Abstract
Background
Characterization of the main features of pre-frailty may contribute to better understanding the mechanisms involved in the development of frailty.
Objective
To characterize the pre-frail population consulting in primary care centres in Mataró (Catalonia, Spain), to describe the Fried’s frailty criteria for this population and to identify the main associated factors.
Design
Cross-sectional study.
Setting
Three primary care centres in Catalonia.
Participants
Pre-frail subjects recruited from among persons aged 70 years and older consulting primary care centres and screened for frailty according to Fried’s criteria.
Measurements
Clinical, nutritional and functional data.
Results
Frailty prevalence of 31.0% and pre-frailty prevalence of 49.0% were observed. Comorbidity was not especially frequent among elderly individuals classified as pre-frail (except for diabetes with 35.8% prevalence). Functional status and nutritional status were both reasonably satisfactory in pre-frail subjects with mean Barthel score of 98 points and 91% classified as well nourished. Among pre-frail subjects, 35% were obese (body mass index>30); 75% reported pain; 12% had an accidental fall in the previous three months; and the mean number of medications ingested was 6.2. Weakness was the most prevalent frailty criterion (70%), followed by slowness (30%). Weakness was associated with age in men and with pain in women. Poor physical activity was associated with pain.
Conclusions
Pre-frailty is very common among elderly subjects consulting primary care centres. Weakness, slowness, diabetes, pain and polypharmacy should alert healthcare professionals to the onset of a frailty process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a geriatric syndrome with multiple causes, characterized by diminished strength, endurance and physiologic reserves that increase the individual’s vulnerability to stressors (1). Frailty results in functional decline, disability and loss of independence; it also represents a significant healthcare burden (2). Given the progressive ageing of the population, caring for frail older adults is becoming a genuine public health problem in terms of preventing disability while promoting a more efficient and sustainable healthcare system (3). Preventing or delaying frailty requires a better understanding of the mechanisms and risk factors involved in its development and progression to disability.
Several screening tools developed to identify frail subjects also define a pre-frailty category (2, 4-7). Since frailty itself is generally considered to be reversible in its initial phases and can be treated and prevented (8, 9), the concept of pre-frailty has begun to attract growing interest in recent years. Pre-frailty identification and characterization is crucial to the design of interventions — mainly based on exercise, nutrition and polypharmacy reduction — aimed at preventing or minimizing functional decline, slowing down the transition to frailty and reducing the risk of acute complications, disability and dependency (10). Prevalence of pre-frailty in large population-based studies has been estimated at between 35% and 50% of community-dwelling elderly subjects aged 65 years and older (11). The pre-frail individual has been profiled as a poorly educated female who is obese and diabetic and has other chronic diseases (11). However, we need a more accurate characterization of the pre-frail population that takes into account sex differences and variables such as medication, nutrition and pain. We also need to better understand the main frailty phenotype components (weight loss, exhaustion, physical inactivity, slowness, weakness) affecting the pre-frail population, their main determinants and how they affect functional capacity. The aim of the present study was to characterize a pre-frail population consulting in primary care centres, to determine the prevalence of the Fried’s five frailty criteria, to identify the main clinical and modifiable factors associated with these criteria and to explore sex differences in their prevalence in this population.
Methods
Study design and population
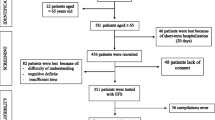
An observational cross-sectional study was designed in which non-institutionalized patients, aged 70 years and older, consulting in primary care centres for any reason were screened for frailty and pre-frailty. Pre-frail subjects who agreed to participate in the study were recruited and underwent comprehensive geriatric assessment. Subjects were recruited between October and December 2013 in three primary care centres: two in the city of Mataró and one in the nearby village of Argentona (Catalonia, Spain). Subjects were screened for frailty and pre-frailty according to Fried’s criteria (2), with individuals considered to be pre-frail if they fulfilled one or two of the following five criteria: (a) weight loss, defined as unintentional weight loss of 4.5 kg or more, weight loss of 5% or more in the last year, or body mass index (BMI) under 19 kg/m2; (b) weakness, defined as poor muscle strength of under 30 kg in men and 17 kg in women; (c) self-reported exhaustion, that is, patients answered “some of the time” or “most of the time” to the questions “how often in the last week did you feel that everything you did was an effort?” or “how often in the last week did you feel that you could not get going?”; (d) slowness, defined as slow walking speed of under 0.75 m/sec; and (e) low physical activity, defined as self-reported outdoor walking of under 30 min/day, (an adapted simple and easy criteria with similar Kcal of physical activity per week than those reported by L Fried). Exclusion criteria included an inability to stand, dementia, in receipt of palliative care and life expectancy below 6 months. All subjects that fulfil all selection criteria were consecutively recruited. The study protocol was approved by the institutional review board of the Consorci Sanitari del Maresme, Mataró, Barcelona (Spain). All participants gave their permission to participate by signing an informed consent form.
Data
Data was collected, assessed and recorded as follows: sociodemographic details (age, sex, educational level and socio-familiar support); comorbidities; number of chronic medications; nutritional status; pain (presence, location and intensity); and depression. Nutrition, pain and depression were assessed using the Mini Nutritional Assessment (MNA) instrument, a visual analogue scale (VAS) and the Geriatric Depression Scale (GDS), respectively. In a physical examination weight, height, walking speed and hand grip were measured and patients underwent the Timed Up-and-Go (TUG) test. Hand grip was measured by a dynamometer (Jamar Hand Dynamometer, Lafayette Instrument Co) held in the dominant hand. The widely used, validated TUG testis used to measure the time taken by subjects to get up from a chair with arms, walk three metres and return to sit in the chair, with scoring as follows: below 20 seconds good mobility; more than 29 seconds, needs assistance; and 20-29 seconds, borderline mobility, balance and functional ability. Functional capacity was also measured by the Barthel index which assesses ten activities of daily living on a scale ranging from 0 to 100: feeding, grooming, toilet use, bathing, dressing, transfer, mobility, climbing stairs, bladder control and bowel control. A self-reported quality of life questionnaire (EuroQoL-5D) was also administered along with a questionnaire (specifically designed for this study) about outdoor life and falls in the previous month.
Statistical analysis
Prevalence rates for frailty and pre-frailty— and the corresponding 95% confidence interval (CI) — were estimated using data from the two Mataró primary care centres, which registered 306 consecutive patients and identified 150 pre-frail subjects. For the objective of describing main characteristics of the pre-frail population, other 21 pre-frail cases identified in the primary care centre of Argentona were added to the pre-frail sample, obtaining an overall sample of 171 pre-frail subjects. The main objectives of the study were descriptive. Continuous and categorical variables were described using means (SD) and percentages, respectively. The variables associated with the presence of each frailty criterion were compared using the chi-square test or Fisher’s exact test. Continuous variables were compared using the Mann-Whitney U test or the t-test for independent data. All analyses were performed for the total sample and for women and men separately. Statistical significance was set at p<.05.
Results
In Mataró, a total of 306 consecutive subjects were screened for frailty, classified as follows: pre-frail, 150 (49.0%); frail, 95(31.0%); and robust, 61 (20.0%). Table 1 shows the prevalence of frailty and pre-frailty by age and sex, indicating a higher prevalence of frailty in women and individuals aged over 80 years. In the overall study (Mataró and Argentona), 171 pre-frail subjects were recruited, 76 men and 95 women. Table 2 presents the main characteristics of the pre-frail sample, broken down for men and women. The most prevalent comorbid conditions were arthrosis, diabetes, hypertension and dyslipidaemia. The prevalence rate for heart failure was under 20% and the prevalence rates for chronic bronchitis/chronic obstructive pulmonary disease, stroke, Parkinson disease, dementia, cancer, chronic kidney failure and chronic liver disease were all under 10%. Pre-frail subjects were ingesting 6.2 medications on average, had mostly an outdoor life and had preserved their functional capacity and nutritional status. One third of the sample was obese while fewer than 2% were underweight. Three quarters of the pre-frailty sample reported pain, mostly in the back or lower limbs and 12% reported accidental falls in the previous three months. Compared to men, women had lower educational levels, were more likely to live alone, to suffer depression and to take drugs, had poorer functional capacity and reported greater pain.
The prevalence of each Fried criterion in pre-frail individuals is summarized in Table 3. Weakness was most prevalent overall, followed by slowness and exhaustion. Physical activity was preserved in over 80% of cases, and weight loss was the least prevalent criterion. The pattern was similar for both sexes, although slowness was somewhat more prevalent in women. A positive weakness criterion was associated with age in men and with back pain in women. Thus, 90% of men aged >80 years compared to 67% of men aged 70-80 years had poor muscle strength (p=.020); and 71% of women with back pain compared to 47% of women with no back pain had poor muscle strength (p=.049). Low physical activity was also associated with lower limb pain (25.0% of those with pain compared to 9.3% of those without pain; p=.041). Finally, slowness was associated with the TUG test result (11.4 sec in those with slowness vs 8.5 sec in those without slowness; p<.001), number of hours walked daily (0.87 hours in those with slowness vs 1.24 hours in those without slowness; p=.002) and number of medications (7.1 medicationsin those with slowness vs 5.3 medications in those without slowness; p=.016).
Discussion
Pre-frailty is an easily identified and highly prevalent clinical condition that frequently leads to functional decline and frailty. In our study pre-frailty prevalence was 49% among individuals aged 70 years and older consulting a primary care centre for any reason — a rate corroborated by other studies based on larger populations: 47% among subjects aged 65 years and older according to the Cardiovascular Health Study (2); 40% in subjects aged 60 years and older according to the Third National Health and Nutritional Examination Survey (12); 32% in subjects aged 65 years and older according to the InCHIANTI study (13); and 37% in subjects aged 50–65 years according to the Survey of Health, Ageing and Retirement in Europe (14). Our slightly higher pre-frailty prevalence rate was probably because our study population was older and was drawn from persons consulting primary care centres. As for frailty, we observed an overall prevalence of 31%, and, in agreement with other published studies, prevalence increased with age and was higher in women (14). The data would indicate that approximately 80% of elderly people aged 70 years and older who consult in primary care settings are at high risk of falls, acute complications, disability or dependence. It is thought that pre-frailty is a reversible and intermediate stage that should alert health professionals to potential functional decline and evolution to frailty or disability (11). Prevention programmes for these health problems need to be urgently implemented to avoid or even reverse functional capacity decline. There is abundant evidence on the positive impact of physical exercise and nutrition interventions in elderly populations (15). However, evidence for the effectiveness of specific frailty and pre-frailty screening programmes is scarce.
A deeper understanding of pre-frailty and its features is required in order to be able to design effective interventions to reverse the condition and prevent disability. A comparison with a randomly selected sample of community-dwelling individuals of the same age and from the same setting — previously documented by our group (16) — indicates that the pre-frail population consulting in primary care settings is not an especially comorbid population; our pre-frail subjects showed prevalence rates for the main chronic diseases that were similar to those for community-dwelling individuals, with the exception of diabetes, which was more prevalent in the pre-frail sample, in both men (34.4% vs 19.6%, respectively) and in women (37.0% vs 21.9%). Diabetes thus seems to be associated with a pre-frail condition. There is growing evidence of the effect of diabetes on skeletal muscle (17) and of accelerated loss of muscle mass and strength in individuals with diabetes (18, 19). Insulin resistance could also be a risk factor for muscle loss (20) because it produces a decrease in protein synthesis and an increase in protein degradation. Insulin is a powerful anabolic signal stimulating muscle protein synthesis in young people; in aged subjects with insulin resistance, however, insulin signalling is suppressed. Moreover, the bio-energetic capacity of skeletal muscle may also be impaired in diabetes; skeletal muscle adenosine triphosphate production is reduced, due to impaired insulin response (21), with the diminished energy availability predisposing an individual to frailty. We also observed that 26% of pre-frail men and 42% of pre-frail women were obese (BMI >30). Obesity also contributes to the development of pre-frailty and frailty by promoting pro-inflammatory processes, insulin resistance, fat infiltration of the skeletal muscle, poor physical activity and hormonal changes with catabolic and satiation effects (such as increased leptin or decreased adiponectin levels) (22). All these changes may lead to a loss of muscle mass and/or strength and to the development of sarcopenic obesity, and, consequently, to pre-frailty and frailty.
Regarding chronic medication, the mean intake of 6.2 prescribed drugs per pre-frail subject in our study can be rated as chronic polypharmacy. Prescriptions in the elderly have increased in recent years and, although this may indicate an improvement in care, careful analysis in terms of quality of care, safety and costs is required (23). Polypharmacy is a known risk factor for falls (24) and should alert physicians to the risk of developing frailty. Drug interactions, duplications, side effects and other drug-related problems increase with the number of medications and are of special relevance in the elderly. Some physiological changes occur with age that may affect pharmacokinetics and pharmacodynamics, such as slow absorption, changes in body composition (increased fat and decreased total water), decline in blood albumin concentrations and impaired liver and renal function affecting drug absorption, distribution and metabolism. All medication in the elderly should be reviewed according to proposed recommendations, such as those by Beers (25), STOPP-START (26), IPET (27) or ACOVE (28).
As far as we know, only three studies have reported the prevalence of each Fried criteria in the pre-frail population (29, 30, 12). We observed 70% prevalence of positive weakness criterion, a rate higher than reported in other studies of pre-frail subjects, probably because of differing age ranges. However, our results agree with the other studies in reporting weakness as the most prevalent Fried criterion. Danon-Hersch et al (29) observed that weakness was associated with heart disease, diabetes mellitus and arthritis in pre-frail subjects aged 65 years and older. The effect of heart disease on weakness may be due to low physical activity, the effect of arthritis may be due to limited physical activity secondary to pain, and the effect of diabetes has been commented above. We observed very high prevalence of pain (75%) in pre-frail elderly subjects; furthermore, the mean pain intensity score was 5 on a 0–10 points scale, indicating moderate pain. We also noted a relationship between Fried weakness and back pain in women and between low physical activity and lower limb pain in the whole sample. Pain may lead to low physical activity, immobility, fatigue and, as consequence, muscle atrophy and loss of muscle strength. Because of the cross-sectional design of our study, it was not possible to establish whether pain was the cause or consequence of diminished muscle function; however, it seems reasonable to assume that pain may be responsible for limited physical activity which, in turn, leads to loss of muscle strength. Our results would underline the need to systematically explore pain in elderly subjects, given that it can be a triggering factor for frailty. Pain is a modifiable factor and its palliation or elimination is likely to contribute to enhanced functional capacity — although, again, we would suggest that the effects of pain on functional capacity and frailty also need further study. Our study has some limitations. The cross-sectional design only allows associations and not causal relationships to be established between different factors. The lack of a non-frail control group with which to compare prevalence rates for the main factors studied and the limited sample size are other limitations.
In summary, pre-frailty is very common among elderly subjects consulting in primary care settings. Weakness is the main frailty component affecting pre-frail subjects. The presence of diabetes, pain or polypharmacy should alert healthcare professionals to the existence of frailty or pre-frailty; furthermore, addressing these issues should contribute to delaying the onset of full-blown frailty. Simple screening tools to identify pre-frailty and frailty conditions in primary care settings are available and simple interventions have shown effectiveness in preventing loss of muscle mass and strength. Nonetheless, more research is needed into the effectiveness of frailty and pre-frailty screening programmes in primary care settings in preventing functional decline and disability.
Acknowledgements: This study was funded by grants from the Spanish Ministry of Health, Instituto de Salud Carlos III (ISCIII), Fondo de Investigación Sanitaria (FIS) programme; PI13/00931.
Conflict of interest: The authors have no conflicts of interest to disclose.
Ethical standards: The authors declare that the present study comply with the Spanish law and all international ethical standards.
References
Morley J, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. Journal of the American Medical Directors Association 2013; 14: 392–7.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2001; 56 (3): M146–M156.
Vellas B, Cestac P, Morley JE. Implementing frailty into clinical practice: we cannot wait. J Nutr Health Ageing 2012; 16 (7): 599–600.
Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–95.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 2012; 16: 601–8.
Steverink N, Slaets JPJ, Schuurmans H, Lis van M. Measuring frailty: development and testing of the Groningen frailty indicator(GFI). Gerontologist 2001; 41: 236–7.
Searle S, Mitnitski A, Gahbauer E, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr2008; 8: 24.
Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med 2006; 166: 418–23.
Walston JD. Frailty–and its dangerous effects-might be preventable. Ann In Med 2004; 141: 489–92.
Clegg A, Young J, Ilife S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752–62.
Fernandez-Garrido J, Ruiz-Ros V, Buigues C, Navarro-Martínez R, Cauli O. Clinical features of pre-frail older individuals and emerging peripheral biomarkers: A systematic review. Arch GerontolGeriat 2014. http://dx.doi.org/10.1016/j. archger.2014.02.008
Smit E, Winter-Stone KM, Loprinzi PD, Tang AM, Crespo CJ. Lower nutritional status and higher food insufficiency in frail older US adults. British Journal of Nutrition 2013; 110: 172–8.
Shardell M, D’Adamo C, Alley DE, Miller RR, Hicks GE, Milaneschi Y et al. Serum 25-hydroxivitamin D, transitions between frailty states, and mortality in older adults: The invecchiare in Chianti study. Journal of the American Geriatrics Society 2012; 60 (2): 256–64.
Santos-Egimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middleaged and older community dwelling Europeans living in 10 countries. Journals of Gerontology Series A: Biologica Sciences and Medical Sciences 2009; 64A (6): 675–81.
Foster A, et al. Rehabilitation for older people in long term care. Cochrane database of systematic reviews. 2009, 1 (CD004294).
Puig-Domingo M, Serra-Prat M, Merino MJ, Pubill M, Burdoy E, Papiol M, et al. Muscle strength in the Mataró Ageing study participants and its relationship to successful ageing. Ageing ClinExp Res 2008; 20: 439–46.
Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHNES), 1999-206. Diabetes Care 2010; 33: 1055–60.
Park SW, Goodpaster BH, Lee JS, and the Health, Ageing, and Body composition study. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care 2009; 32: 1993–7.
Park SW, Goodpaster BH, Strotmeyer ES and the Health, Ageing, and Body composition study. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, ageing, and body composition study. Diabetes Care 2007; 30: 1507–12.
Barzilay JI, Cotsonis GA, Walston J, and the Health ABC study. Insuline resistance is associated with decreased quadriceps muscle strength in non diabetic adults aged ≥70 years. Diabetes care 2009; 32: 736–8.
Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002; 51: 2944–50.
Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol 2014; 2 (10): 819–29.
Franchi C, Tettamanti M, Pasina L, Djignefa CD, Fortino I, Bortolotti A, et al. Changes in drug prescribing to italian community-dwelling elderly people: the EPIFARM-Elderly project 2000-2010. Eur J ClinPharmacol 2014; 70 (4): 437–43.
Richardson K, Bennett K, Kenny RA. Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. Age Ageing 2014 pii: afu141
Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med 1997;157:1531–6.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J ClinPharmacolTher. 2008 Feb;46(2):72–83.
Naugler CT, Brymer C, Stolee P, Arcese ZA. Development and validation of an improving prescribing in the elderly tool. Can J ClinPharmacol. 2000 Summer;7(2):103–7
Wenger NS, Shekelle PG. Assessing care of vulnerable elders: ACOVE Project overview. Ann Intern Med. 2001 Oct 16;135(8 Pt 2):642–6.
Danon Hersch N, Rodondi N, Spagnoli J, Santos-Eggimann B. Prefrailty and chronic morbidity in the youngest old: an insight from the Lausanne cohort Lc65. Journal American Geriatrics Society 2012; 60 (9): 1687–94.
Xue Q, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Ageing Study II. Journalñs of Gerontology Series A: Biological Sciences and Medical Sciences 2008; 63 (9): 984–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Serra-Prat, M., Sist, X., Saiz, A. et al. Clinical and functional characterization of pre-frailty among elderly patients consulting primary care centres. J Nutr Health Aging 20, 653–658 (2016). https://doi.org/10.1007/s12603-016-0684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0684-3