Abstract
Lactobacilli in the vaginal tract are essential to protect against microbial infections. We therefore focused on isolating vaginal lactobacilli from pregnant women and testing their functional properties. Lactobacilli were isolated from 50 vaginal swabs and the purified isolates were identified by MALDI-TOF MS. Functional properties (antimicrobial activity, organic acids and hydrogen peroxide production, antibiotic susceptibility, auto-aggregation, and hydrophobicity) of selected isolates were tested. Lactobacilli (41 strains) were identified in 58% of swabs with a predominance of Lactobacillus crispatus (48%) followed by L. jensenii (21%), L. rhamnosus (14%), L. fermentum (10%), and L. gasseri (7%). The highest antibacterial activity was determined for L. fermentum and L. rhamnosus. Strong anti-Candida activity was observed for strains L. crispatus, L. fermentum, and L. rhamnosus. Strain L. jensenii 58C possessed the highest production of hydrogen peroxide (6.32 ± 0.60 mg/l). The best lactic acid producer was strain L. rhamnosus 72A (11.6 ± 0.2 g/l). All strains were resistant to fluconazole and metronidazole. The highest auto-aggregation was observed for strain L. crispatus 51A (98.8 ± 0.1% after 24 h). Strain L. rhamnosus 68A showed the highest hydrophobicity (69.1 ± 1.4%). Strains L. fermentum and L. rhamnosus showed high antibacterial activity and hydrophobicity, and strains L. crispatus possessed high auto-aggregation and anti-Candida activity. Thus, these strains alone or in a mix could be used for the preparation of probiotic products for treatment and prevention of vulvovaginal infections of pregnant and non-pregnant women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vaginal microbiome of healthy women is a dynamic ecosystem, and it is colonized by a variety of microorganisms. The composition of the vaginal microbiome is influenced by a number of factors such as age, hormonal levels, sexual activity, hygiene, phase of menstrual cycle, or diet [1, 2]. In healthy premenopausal women, bacteria of the genus Lactobacillus are dominant in the vaginal microbiome at 107–108 CFU/g of vaginal fluid [3]. The most frequently found are species of L. crispatus, L. gasseri, L. iners, and L. jensenii, but this depends on ethnic group or geographic location. There are also differences between pregnant and non-pregnant women; lower strain diversity was found in pregnant women. On the other hand, lactobacilli in pregnant women are more stable than in non-pregnant women [2, 4, 5].
The healthy urogenital tract plays a significant role in protecting against vaginal infections, and vaginal lactobacilli are important because of their protective functions (adhesion to the vaginal tissue and production of antimicrobial substances) [3]. An abnormal vaginal microbiome may lead to vaginal infections, and production of pro-inflammatory cytokines and prostaglandins, which can cause uterine contractions and weaken fetal membranes at pregnant women. Thus, the presence of abnormal microbiome in early pregnancy is recognized as a risk factor for preterm delivery and low birth weight. Preterm birth is defined as delivery before 37 completed weeks of gestation and it is responsible for neonatal morbidity and mortality almost in 80% [6,7,8,9]. Usually, preterm birth is caused by microbial attack in the amniotic cavity, especially by Streptococcus agalactiae. This pathogenic microorganism colonizes the lower vaginal tract and can also cause neonatal infections [4, 10, 11]. Preterm birth or amniotic fluid infection is also associated with bacterial vaginosis, which can be caused by a variety of microorganisms such as Gardnerella vaginalis, Mycoplasma hominis, or Atopobium vaginae [4, 12].
The protective role of vaginal lactobacilli is based on two main mechanisms. The first protective mechanism is specific adhesion of lactobacilli to the vaginal tissue, where formation of a biofilm can inhibit adhesion of pathogenic vaginal microorganisms by several mechanisms (e.g., competition for receptors, displacement of adhered pathogenic microorganisms, and avoiding their re-adhesion) [2, 13, 14]. The second protective mechanism is the production of antimicrobial substances (e.g., organic acids, hydrogen peroxide, bacteriocins) [15]. Organic acids, mainly lactic acid, are produced as the final product of carbohydrate fermentation and acidify the vaginal tract to pH 3.5–4.5. However, the pH is influenced by many factors (age, vaginal infection, and phase of menstrual cycle) [2, 9, 16, 17]. Some strains of vaginal lactobacilli, including L. acidophilus, L. crispatus, L. fermentum, and L. jensenii, are able to produce hydrogen peroxide. These lactobacilli are important because the hydrogen peroxide can reduce the development of bacterial vaginosis, as well as infections caused by HIV-1 and herpes simplex viruses [2, 18]. Other antimicrobial substances produced by vaginal lactobacilli are bacteriocins (proteins with antimicrobial activity), reuterin, and biosurfactants [2, 16, 18].
Lactobacilli, therefore, are able to inhibit the growth of pathogenic microorganisms through various mechanisms and may help in the reduction of vaginal infections. Knowledge of the biology and metabolic activities of vaginal lactobacilli is therefore important for the prevention and treatment of vaginal infections.
The aim of this study was to isolate vaginal lactobacilli from healthy pregnant women in the 36th week of pregnancy. We focused on functional properties testing, especially on antimicrobial activity testing, to find out strains suitable for the treatment of pregnant women’s vaginal infections which induce preterm birth or neonatal infections.
Materials and Methods
Samples
Fifty swab samples were obtained from healthy pregnant women (36th week of pregnancy) from the Czech Republic. Samples were collected at the Department of Obstetrics and Gynecology of the First Faculty of Medicine, General University Hospital, Charles University, Prague, Czech Republic, and stored at 6 °C for 48–72 h. Sample collecting was approved by the Ethics Committee of the General University Hospital.
Isolation and Identification
Swabs were vortexed for 1 min at maximum speed (2800 min−1) in de Man, Rogosa, and Sharpe (MRS) broth (Merck, Germany). The suspension was diluted 3 times with physiological saline. Each dilution (100 μl) was seeded on MRS agar (Merck, Germany) and blood agar (Columbia blood agar base with 5% defibrinated sheep blood) (Oxoid, UK) plates. The plates were incubated at 37 °C for 48 h, under a modified atmosphere containing 5% CO2. After incubation, the colonies were identified by colony morphology, catalase test, and Gram staining. Selected colonies were identified by MALDI-TOF MS. Identified isolates were stored at − 21 °C in MRS broth supplemented with glycerol (Penta, Czech Republic) (50% v/v).
Indicator Microorganisms
As indicator microorganisms for antimicrobial activity testing, we used the following pathogenic microorganisms. Five strains (Escherichia coli CCM 4517, Gardnerella vaginalis CCM 6221, Staphylococcus aureus CCM 4516, Staphylococcus aureus CCM 7719, Candida albicans CCM 8215) were obtained from the Czech collection of microorganisms (CCM, Czech Republic). Gardnerella vaginalis DSMZ 104275 was obtained from the German collection of microorganisms and cell cultures (DSMZ, Germany). Two strains (Candida glabrata ATCC 2001, Candida parapsilosis ATCC 22019) were obtained from the American type culture collection (ATCC, USA). Three strains (Escherichia coli MK 57B, Streptococcus agalactiae MK 14E, Streptococcus agalactiae MK 31B) were obtained from the Collection of microorganisms of the Department of Dairy, Fat and Cosmetics, both isolates originally from the vaginal tract.
Cultivation
Lactobacilli were cultivated in MRS broth at 37 °C, for 18 h, under a modified atmosphere containing 5% CO2 (overnight grown culture). Pathogenic bacteria were cultivated aerobically in Brain heart infusion (BHI) broth (Himedia, India) at 37 °C, for 24 h. Pathogenic yeasts were cultivated aerobically in Malt extract broth (Oxoid, UK) at 30 °C, for 24 h.
Antibacterial Activity
Antibacterial activity of selected Lactobacillus spp. isolates was tested by agar spot-diffusion method against eight pathogenic microorganisms (E. coli CCM 4517, E. coli MK 57B, G. vaginalis DSMZ 104275, G. vaginalis CCM 6221, S. aureus CCM 4516, S. aureus CCM 7719, St. agalactiae MK 14E, St. agalactiae MK 31B). The BHI soft agar (pH 5.6 before sterilization) was inoculated with the indicator pathogenic microorganisms at a density of 105 CFU/ml. The inoculated BHI soft agar was poured into a Petri dish and left to solidify. Live cells of each Lactobacillus strain (10 μl) were injected into the inoculated BHI soft agar. These plates were incubated aerobically at 37 °C for 24 h. Antibacterial activity was evaluated by the diameter of the zones of inhibition (≤ 5 mm, low inhibition; 5–10 mm, medium inhibition, ≥ 10 mm, high inhibition).
Anti-Candida Activity
Anti-Candida activity of lactobacilli isolates was tested against three pathogenic yeasts (C. albicans CCM 8215, C. glabrata ATCC 2001, and C. parapsilosis ATCC 22019). Bacterial cells of an overnight grown culture were harvested by centrifugation at 8600g, for 5 min, at 4 °C. Cells were washed twice in physiological saline under the same conditions. Washed cells were adjusted to McFarland 2 in physiological saline. This suspension (1 ml) was inoculated onto a Petri dish and overlaid with MRS agar. Plates were incubated at 37 °C, for 24 h, under a modified atmosphere containing 5% CO2. After 24 h, Malt extract agar was poured onto the inoculated plates. Yeast cells from an overnight grown culture were harvested by centrifugation at 8600g, for 5 min, at 4 °C. Cells were washed twice in physiological saline and then adjusted to McFarland 0.5 with the same solution. This suspension (100 μl) was inoculated onto the Malt extract agar layer. Plates were incubated at 37 °C, for 24 h, under a modified atmosphere containing 5% CO2. These plates were subsequently incubated aerobically at 25 °C, for 24 h. The anti-Candida activity was assessed by yeast growth and inhibition activity was evaluated as follows: +++, high anti-Candida activity (total inhibition of Candida spp.); ++. medium anti-Candida activity; +, low anti-Candida activity; 0, no anti-Candida activity (high growth of Candida spp.).
Production of Organic Acids
Production of organic acids was detected by HPLC (Agilent 1260 Infinity, USA). Bacterial cells from an overnight grown culture were centrifuged at 17,000g, for 10 min, at 4 °C. The supernatant (250 μl) was transferred to an Eppendorf tube and 1600 μl of ethanol (96%) were added and mixed. This mixture was incubated for 30 min at room temperature and then centrifuged at 17,000g, for 10 min, at 4 °C. After centrifugation, the mixture was filtered through a 0.22 μm PVDF filter. HPLC was performed using a Polymer IEX H column (Watrex, Czech Republic) (350 × 8 mm) with a pre-column (50 × 8 mm). The column and pre-column were preheated to 60 °C. The mobile phase was H2SO4 (9 mmol/l) with a flow of 0.6 ml/min. Detection was by UV detector (210 nm; 55 °C; 500 mV). The concentration of lactic acid was evaluated using a calibration curve.
Hydrogen Peroxide Production—Plate Method
Determination of hydrogen peroxide produced by lactobacilli was tested on MRS agar supplemented with 3,3′,5,5′-tetramethylbenzidine (250 μl/ml) (Sigma-Aldrich, USA) and horseradish peroxidase (0.01 mg/ml) (Sigma-Aldrich, USA). Plates were inoculated with selected Lactobacillus spp. and incubated anaerobically at 37 °C, for 48 h, using an anaerobic jar containing AnaeroGen™ (Oxoid, UK). After incubation, plates were exposed to aerobic conditions for 30 min. Colonies of hydrogen peroxide producing strains form a blue pigment.
Detection of Hydrogen Peroxide Concentration—Spectrophotometric Method
Bacterial cells from an overnight grown culture were centrifuged at 8600 g, for 5 min, at 4 °C. Supernatant was removed and the cells were washed twice by phosphate buffer (1 mol/l; pH 6.8). Cooled phosphate buffer (20 ml) was added to washed cells and mixed. This suspension was cultivated at 5 °C, for 48 h. After cultivation, the suspension was centrifugated at 8600g, for 5 min, at 4 °C. Obtained supernatant was used for the quantification of H2O2. The supernatant (5 ml) was mixed with water solution of horse radish peroxidase (1 ml; 0.001% w/v) and methanolic solution of o-dianisidine (0.1 ml; 1% w/v) (Sigma-Aldrich, USA), and this mixture was cultivated at 37 °C, for 10 min. Then HCl solution (0.2 ml; 4 mol/l) was added and the absorbance of samples was measured at 400 nm. Concentration of H2O2 produced by lactobacilli was evaluated according to the calibration curve of H2O2, which was measured by the same procedure with H2O2 solutions in phosphate buffer instead of supernatant.
Hemolytic Activity
Lactobacilli were streaked onto blood agar with 5% of defibrinated sheep blood. Inoculated plates were incubated at 37 °C, for 48 h, under a modified atmosphere with 5% of CO2. The result was evaluated visually according to zones of hemolysis. The Staphylococcus aureus CCM 3953 was used as a positive control, which showed β-hemolysis.
Antibiotic Resistance
Antibiotic resistance was tested by disk diffusion method with 15 antibiotics (Oxoid, UK): ampicillin (AMP; 10 μg), cefotaxime (CTX; 30 μg), chloramphenicol (C; 30 μg), ciprofloxacin (CIP; 5 μg), clindamycin (DA; 2 μg), erythromycin (E; 15 μg), fluconazole (FCA; 25 μg), gentamicin (CN; 10 μg), kanamycin (K; 30 μg), metronidazole (MTZ; 5 μg), nitrofurantoin (F; 300 μg), ofloxacin (OFX; 5 μg), streptomycin (S; 10 μg), tetracycline (TE; 30 μg), and vancomycin (VA; 30 μg). Bacterial cells of an overnight grown culture were centrifuged at 8600g, for 5 min, at 4 °C. Cells were washed in physiological saline under the same conditions. Washed cells were adjusted to McFarland 1 in physiological saline. This suspension (100 μl) was inoculated onto Mueller-Hinton agar (Oxoid, UK) plates and MRS agar plates. Antibiotic discs were placed on the surface of the agar and the plates were incubated at 37 °C, for 48 h, under a modified atmosphere containing 5% of CO2. Diameters of inhibition zones were measured after incubation.
Auto-Aggregation
Bacterial cells from an overnight grown culture were harvested by centrifugation at 8600g, for 5 min, at 4 °C. Cells were washed twice in phosphate buffered saline (PBS) (pH 7.2 before sterilization) under the same conditions. Cells were adjusted to an absorbance (650 nm) of 0.45–0.55. Samples were incubated aerobically at 37 °C, for 24 h. At times 0, 6, and 24 h, 1 ml of the upper layer was transferred to a cuvette and the A650 was measured. The percentage of auto-aggregation was calculated using the following equation. As a blank, pure PBS was used.
A0…A650 at 0 h
Ax…A650 at times 6 or 24 h
Hydrophobicity
Bacterial cells from an overnight grown culture were harvested by centrifugation at 8600g, for 5 min, at 4 °C. Cells were washed twice in PBS (pH 7.2 before sterilization) under the same conditions. The suspension was adjusted to an A650 of 0.45–0.55 and 3 ml were added to a glass tube. Hexane (0.5 ml) was added, vortexed for 1 min and incubated for 20 min at room temperature. The water layer was then removed and the A650 was measured. The percentage of hydrophobicity was calculated using the following equation. As a blank, pure PBS was used.
Abefore…A650 adjusted before extraction
Aafter…A650 after extraction
Results
Identification of Vaginal Lactobacilli
Bacteria from the genus Lactobacillus occurred in 29 (58%) out of 50 samples of vaginal swabs of pregnant women and 41 strains of lactobacilli were isolated. The most frequent species was L. crispatus (48%). The next most frequent were L. jensenii (21%), L. rhamnosus (14%), L. fermentum (10%), and L. gasseri (7%). Pre-screening of all isolates was focused especially on growth ability and afterwards 21 isolates were selected for further testing of functional properties.
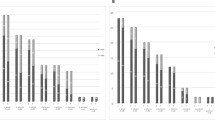
Antibacterial Activity
Antibacterial activity of lactobacilli was tested by the agar spot-diffusion method against five indicator pathogenic microorganisms. The antibacterial activity was measured with live lactobacilli. Results are summarized in Table 1. The major proportion of isolates was inhibitory against all pathogenic bacteria tested. All isolates inhibited growth of G. vaginalis DSMZ 104275 and Str. agalactiae MK 14E. Strains L. rhamnosus 10A, L. fermentum 74A, and L. fermentum 74B were strongly inhibitory against all pathogenic bacteria tested.
Anti-Candida Activity
Lactobacillus spp. isolates were tested against three pathogenic yeasts and results are presented in Table 2. The highest anti-Candida activity was observed against C. albicans CCM 8215 by all lactobacilli tested. Isolates of L. crispatus, L. fermentum, and L. rhamnosus showed very good inhibitory activity against Candida spp. whereas most strains of L. gasseri and L. jensenii showed poor or no anti-Candida activity.
Production of Hydrogen Peroxide and Organic Acids
Lactobacilli are able to produce antimicrobially active substances. The majority are organic acids (mainly lactic acid) and hydrogen peroxide. All isolates were tested for hydrogen peroxide production and this was determined by pigment changes in colonies. It was found that 71% (Table 3) of isolates were able to produce hydrogen peroxide. Production was divided into two groups, low production of H2O2 (light blue pigmented colonies) and high production of H2O2 (dark blue pigmented colonies). Color changes of colonies were detected for all strains of L. crispatus, L. gasseri, and L. jensenii. On the other hand, detection of hydrogen peroxide by spectrophotometry method showed all strains are able to produce hydrogen peroxide in different concentrations. The highest concentration of H2O2 was detected for L. jensenii 58C (6.32 ± 0.60 mg/l). The lowest concentration of H2O2 was detected for strain L. rhamnosus 72A (0.33 ± 0.05 mg/l).
Production of organic acids was tested by HPLC and the concentration of lactic acid was calculated (Table 3). The concentration of lactic acid ranged from 4.6 ± 0.1 g/l to 11.6 ± 0.2 g/l and was strain specific. The best lactic acid producer was strain L. rhamnosus 72A (11.6 ± 0.2 g/l), followed by strains L. crispatus 2A and L. crispatus 69E (10.4 ± 0.0 g/l for both of them). The lowest concentration of lactic acid was detected for strain L. crispatus 51A (4.6 ± 0.1 g/l).
Hemolytic Activity
No strain showed the β-hemolysis (complete lysis of erythrocytes) on blood agar with defibrinated sheep blood. Strains L. gasseri (71 B, 71C) showed α-hemolysis (partial decomposition of hemoglobin). No hemolysis was detected for other tested lactobacilli.
Antibiotic Resistance
Antibiotic resistance was tested for all 21 Lactobacillus spp. isolates on Mueller-Hinton agar and MRS agar plates. Differences between each tested media were detected in 28% cases without significant variance. Table 4 shows the sensitivity of each strain to antibiotics on Mueller-Hinton agar. All isolates were resistant to fluconazole and metronidazole and sensitive to ampicillin, erythromycin, chloramphenicol, and tetracycline. When antibiotic susceptibility was tested on MRS agar, lactobacilli possessed higher resistance to gentamicin, kanamycin, and streptomycin. Sensitivity to other antibiotics tested was strain specific.
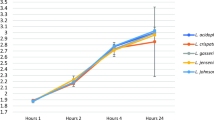
Auto-Aggregation and Hydrophobicity
The results of auto-aggregation and hydrophobicity testing are summarized in Table 3. These results represent strain diversity between isolates. Our isolates showed auto-aggregation between 12.1–89.9% after 6 h and 32.5–98.8% after 24 h. A significant proportion of L. crispatus strains tested showed very strong auto-aggregation, more than 90% after 24 h. The highest auto-aggregation was determined for strain L. crispatus 51A (98.8 ± 0.1% after 24 h) and the lowest was observed for strain L. rhamnosus 10A (32.5 ± 3.8% after 24 h).
Hydrophobicity of our isolates was in the range 19.1–69.1%. The highest hydrophobicity was exhibited by strain L. rhamnosus 68A, which achieved 69.1 ± 1.4% and the lowest was shown by strain L. jensenii 51E (19.4 ± 2.4%). In this study, no correlation between auto-aggregation and hydrophobicity was observed.
Discussion
Lactobacilli were isolated from vaginal swabs obtained from healthy pregnant women in the third trimester. All swabs were collected in the same time in the 36th week of pregnancy to obtain relevant results. During this period, estrogen levels are high, as well as lactobacilli abundance. Romero et al. [19] found out that bacterial microbiota is more stable during normal pregnancy than in the non-pregnant state. Also, they identified four lactobacilli (L. crispatus, L. gasseri, L. jensenii, L. vaginalis) as species with higher relative abundance in pregnant women. In our study, the most frequent species were L. crispatus, followed by L. jensenii, L. rhamnosus, L. fermentum, and L. gasseri. These results are typical for European woman and they correspond with several studies. For example, Kiss et al. [20] observed lactobacilli in the vaginal microbiome of pregnant women of Caucasian origin, with L. crispatus and L. gasseri being the most frequently found species, followed by L. jensenii and L. rhamnosus. Petricevic et al. [6] identified five leading Lactobacillus spp. in the vaginal microbiome of pregnant women: L. crispatus, L. iners, L. gasseri, L. johnsonii, and L. jensenii. In our study L. iners was not identified. Lactobacillus iners grows on blood agar and is uncultivatable on MRS agar, in contrast with other lactobacilli that grow readily on MRS agar. In our study, lactobacilli were isolated only by cultivation, in contrast with other studies where genetic methods, independent of cultivation, were used for identification purposes. This may explain why L. iners was not detected in our study.
Antimicrobial activity of isolates is considered as a significant criterion for probiotic strain selection. The majority of isolates showed medium or high inhibitory activity against the pathogenic bacteria tested. All strains inhibited growth of Str. agalactiae MK 14E. Streptococcus agalactiae can colonize newborns during delivery and can cause fetal sepsis [6]. Our vaginal isolates therefore have the potential to decrease the number of Str. agalactiae in pregnant women and to decrease the risk of fetal sepsis. All isolates were able to inhibit G. vaginalis DSMZ 104275, the bacteria associated with bacterial vaginosis, and almost all isolates also showed inhibitory activity against bacteria that are usually associated with aerobic vaginitis, such as E. coli and S. aureus. Aerobic vaginitis and bacterial vaginosis appear to be linked with spontaneous miscarriage, premature rupture of membranes, and increased risk of preterm birth [21, 22].
Some strains of vaginal lactobacilli inhibit the growth of Candida spp. [23]. Our results show that the highest inhibitory activity occurred with strains of L. crispatus, L. fermentum, and L. rhamnosus. These results are in accordance with the study of Strus et al. [23], where strains of L. fermentum and L. rhamnosus showed partial or total inhibition of Candida growth. Hütt et al. [24] tested antagonistic activity of L. crispatus, L. gasseri, and L. jensenii against C. albicans and C. glabrata. In that study, L. crispatus showed substantially higher antagonistic activity than L. gasseri and L. jensenii. In general, inhibitory activity of lactobacilli decreased in the order C. albicans, C. glabrata, and C. parapsilosis.
Hydrogen peroxide is an antimicrobial substance produced by certain strains of vaginal lactobacilli. These lactobacilli play a significant role, especially in the vaginal tract of pregnant women. Hydrogen peroxide has a protective effect against catalase-negative microorganisms such as G. vaginalis, which cause bacterial vaginosis [4, 25]. Hydrogen peroxide producing strains are responsible for maintaining microbial balance and their absence is associated with the development of bacterial vaginosis [2, 18]. In this study, we found that 71% of isolates were able to produce hydrogen peroxide, especially strains of L. crispatus, L. gasseri, and L. jensenii. Rabe and Hillier [26] also observed production of hydrogen peroxide by the same vaginal lactobacilli. Bouridane et al. [25] tested 70 isolates and 57 of them (81.42%) were able to produce hydrogen peroxide.
Lactic acid is an antimicrobial compound produced by lactobacilli as the main product of carbohydrate fermentation. Lactic acid maintains vaginal pH at values 3.5–4.5 and inhibits growth of pathogenic microorganisms [17]. Production of lactic acid is strain specific. In a previous study, the best lactic acid producers were strains of L. gasseri [24]. In our study, the highest concentration of lactic acid was detected for strain L. rhamnosus 72A, which was followed by strains of L. crispatus.
It is very important to know the antibiotic susceptibility of vaginal lactobacilli, because resistance to an antibiotic can be considered as advantageous. A resistant strain can be administered together with a vaginal drug and the strain can start colonizing the urogenital mucosa [25, 27]. In our study, it was determined that all strains were resistant to metronidazole and fluconazole. Usually, metronidazole is used to treat bacterial vaginosis [16, 28]. Thus, these strains could be co-administrated with these antibiotics during treatment of bacterial vaginosis.
Adherence to vaginal cells is one antimicrobial mechanism. A previous study showed that there was a correlation between adhesion to the vaginal tissue and auto-aggregation [29]. Auto-aggregation can correlate with hydrophobicity [27, 30], but in our study, this correlation was not proven. Generally, strain diversity was detected for each property tested.
For future testing, six strains with appropriate functional properties were selected. Strains L. crispatus 46B and L. crispatus 69E were capable of substantial production of hydrogen peroxide, strong auto-aggregation, and high or medium anti-Candida activity. High antibacterial activity against all indicator pathogenic microorganisms was proven for strains L. rhamnosus 10A, L. fermentum 74A, and L. fermentum 74B. Relatively satisfactory properties were determined for strain L. gasseri 8D, which showed high hydrogen peroxide production, strong auto-aggregation, and high inhibitory activity against G. vaginalis and Str. agalactiae. Thus, these lactobacilli isolates could be appropriate candidates on the base of their stability and properties according to Romero et al. [19], where higher stability of lactobacilli from pregnant women was detected. On the other hand, Romero et al. [19] compared isolates from pregnant women with isolates from non-pregnant women. This comparison has not been done in our study, so it could be little limitation of our research. Also, weaknesses of this study may be that all tested properties were determine only in vitro and lactobacilli may show a little bit different property in the real system of vaginal tract. Therefore, it is necessary to subject selected strains for clinical trials.
In conclusion, lactobacilli are important for maintaining the normal environment of the vaginal tract. Lactobacilli isolated in our study have a promising potential for future use and six selected strains (L. crispatus 46B and 69E, L. fermentum 74A and 74B, L. gasseri 8D, L. rhamnosus 10A) could be potential probiotic candidates for clinical trials. They could be used for preparation of probiotic products for treatment and prevention of vulvovaginal infections, especially for pregnant women with abnormal microbiome to reduce risk of preterm birth or neonatal infection causes by Streptococcus agalactiae. The advantage of lactobacilli isolated from the vaginal tract of pregnant women is the increased chance of their later adhesion and colonization of the tract since this represents a transfer back to their natural environment. They can also be potentially used in non-pregnant women as a replacement for antibiotic therapy of vulvovaginal infections.
References
Granato P (2006) Microbial flora of humans and microbial virulence factors. In: Wooley D, Byers K (eds) Biological safety: principles and practices. ASM Press, Washington, pp 3–17
Borges S, Silva J, Teixeira P (2014) The role of lactobacilli and probiotics in maintaining vaginal health. Arch Gynecol Obstet 289:479–489. https://doi.org/10.1007/s00404-013-3064-9
Boris S, Barbés C (2000) Role played by lactobacilli in controlling the population of vaginal pathogens. Microbes Infect 2:543–546. https://doi.org/10.1016/S1286-4579(00)00313-0
DiGiulio DB, Callahan BJ, McMurdie PJ, Costello EK, Lyell DJ, Robaczewska A, Sun CL, Goltsman DSA, Wong RJ, Shaw G, Stevenson DK, Holmes SP, Relman DA (2015) Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci U S A 112:11060–11065. https://doi.org/10.1073/pnas.1502875112
Walther-António MRS, Jeraldo P, Berg Miller ME, Yeoman CJ, Nelson KE, Wilson BA, White BA, Chia N, Creedon DJ (2014) Pregnancy’s stronghold on the vaginal microbiome. PLoS One 9:1–10. https://doi.org/10.1371/journal.pone.0098514
Petricevic L, Domig KJ, Nierscher FJ, Sandhofer MJ, Fidesser M, Krondorfer I, Husslein P, Kneifel W, Kiss H (2014) Characterisation of the vaginal Lactobacillus microbiota associated with preterm delivery. Sci Rep 4:1–6. https://doi.org/10.1038/srep05136
Farr A, Kiss H, Hagmann M, Machal S, Holzer I, Kueronya V, Husslein PW, Petricevic L (2015) Role of Lactobacillus species in the intermediate vaginal flora in early pregnancy: a retrospective cohort study. PLoS One 10:1–12. https://doi.org/10.1371/journal.pone.0144181
Park JS, Park CW, Lockwood CJ, Norwitz ER (2005) Role of cytokines in preterm labor and birth. Minerva Ginecol 57:349–366
Nuriel-Ohayon M, Neuman H, Koren O (2016) Microbial changes during pregnancy, birth, and infancy. Front Microbiol 7:1–13. https://doi.org/10.3389/fmicb.2016.01031
Boldenow E, Gendrin C, Ngo L, Bierle C, Vornhagen J, Coleman M, Merillat S, Armistead B, Whidbey C, Alishetti V, Santana-Ufret V, Ogle J, Gough M, Srinouanprachanh S, MacDonald JW, Bammler TK, Bansal A, Liggitt HD, Rajagopal L, Adams Waldorf KM (2016) Group B Streptococcus circumvents neutrophils and neutrophil extracellular traps during amniotic cavity invasion and preterm labor. Sci Immunol 1:1–13. https://doi.org/10.1126/sciimmunol.aah4576
Borges S, Silva J, Teixeira P (2012) Survival and biofilm formation by group B streptococci in simulated vaginal fluid at different pHs. Antonie Leeuwenhoek 101:677–682. https://doi.org/10.1007/s10482-011-9666-y
Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, Frances Coach M, Edelman R, Pastorek JG, Vijaya Rao A, McNellis D, Regan JA, Carey C, Klebanoff MA (1995) Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. N Engl J Med 333:1737–1742. https://doi.org/10.1056/NEJM199512283332604
Borges S, Barbosa J, Teixeira P (2016) Gynecological health and probiotics. In: Watson RR, Preedy VR (eds) Probiotics, prebiotics, and synbiotics - bioactive foods in health promotion. Elsevier, London, pp 741–752
Boris S, Suárez JE, Vázquez F, Barbés C (1998) Adherence of human vaginal lactobacilli to vaginal epithelial cells and interaction with uropathogens. Infect Immun 66:1985–1989
Verdenelli MC, Coman MM, Cecchini C, Silvi S, Orpianesi C, Cresci A (2014) Evaluation of antipathogenic activity and adherence properties of human Lactobacillus strains for vaginal formulations. J Appl Microbiol 116:1297–1307. https://doi.org/10.1111/jam.12459
Reid G (2001) Probiotic agents to protect the urogenital tract against infection. Am J Clin Nutr 78:437–443. https://doi.org/10.1093/ajcn/73.2.437s
Lalan MS, Misra A (2011) Applications of polymers in vaginal drug delivery. In: Misra A, Shahiwala A (eds) Applications of polymers in drug delivery. Smithers Rapra, Shawbury, pp 351–377
Amin M, Goodarzi H, Orang Z, Farsi S, Jorfi M (2011) Isolation and identification of Lactobacillus species from the vagina and their antimicrobial properties. Afr J Microbiol Res 5:3300–3304. https://doi.org/10.5897/AJMR11.481
Romero R, Hassan SS, Gajer P, Tarca AL, Fadrosh DW, Nikita L, Galuppi M, Lamont RL, Chaemsaithong P, Miranda J, Chaiworapongsa T, Ravel J (2014) The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome 4:1–19. https://doi.org/10.1186/2049-2618-2-4
Kiss H, Kögler B, Petricevic L, Sauerzapf I, Klayraung S, Domig K, Viernstein H, Kneifel W (2007) Vaginal Lactobacillus microbiota of healthy women in the late first trimester of pregnancy. BJOG 114:1402–1407. https://doi.org/10.1111/j.1471-0528.2007.01412.x
Rosenstein IJ, Morgan DJ, Sheehan M, Lamont RF, Taylor-Robinson D (1996) Bacterial vaginosis in pregnancy: distribution of bacterial species in different gram-stain categories of the vaginal flora. J Med Microbiol 45:120–126. https://doi.org/10.1099/00222615-45-2-120
Donders GGG, Bellen G, Grinceviciene S, Ruban K, Vieira-Baptista P (2017) Aerobic vaginitis: no longer a stranger. Res Microbiol 168:845–858. https://doi.org/10.1016/j.resmic.2017.04.004
Strus M, Kucharska A, Kukla G, Brzychczy-Wloch M, Maresz K, Heczko PB (2005) The in vitro activity of vaginal Lactobacillus with probiotic properties against Candida. Infect Dis Obstet Gynecol 13:69–75. https://doi.org/10.1080/10647440400028136
Hütt P, Lapp E, Štšepetova J, Smidt I, Taelma H, Borovkova N, Oopkaup H, Ahelik A, Rööp T, Hoidmets D, Samuel K, Salumets A, Mändar R (2016) Characterisation of probiotic properties in human vaginal lactobacilli strains. Microb Ecol Health Dis 27:1–9. https://doi.org/10.3402/mehd.v27.30484
Bouridane H, Sifour M, Idoui T, Annick L, Thonard P (2016) Technological and probiotic traits of the lactobacilli isolated from vaginal tract of the healthy women for probiotic use. Iran J Biotech 14:192–201. https://doi.org/10.15171/ijb.1432
Rabe LK, Hillier SL (2003) Optimization of media for detection of hydrogen peroxide production by Lactobacillus species. J Clin Microbiol 41:3260–3264. https://doi.org/10.1128/JCM.41.7.3260-3264.2003
Kaewnopparat S, Dangmanee N, Kaewnopparat N, Srichana T, Chulasiri M, Settharaksa S (2013) In vitro probiotic properties of Lactobacillus fermentum SK5 isolated from vagina of a healthy woman. Anaerobe 22:6–13. https://doi.org/10.1016/j.anaerobe.2013.04.009
Anukam KC, Reid G (2008) Effects of metronidazole on growth of Gardnerella vaginalis ATCC 14018, probiotic Lactobacillus rhamnosus GR-1 and vaginal isolate Lactobacillus plantarum KCA. Microb Ecol Health Dis 20:48–52. https://doi.org/10.1080/08910600701837964
Malik S, Petrova MI, Claes IJJ, Verhoeven TLA, Busschaert P, Vaneechoutte M, Lievens B, Lambrichts I, Siezen RJ, Balzarini J, Vanderleyden J, Lebeer S (2013) The highly autoaggregative and adhesive phenotype of the vaginal Lactobacillus plantarum strain CMPG5300 is sortase dependent. J Appl Environ Microbiol 79:4576–4585. https://doi.org/10.1128/AEM.00926-13
Kos B, Šuškovic J, Vukovic S, Šimpraga M, Frece J, Matošic S (2003) Adhesion and aggregation ability of probiotic strain Lactobacillus acidophilus M92. J Appl Microbiol 94:981–987. https://doi.org/10.1046/j.1365-2672.2003.01915.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Sample collecting was approved by the Ethics Committee of the General University Hospital, Prague.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumherová, M., Veselá, K., Kosová, M. et al. Novel Potential Probiotic Lactobacilli for Prevention and Treatment of Vulvovaginal Infections. Probiotics & Antimicro. Prot. 13, 163–172 (2021). https://doi.org/10.1007/s12602-020-09675-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-020-09675-2