Abstract
Background
The assessment of physical activity levels of hospitalised older people requires accurate and reliable measures. Physical activities that older people in hospital commonly engage in include exercises and walking. Measurement of physical activity levels of older inpatients is essential to evaluate the impact of interventions to improve physical activity levels and to determine associations between physical activity in hospital and other health-related outcome measures.
Objective
To determine which measures are used to measure physical activity of older people in hospital, and to describe their properties and applications.
Method
A systematic review of four databases: Medline, Embase, CINAHL and AMED was conducted for papers published from 1996 to 2016. Inclusion criteria were participants aged ≥ 65 years and studies which included measures of physical activity in the acute medical inpatient setting. Studies which specifically assessed the activity levels of surgical patients or patients with neurological conditions such as stroke or brain injury were excluded. All study designs were included in the review.
Results
18 studies were included from 127 articles selected for full review. 15 studies used objective measures to measure the physical activity of older inpatients: 11 studies used accelerometers and four used direct systematic observations. Seven accelerometers were identified including the StepWatch Activity Monitor, activPAL, GENEActiv, Kenz Lifecorder EX, Actiwatch-L, Tractivity and AugmenTech Inc. Pittsburgh accelerometer. Three studies used a subjective measure (interviews with nurses and patients) to classify patients into low, intermediate and high mobility groups. The StepWatch Activity Monitor was reported to be most accurate at step-counting in patients with slow gait speed or altered gait. The activPAL was reported to be highly accurate at classifying postures.
Conclusion
Physical activity levels of older inpatients can be measured using accelerometers. The accuracy of the accelerometers varies between devices and population-specific validation studies are needed to determine their suitability in measuring physical activity levels of hospitalised older people. Subjective measures are less accurate but can be a practical way of measuring physical activity in a larger group of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The adverse effects of hospitalisation on older people are well recognised and it is estimated that between 30-60% of older people become more dependent in activities of daily living as a result (1). Studies have reported that physical activity levels of older adults in hospital are generally very low (2-4). Physical activity is defined as any bodily movement produced by skeletal muscle that results in energy expenditure (5). In the hospital setting, the common physical activities that patients are involved in include exercises and mobility. Exercise is a subset of physical activity and is planned, structured, and repetitive and has a final or an intermediate objective of improvement or maintenance of physical fitness (5). Mobility is also an aspect of physical activity and is a critical characteristic for functional independence (6). Previous studies have demonstrated the association between low mobility in hospital and several adverse outcomes including functional decline, admission to nursing home and death (7, 8). Importantly, studies have shown that interventions which promoted increased physical activity of older inpatients through rehabilitative or mobility interventions, were associated with improved physical functioning, shorter hospital stay, and reduced nursing home admissions (9-11).
Assessment of physical activity involve quantifying or describing behaviours and activities of the patient, and is different from physical function measures which generally relate to the patient’s ability to perform (12). Physical activity measures can be broadly classified into objective and subjective measures. In general, objective measurement using devices such as accelerometers and pedometers are reported to be more accurate than self-reported instruments or questionnaire (13). However, the accuracy of these objective measures vary across a whole range of devices (14). Additional factors such as sample size, population demographic, primary outcome variable of interest, cost and staffing levels are important considerations when deciding on which measure to use. Measuring physical activity of older people in hospital often presents a particular challenge as patients are acutely unwell and are generally frailer than their community-dwelling counterparts. Yet, in order to understand physical activity of hospitalised older adults and its association with health outcomes, an accurate and reliable measure is necessary.
The aim of this review is to systematically search from existing literature, the tools and measures which are currently used to assess physical activity levels of hospitalised older adults and to describe their clinimetric properties and applications.
Methods
Data Sources and Searches
An initial search of the Cochrane library and PROSPERO confirmed that no similar systematic review was identified. In August 2016, a literature search was conducted using four databases: Medline, Embase, AMED, and CINAHL. Two of the authors agreed on the keywords and MESH terms and the full search strategy for Medline is provided (see Appendix). Inclusion criteria for the review were: participants aged ≥ 65 years, any study which included measures of physical activity, studies involving acute medical inpatient setting, published from 1996 onwards. The authors chose 1996 as a cut-off point since it was highly unlikely that that any studies older than 20 years would be relevant. Studies which specifically assessed the activity levels of surgical patients or patients with neurological conditions such as stroke or brain injury were excluded. Papers not meeting all of the inclusion criteria were excluded. All languages were included in the review. Additionally, a manual search was conducted primarily from manufacturer websites for the characteristics, functionality and cost of the accelerometers included in this review.
Study selection
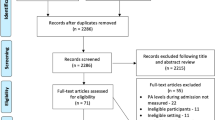
Two authors conducted the initial search of the four databases individually. Titles of articles retrieved through the initial search were then screened independently for relevance prior to abstract review. (Figure 1) Three authors independently reviewed the abstracts and articles selected by at least one author were included for full text review. Two authors reviewed the full texts and identified relevant studies for final analysis. Any disagreements were resolved through discussion. The references of selected articles were also screened for relevance.
Data extraction and Quality Assessment
Two investigators independently abstracted data from each paper with regard to study characteristics (patients’ age, study setting, number of participants), physical activity measure employed, and authors’ comments regarding each measure, including its accuracy. Additionally, data regarding the aim of the study, the duration of physical activity monitoring and comparators used were also abstracted. Any disagreement during the data abstraction process was resolved through discussion with the third reviewer.
The quality of each paper was assessed using the Downs and Black study quality checklist by two authors working independently (15). The Downs and Black checklist is commonly used to assess health care intervention studies and is appropriate for both randomised and non-randomised studies. The overall study quality is assessed by 27 questions under the following sections: study quality (10 items), external validity (3 items), study bias (7 items), confounding and selection bias (6 items) and power of the study (1 item). The quality of the study is rated against a total score of 32, with 25 items scoring 0 or 1, 1 item scoring 1 or 2, and 1 item scoring 0 to 5. No studies were excluded based on the quality of the paper.
Data synthesis and analysis
The studies included were analysed based on the type of assessment of physical activity of hospitalised older people. For studies which utilised accelerometers, information such as the make and general description of the accelerometers, the outcome measures, the reported accuracy of the devices and its practical application are described.
Due to the heterogeneity of the studies, statistical pooling of data was not appropriate and the results are presented as a narrative synthesis of the methods currently used to measure physical activity of older acute medical inpatients. PRISMA guidance was adhered to in the reporting of this review. This review is registered on PROSPERO, an international prospective register of systematic reviews: CRD42015025278.
Results
The initial search identified 5855 articles after duplicates were removed. 159 articles were selected for abstract review. 127 articles were selected by three reviewers for full text review, and 17 studies met the inclusion criteria. Reference screening identified one additional article which met the inclusion criteria thus 18 papers were included in the final analysis (Table 1). The quality of the papers, which ranged from 9/32 to 21/32, is presented in Table 2.
Objective measures
15 studies employed objective measures to measure physical activity. 11 studies used accelerometers , including one study (16) which employed two different accelerometers. Four studies (4, 17-19) used the StepWatch Activity Monitor, two studies (16, 20) used the activPAL, two studies (2, 21) used the AugmenTech Inc Pittsburgh accelerometer, and the other accelerometers used include the GENEActiv (16), Actiwatch-L (22), Tractivity (23) and Kenz Lifecorder EX 1-axial accelerometer (24). Sample sizes for the accelerometer studies ranged from 8 to 287 participants. Four studies (25-28) used direct observation as a measure of physical activity with sample sizes ranging from 47 to 124 participants. The characteristics of the accelerometers are summarised in Table 3.
StepWatch Activity Monitor
The StepWatch Activity Monitor (SAM) is a water-resistant dual-axis accelerometer worn at the ankle, attached by a Velcro strap. It is suitable for continuous monitoring and its primary outcome measure is step count (calculated by the stride count multiplied by two). Stride count is recorded at one minute intervals synchronized to a 24-hour clock. The device is time-stamped and outcomes include the average step count and percentage of time spent at low (1-15 steps/minute), medium (16-40 steps/minute) and high (>40 steps/minute) activity. The activity level definitions can be modified to suit different participant characteristics. It has a typical battery life of seven years, which is not rechargeable. Of the four studies which used SAM, only one study (4) tested its accuracy on one representative patient against direct observation and reported the device to be 99% accurate in step counting although the participant’s gait speed was not reported. The SAM has previously been reported to be accurate in measuring step counts among community-dwelling older adults (29-31), and at slow gait speeds (32) down to 0.44 m/s. Among 34 community-dwelling older people (mean age 79.2 years), the SAM was found to overestimate steps by 6.5% at gait speed <0.8m/s (33). Under laboratory conditions, the accuracy of SAM was tested on 20 participants (mean age 30 years, SD 13) who walked on a treadmill at three selected speed (0.44m/s, 0.89m/s and 1.34m/s) (32). The mean accuracy of the SAM across the three speeds was 99.7% (SD 0.67) and the intraclass correlation coefficient for SAM counts versus manual counts was 0.999. The SAM has also been shown to be accurate in step counting among patients with gait abnormalities including muscular dystrophy (34), cerebral palsy (35), multiple sclerosis (36), stroke (37), and patients who require a walking stick to aid mobility (38). It is reported to be well-tolerated by older patients (19).
activPAL
The activPAL is a single-axis accelerometer which is attached at the thigh using hydrogel pads. It can be waterproofed by wrapping medical grade adhesive around the device and attached to the thigh with a dressing, which allows continuous monitoring up to seven days. Based on thigh inclination and limb movement, the software can classify posture as sitting/lying, standing or walking. It is able to calculate step count and cadence. The output is time stamped which allows detailed analysis of the activity profile. This review identified one study which validated the use of activPAL in 14 older inpatients (mean age 84 years) against video observation and reported it to be highly accurate (100%) in classifying sedentary versus upright positions. However, the accuracy of activPAL in step counting was affected by slow gait speed (< 0.47m/s) (limits of agreement = -2.01 to 16.54, absolute percent error = 40.31) (20). One study involving 21 older community-dwelling adults (mean age 71.9±5.7) examined the accuracy of the activPAL in step counting using a treadmill and found the device to be accurate in measuring step counts with gait speeds ranging between 0.67m/s to 1.56m/s (39).
AugmenTech Inc. Pittsburgh wireless monitors
Two studies (2, 21) utilised the AugmenTech Inc. Pittsburgh accelerometer. To the authors’ knowledge, this device is no longer manufactured and attempts to contact the manufacturer were unsuccessful. As such, further description of the device is not relevant to the aims of this review.
GENEActiv
The GENEActiv is a waterproof, wrist-worn tri-axial accelerometer which produces raw data output that is time stamped. It contains a temperature sensor which enables researchers to determine how long the device was worn and if the device was removed at any point. The device allows continuous monitoring for a maximum of 7 to 45 days depending on the settings of the logging frequencies. By developing algorithms and with the use of analysis packages such as R, Matlab and Excel macro, raw data can be converted into clinically relevant outcomes such as body posture, sleep/wake measurements, and physical activity levels in terms of acceleration and metabolic equivalent of tasks (MET).
One study in this review examined the accuracy of the GENEActiv in posture classification under 3 different conditions (free-living, laboratory-based and hospital inpatients), by comparing it against another device, the activPAL (16). Ten patients (mean age 76 years) admitted to hospital with COPD wore both devices continuously for 1-2 days. The study reported that the number of minutes classified as sitting by the wrist-worn GENEActiv significantly correlated with the number of minutes classified as sitting by the activPAL (r = 0.78, p<0.01). The study also reported that the GENEActiv underestimated patients’ sitting and lying time by approximately 2.2 hours compared to the activPAL (p<0.05).
Actiwatch-L
This device which uses actigraphy technology, is wrist-worn and records movement-induced accelerations during one minute time periods. The most common clinical use of the Actiwatch-L is in evaluating sleep disorders and rest-activity rhythm disturbance. One study in this review used the Actiwatch-L to measure the rest-activity rhythm and light exposure of 10 older inpatients (mean age 81 years) admitted to an acute care unit (22) and reported that the device was well-tolerated by patients. Advances in accelerometer technology have led to further development of the device which has now been phased out and replaced by a new device, the MotionWatch 8. The MotionWatch 8 is a waterproof wrist-worn tri-axial accelerometer which allows continuous monitoring. It has been used to study physical activity levels of older adults in the community (40) and it produces data in counts per minute which can be used to classify patients into sedentary, light and moderate vigorous physical activity.
Tractivity
One study used the Tractivity to measure ambulatory levels of hospitalised patients and included a subgroup of medical inpatients age ≥65 (23). The Tractivity is water-resistant and worn on the ankle secured by an ankle band with Velcro straps. The main outcome measure is step count, which is time-stamped, and the sensor memory allows up to 30 days of continuous monitoring. This study reported an unpublished sub-study on the Tractivity and found the device to have acceptable limits of agreement with the StepWatch Activity Monitor (+284 steps; 95% limits of agreement -911 – 343) in 20 hospital inpatients whose age and gait speed was not reported (23). They also reported high reliability (intraclass correlation = 0.99) and high correlation between the Tractivity step counts and the nurses’ documentation on a paper log of distance walked measured in feet (r = 0.76).
Kenz Lifecorder EX
This device is non-waterproof, and is worn at waist level just above either leg. It is able to record step counts and time spent in various levels of intensity. Using pre-entered data such as age, sex, height and weight, the device is also able to compute physical activity energy expenditure. The device is built with an internal memory which is capable of recording up to 200 days and has a battery life of 6 months. One study in this review used the Kenz Lifecorder EX 1 axial accelerometer to measure physical activity levels of 235 cardiac inpatients (mean age 74 years) (24). It has also been used to measure step count and intensity of physical activity of community-dwelling older people (age range 60-78 years) (41). However this accelerometer may be less accurate at slow gait speeds: in one study assessing the accuracy of pedometers using a treadmill, the Kenz Lifecorder EX, which was worn by 10 male subjects (mean age 33), underestimated actual step counts by about 10% at 0.9m/s but was found to be accurate at a gait speed of 1.1m/s and above (42).
Direct observation
Four studies identified (25-28) used direct observation alone to measure physical activity and two studies (4, 20) used direct observation to validate or supplement the accelerometer data. Mudge et al (2008) measured patient activity on the ward by monitoring hallway ambulation (25). Participants were observed for 2 to 3 hours periods at varying times in the morning and afternoon shift over a 7 day period and the frequency and time spent walking in the hallways were recorded. More recently, Mudge et al (2016) utilised a behavioural mapping protocol, where participants in each room were observed for 2 minutes before moving to the next room, with the sequence repeated in the same order for 4 hours (28). Observations were done by trained physiotherapy students with 2 observation periods between 10am to 2pm and 2pm to 6pm. Activities were classified as lying in bed, sitting in or on the bed, sitting on a chair, standing, actively wheeling, or walking.
Boltz et al used a previously developed tool, the Restorative Care Behaviour Checklist, which is an observational measure of patient involvement in activities such as bed mobility, transfers, ambulation, bathing, dressing, hygiene, eating, use of personal assistive devices, communication, and exercise (26). Patients recruited in this study were observed over a 3 hour period on 3 separate occasions. Doherty-King et al utilised trained observers who shadowed 15 registered nurses each for two to three 8 hour periods. A hand-held computer tablet was used to collect data on the frequency and duration of patients’ mobility events such as standing, transferring, walking by the bed space, walking to and from the bathroom, walking in the bay and walking in the hallway (27).
Subjective measures
Three studies (7, 8, 43) utilised subjective methods to measure the physical activity of older inpatients. All three studies interviewed nurses or patients regarding the frequency of mobility of patients over the past 24 hours. Brown et al developed an empirical scoring system for increasing levels of mobility , with a score of 0 for complete bedrest, 2 for transferring from bed to chair once, 4 for transferring ≥ twice, 6 for ambulation once with total assistance, 8 for ambulation ≥ twice with total assistance or once with partial or no assistance, 10 for ≥ twice with partial assistance, and a score of 12 for independent ambulation ≥ twice per day (7). In this study, nurses looking after the patients were interviewed at baseline and on alternate days. An average score of 4 or less was classified as low level mobility, 4-8 was defined as intermediate and a score of 8 and above was considered as high mobility. Zisberg et al modified this scale with a change in scoring to 14 to take into consideration the distance mobilised by patients, classified by ambulation inside or outside their hospital room (8, 43). The sample sizes for the three studies ranged between 498- 684 participants but the validity and reliability of this measure was not reported.
Discussion
This review has shown that objective methods using accelerometers were most commonly used among researchers investigating the physical activity levels of hospitalised older people. The outcome measures produced by accelerometers include step count, posture identification, physical activity energy expenditure and physical activity intensity. The variety of outcome measures reflect the multidimensional construct of physical activity and hence using one method of measurement can be difficult to fully capture its entirety. One of the benefits of using accelerometers is continuous objective monitoring of physical activity. This review has also shown that the accuracy the accelerometers in measuring step counts or posture vary across devices.
Only three studies tested the accuracy of the devices among older people in hospital. The activPAL was shown to be highly accurate in comparison to video observation in classifying postures but lacked accuracy in step counting at gait speed <0.47m/s (20). The GENEActiv underestimated time sitting/lying by comparison with the activPAL (16). In the study by Fisher et al in 2011, the SAM was found to be 99% accurate in step counting in one representative patient (4). Older people in hospital are more likely to engage in lower intensity physical activity and have lower gait speed then their community-dwelling counterparts (44) and hence it is important that the accuracy of the device is population-specific.
The limited evidence available suggests that the SAM is the most accurate device currently available for measuring step counts of older inpatients and is reported to be well-tolerated. The activPAL is the most accurate at classifying postures in studying the activity and sedentary behaviour of hospitalised older people. It does provide step counts but has been reported to be less accurate at slower gait speeds. The GENEActiv is able to measure physical activity intensity and also classify posture.
Direct observation using a systematic approach of observing patients and coding their behaviour has benefits including elimination of the risk of recall bias, and additional contextually rich data such as the types of activity, frequency and the physical and social environment in which the physical activity takes place (45). Barriers to using direct observation include limitation of time and resources although the use of hand-held devices allows data to be entered and stored efficiently, making the data more manageable and easier to analyse. Video observation is useful for observing patients for a short period of time but is less practical for continuous monitoring.
The only subjective measure identified in this review was a score to classify patients into low, moderate and high mobility levels. The advantage of this method of measurement is its ease of use, requiring little resources, which may be relevant when studying a larger number of participants. However, it only provides an estimate of patients’ physical activity level and is susceptible to recall bias (46, 47) as the information is dependent on participants to recall activities over the past 24 hours. As older people have a higher risk of cognitive impairment or short-term memory loss, this may have an impact on the accuracy of the information collected.
For routine measurement of physical activity in the clinical setting, subjective measures are more cost-effective and practical to administer to a higher number of patients. However objective measures may be more appropriate for use in research as it provides more accurate measurements of physical activity. This review has identified a lack of evidence for the accuracy of accelerometers specifically to measure physical activity among hospitalised older people. Future research should focus on determining the accuracy of these devices in this very specific patient group.
Limitations
The search strategy was designed to include studies involving older general medical inpatients and hence studies limited to specific neurological conditions such as stroke and Parkinson’s disease were excluded. The quality of the studies included was generally modest to poor, with scores ranging from 9 to 21 out of a total of 32. Of the 18 studies included, 11 studies had a score of less than 16 out of 32. However the aim of the review is to explore the methods of measurement in current practice and hence these studies were included.
Conclusion
This review has identified and described the measures currently used to assess physical activity levels of older people in general medical wards in hospital. The seven accelerometers identified each have their own strengths and weaknesses. There are few validation studies looking specifically at the accuracy of these devices in measuring physical activity of hospitalised older people. Further population-specific validation studies are needed to determine which devices are most suitable for this group of patients to better inform researchers and clinicians who are interested in measuring physical activity levels of frail hospitalised older people. Among the devices currently used in practice, the StepWatch Activity Monitor appears to provide the most accurate step count for older people with low gait speed or altered gait. The activPAL has been shown to be highly accurate in measuring posture and while it is able to measure step count it appears to be less accurate at slow gait speed. Direct systematic observation is often time consuming and labour intensive but with the use of hand-held devices and a carefully designed observation protocol, it can be a useful measure of physical activity. Subjective measures are less accurate but can be a practical way of measuring physical activity in a larger group of patients.
Key points
-
Accelerometers are used to measure physical activity levels of older people in the acute hospital setting.
-
The StepWatch Activity Monitor appears to provide the most accurate step count among older people with low gait speed or altered gait.
-
The activPAL has been shown to be highly accurate in measuring posture.
-
Subjective measures are less accurate but can be a practical way of measuring physical activity in a larger group of patients.
Funding Source: This research is funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Wessex. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. This study is supported by the Faculty of Medicine at the University of Southampton. SEL, KI, AAS, and HCR receive support from the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Wessex. HCR and AAS receive support from the NIHR Southampton Biomedical Research Centre. SEL was supported by the University of Southampton NIHR Academic Clinical Fellowship Scheme.
Sponsor’s Role: The opinion expressed in this document are those of the authors. The sponsors had no role in the design, methods, data collection, analysis and preparation of this paper.
Conflict of Interest: The authors do not have any conflicts of interest.
Ethical standard: Informed consent was obtained from all participants.
References
Lafont C, Gerard S, Voisin T, et al. Reducing «iatrogenic disability» in the hospitalized frail elderly. The journal of nutrition, health & aging. 2011;15(8):645–660.
Brown CJ, Redden DT, Flood KL, et al. The underrecognized epidemic of low mobility during hospitalization of older adults. Journal of the American Geriatrics Society. 2009;57(9):1660–1665.
Bodilsen A, Pedersen M, Petersen J. Acute Hospitalization of the Older Patient. American Journal of Physical Medicine & Rehabilitation. 2013;92:789–796.
Fisher S, Goodwin J, Protas EJ, et al. Ambulatory Activity of Older Adults Hospitalized with Acute Medical Illness. Journal of the American Geriatrics Society. 2011;59(1):91–95.
Caspersen C, Powell K, Christenson G. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public health reports (Washington, D.C.: 1974). 1985;100(2):126–131.
Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The life study randomized clinical trial. JAMA. 2014;311(23):2387–2396.
Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. Journal of the American Geriatrics Society. 2004;52(8):1263–1270.
Zisberg A, Shadmi E, Sinoff G, et al. Low mobility during hospitalization and functional decline in older adults. Journal of the American Geriatrics Society. 2011;59(2):266–273.
Kosse NM, Dutmer AL, Dasenbrock L, et al. Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: a systematic review. BMC Geriatrics. 2013;13:107–107.
Brown CJ, Foley KT, Lowman JD, et al. Comparison of posthospitalization function and community mobility in hospital mobility program and usual care patients a randomized clinical trial. JAMA Internal Medicine. 2016;176(7):921–927.
Martínez-Velilla N, Cadore EL, Casas-Herrero Á, et al. Physical activity and early rehabilitation in hospitalized elderly medical patients: Systematic review of randomized clinical trials. The journal of nutrition, health & aging. 2016;20(7):738–751.
DiPietro L. The epidemiology of physical activity and physical function in older people. Medicine & Science in Sports & Exercise. 1996;28(5):596–600.
Colbert LH, Matthews CE, Havighurst TC, et al. Comparative validity of physical activity measures in older adults. Medicine and Science in Sports and Exercise. 2011;43(5):867–876.
Bassett DR, Dinesh J. Use of pedometers and accelerometers in clinical populations: validity and reliability issues. Physical Therapy Reviews. 2010;15(3):135–142.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health. 1998;52(6):377–384.
Rowlands AV, Olds TS, Hillsdon M, et al. Assessing sedentary behavior with the geneactiv: Introducing the sedentary sphere. Medicine and Science in Sports and Exercise. 2014;46(6):1235–1247.
Fisher SR, Graham JE, Brown CJ, et al. Factors that differentiate level of ambulation in hospitalised older adults. Age and ageing. 2012;41(1):107–111.
Fisher SR, Kuo YF, Graham JE, et al. Early ambulation and length of stay in older adults hospitalized for acute illness. Archives of Internal Medicine. 2010;170(21):1942–1943.
Ostir GV, Berges IM, Kuo YF, et al. Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. Journal of the American Geriatrics Society. 2013;61(4):551–557.
Taraldsen K, Askim T, Sletvold O, et al. Evaluation of a Body-Worn Sensor System to Measure Physical Activity in Older People With Impaired Function. Physical Therapy. 2011;91(2):277–285.
Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2012;68(3):331–337.
Vinzio S, Ruellan A, Perrin A, et al. Actigraphic assessment of the circadian restactivity rhythm in elderly patients hospitalized in an acute care unit. Psychiatry and Clinical Neurosciences. 2003;57(1):53–58.
Sallis R, Roddy-Sturm Y, Chijioke E, et al. Stepping toward discharge: Level of ambulation in hospitalized patients. Journal of Hospital Medicine. 2015;10(6):384–389.
Izawa KP, Watanabe S, Oka K, et al. Differences in daily in-hospital physical activity and geriatric nutritional risk index in older cardiac inpatients: preliminary results. Aging clinical and experimental research. 2014;26(6):599–605.
Mudge AM, Giebel AJ, Cutler AJ. Exercising body and mind: An integrated approach to functional independence in hospitalized older people. Journal of the American Geriatrics Society. 2008;56(4):630–635.
Boltz M, Resnick B, Capezuti E, et al. Functional Decline in Hospitalized Older Adults: Can Nursing Make a Difference? Geriatric Nursing. 2012;33(4):272–279.
Doherty-King B, Yoon JY, Pecanac K, et al. Frequency and duration of nursing care related to older patient mobility. Journal of Nursing Scholarship. 2013;46(1):20–27.
Mudge AM, McRae P, McHugh K, et al. Poor mobility in hospitalized adults of all ages. Journal of Hospital Medicine. 2016;11(4):289–291.
Cavanaugh JT, Coleman KL, Gaines JM, et al. Using Step Activity Monitoring to Characterize Ambulatory Activity in Community-Dwelling Older Adults. Journal of the American Geriatrics Society. 2007;55(1):120–124.
Storti KL, Pettee KK, Brach JS, et al. Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and science in sports and exercise. 2008;40(1):59–64.
Bergman RJ, Bassett DR, Muthukrishnan S, et al. Validity of 2 devices for measuring steps taken by older adults in assisted-living facilities. Journal of physical activity & health. 2008;5 Suppl 1:S166–S175.
Foster RC, Lanningham-Foster LM, et al. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Preventive Medicine. 2005;41(3–4):778–783.
Storti KL, Pettee KK, Brach JS, et al. Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and science in sports and exercise. 2008;40(1):59–64.
McDonald CM, Widman LM, Walsh DD, et al. Use of step activity monitoring for continuous physical activity assessment in boys with Duchenne muscular dystrophy. Archives of physical medicine and rehabilitation. 2005;86(4):802–808.
Bjornson KF, Belza B, Kartin D, et al. Ambulatory Physical Activity Performance in Youth With Cerebral Palsy and Youth Who Are Developing Typically. Physical Therapy. 2007;87(3):248–257.
Sandroff BM, Motl RW, Pilutti LA, et al. Accuracy of StepWatch™ and ActiGraph accelerometers for measuring steps taken among persons with multiple sclerosis. PloS one. 2014;9(4):e93511–e93511.
Mudge S, Stott NS, Walt SE. Criterion validity of the StepWatch Activity Monitor as a measure of walking activity in patients after stroke. Archives of physical medicine and rehabilitation. 2007;88(12):1710–1715.
Wendland DM, Sprigle SH. Activity monitor accuracy in persons using canes. Journal of Rehabilitation Research and Development. 2012;49(8):1261–1268.
Grant PM, Dall PM, Mitchell SL, et al. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. Journal of aging and physical activity. 2008;16(2):201–214.
Landry GJ, Falck RS, Beets MW, et al. Measuring physical activity in older adults: calibrating cut-points for the MotionWatch 8. Frontiers in Aging Neuroscience. 2015;7:165.
Koizumi D, Rogers NL, Rogers ME, et al. Efficacy of an accelerometer-guided physical activity intervention in community-dwelling older women. J Phys Act Health. 2009;6(4):467–474.
Crouter S, Schneider P, Karabulut M, et al. Validity of 10 Electronic Pedometers for Measuring Steps, Distance, and Energy Cost. Medicine & Science in Sports & Exercise. 2003;35(8):1455–1460.
Zisberg A, Shadmi E, Gur-Yaish N, et al. Hospital-Associated Functional Decline: The Role of Hospitalization Processes Beyond Individual Risk Factors. Journal of the American Geriatrics Society. 2015;63(1):55–62.
Graham E, Fisher SR, Berges I-m, et al. Walking Speed Threshold for Classifying Walking Independence in Hospitalized Older Adults. Physical Therapy. 2010;90(11):1591–1598.
McKenzie TL. The use of direct observation to assess physical activity. In: welk G, ed. Physical Activity Assessments for Health-Related Research: Human Kinetics; 2002:179–195.
Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Research quarterly for exercise and sport. 2000;71(2 Suppl):S1–14.
Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. British Journal of Sports Medicine. 2003;37(3):197–206.
Esliger DW, Rowlands AV, Hurst TL, et al. Validation of the GENEA Accelerometer. Med Sci Sports Exerc. 2011;43(6):1085–1093.
Phillips LRS, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. Journal of Science and Medicine in Sport. 2013;16(2):124–128.
Zhang S, Murray P, Zillmer R, et al. Activity classification using the GENEA: optimum sampling frequency and number of axes. Med Sci Sports Exerc. 2012;44(11):2228–2234.
Zhang S, Rowlands AV, Murray P, et al. Physical activity classification using the GENEA wrist-worn accelerometer. Med Sci Sports Exerc. 2012;44(4):742–748.
Grant PM, Ryan CG, Tigbe WW, et al. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. British Journal of Sports Medicine. 2006;40(12):992–997.
Lyden K, Kozey Keadle SL, et al. Validity of two wearable monitors to estimate breaks from sedentary time. Med Sci Sports Exerc. 2012;44(11):2243–2252.
Brown CJ, Roth DL, Allman RM. Validation of use of wireless monitors to measure levels of mobility during hospitalization. Journal of Rehabilitation Research and Development. 2008;45:551–558.
Levine B, Moyles T, Roehrs J, et al. Actigraphic monitoring and polygraphic recording in determination of sleep and wake. Sleep Research. 1986;15:247.
Cole R, Kripke D, Gruen W, et al. Automatc sleep/wake identification from wrist actigraphy. 1992. 1992;15:461–469.
Schneider PL, Crouter SE, Lukajic O, et al. Accuracy and Reliability of 10 Pedometers for Measuring Steps over a 400-m Walk. Medicine & Science in Sports & Exercise. 2003;35(10):1779–1784.
Kuys SS, Dolecka UE, Guard A. Activity level of hospital medical inpatients: An observational study. Archives of gerontology and geriatrics. 2012;55(2):417–421.
Kramer SF, Cumming T, Churilov L, et al. Measuring Activity Levels at an Acute Stroke Ward: Comparing Observations to a Device. BioMed Research International. 2013;2013:8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, S.E.R., Ibrahim, K., Sayer, A.A. et al. Assessment of Physical Activity of Hospitalised Older Adults: A Systematic Review. J Nutr Health Aging 22, 377–386 (2018). https://doi.org/10.1007/s12603-017-0931-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0931-2