. 2011;11:47. doi: 10.1186/1471-2318-11-47
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Hou, C., Ping, Z., Yang, K. et al. Trends of Activities of Daily Living Disability Situation and Association with Chronic Conditions among Elderly Aged 80 Years and Over in China. J Nutr Health Aging 22, 439–445 (2018). https://doi.org/10.1007/s12603-017-0947-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0947-7