Abstract
Lack of elasticity in the central artery causes an increase in left ventricular (LV) afterload. Although regular moderate-intensity endurance exercise improves cardiovascular function, including arterial destiffening, little is known about the effect of short-term vigorous exercise on cardiovascular function (i.e., the interaction between cardiac and arterial functions). We measured arterial stiffness [via pulse wave velocity from the heart to ankle (haPWV)] and LV contractility (via systolic interval time) before and after a 1-week training camp in a total of 33 regularly highly-trained collegiate endurance runners. They participated in three training sessions per day which mainly consisted of long-distance running and sprint training. The averaged running distance was ≈44 % longer during the camp than the regular training program. After the camp, heart rate at rest and haPWV were significantly increased, whereas blood pressure remained unchanged. Although a ratio of pre-ejection period and LV ejection time (PEP/LVET, an index of blunted LV contractility) was unaltered, presumably due to the large variability of individual response, there was a significant correlation between changes in haPWV and PEP/LVET (r = 0.54, P < 0.01). These results suggest that, in regularly highly-trained endurance athletes, arterial stiffness increases after a training camp characterized by greater training volume (vs. regular training), and that the individual response in arterial stiffness correlates with the corresponding changes in myocardial contractility.
Similar content being viewed by others
Introduction
There is increasing recognition that the elastic proximal aorta has an important role to expand and retract with repetitive blood flow ejection from the left ventricular (LV) [1, 2]. It dampens and confines the aortic pressure fluctuations to the larger arteries. The impairment of such a function (e.g., arterial stiffening) results in a greater reflected wave from the periphery, which induces excessive elevations of LV afterload causing extra myocardium work. Previous studies have reported that higher physical conditioning status, indexed by maximal and sub-maximal aerobic capacity, is associated with reduced arterial stiffness, and vice versa [3, 4]. Therefore, arterial stiffening might be unfavorable for aerobic performance because of excessive myocardium work.
It is well known that regular endurance training improves cardiovascular function, including arterial destiffening [5]. However, a few studies have suggested that highly-trained marathon runners exhibit higher stiffness of the central artery compared with physiologically active controls [6, 7], suggesting the possibility of a chronic increase in arterial stiffness by regular intense exercise training. Regarding acute influence (i.e., single exhaustive exercise bout), Vlachopoulos et al. [7] reported that arterial stiffness did not change immediately after a full marathon race in regularly trained marathon runners, but that unchanged arterial stiffness might be attributed to post-exercise hypotension. Therefore, the effect of a single bout of exhaustive exercise on arterial stiffness is not fully known. Furthermore, little is known about the impact of short-term repeated bouts of vigorous exercise on arterial stiffness. In addition, although strenuous prolonged exercise may acutely depress LV contractile function [8, 9], the influence of such intense exercise on the interaction between arterial stiffness and LV contractility (i.e., ventricular–arterial coupling) remains to be identified.
In this study, we hypothesized that short-term vigorous endurance training increased central arterial stiffness even in regularly highly-trained endurance runners, and that the increased central arterial stiffness was associated with the decrease in LV contractility. To test these hypotheses, we evaluated arterial stiffness and LV contractility before and after a 1-week summer training camp characterized by a greater training volume (vs. regular training) in highly-trained collegiate endurance runners.
Methods
Subjects
We studied a total of 33 elite collegiate endurance runners in Japan (male, 19 ± 1 years, and 171 ± 5 cm). Their averaged best time for a 5000-m race was 14′29″ ± 0′17″. All the subjects were healthy, normotensive (<140/90 mmHg), nonobese (BMI < 25 kg/m2), nonsmokers, free of medication and overt chronic heart and lung disease as assessed by their medical history. None of the subjects were taking cardiovascular-acting medication. This study was reviewed and approved by the Institutional Review Board (Toyo University: 2012-R-04). Additionally, all procedures conformed to the ethical guidelines of the Helsinki Declaration. Informed written consent was obtained from all subjects prior to participation.
Experimental protocol
One day before and 1 day after a 1-week summer training camp, all measurements were performed in the supine position in a quiet air-conditioned room (24–25 °C) after overnight fasting, and more than 10 min quiet resting, at the same time of day in the morning. Subjects abstained from alcohol for 24 h and caffeine for 10 h prior to the experiment.
Measurements
Heart rate (HR), blood pressure (BP), pulse wave velocity (PWV) (e.g., an inverse index of arterial compliance), and systolic interval time (e.g., an index of LV contractility) were measured by an automated polygraph apparatus (form PWV/ABI; Omron-Colin, Kyoto, Japan) equipped with an electrocardiogram (ECG), a phonocardiogram (PCG), an applanation tonometry sensor, and extremities cuffs connected to an oscillometric pressure sensor and a plethysmographic sensor. PWV from the aortic annulus (e.g., heart) to ankle (haPWV) and between brachium and ankle (baPWV) were measured in the supine position after a supine resting of at least 15 min, as previously reported [10, 11]. Briefly, ECG, PCG (via a microphone placed on the left edge of the sternum), left carotid arterial pressure waveform (via applanation tonometry sensor), and arterial pressure waveforms of right brachial and both posterior-tibial arteries (via air-plethysmographic sensors) were simultaneously recorded. The characteristic points of ECG, PCG, and pressure waveforms were automatically detected by a band-pass filter. haPWV and baPWV were calculated by the following equations [12]:
where L ha is the arterial path length from the aortic annulus to the midpoint of the right ankle cuff estimated by the subjects height [e.g., 0.8129 × height (in cm) + 12.328], L hb is the arterial path length from the aortic annulus to the midpoint of right brachial cuff estimated by the subjects height [0.2195 × height (in cm) − 2.0734), T hb is the time interval between the commencement of the second heart sound and the dicrotic notch on the right brachial arterial pressure wave, and T ba is the “foot-to-foot” time interval between brachial and posterior-tibial arterial pressure waves, respectively.
For evaluation of left ventricular contractility, the duration of the phases of LV systole was automatically measured from simultaneous recordings of ECG, PCG, and the carotid arterial pulse waveforms. The following phases of the cardiac cycle were measured: (1) the total electro-mechanical systolic interval (QS2) was measured from the onset of the QRS complex to the second heart sound; (2) the LV ejection time (LVET) was measured from the beginning upstroke to the trough of the dicrotic notch of the carotid arterial pressure waveforms, and (3) the pre-ejection period (PEP) was calculated by subtracting LVET from the QS2 interval. A ratio of PEP/LVET was defined as an inverse index of LV contractility [13].
Training camp
The training camp was conducted in August, 2013. Although each subject regularly engaged in long-distance running, the weekly running distance during the camp was relatively longer (179 ± 55 km/week) than the regular training program (124 ± 48 km/week) right before the start of the camp. During the camp, athletes were required to attend three practice session per day; 1st session (0530–0730 hours), athletes mainly performed long distance running (15–18 km); 2nd session (0830–1230 hours) consisted of long-distance running and basic core and lower body strength training; 3rd session (1400–1830 hours) consisted mainly of speed development training such as repetition of 400-m sprints.
Statistics
Student’s paired t test was performed to compare variables of interest before and after the training camp. Product-moment correlation analysis was applied to determine the relationships among these changes (e.g., from before to after the camp). All data are reported as mean ± SD. All comparisons were based on a 95 % confidence limit with P < 0.05 considered statistically significant.
Results
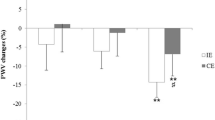
Changes in selected physiological characteristics are shown in Table 1. Excessive body weight losses indicating dehydration were not seen after the 1-week training camp. More than 60 % of subjects exhibited an increase in HR. Therefore, the averaged increase in HR was slight but significant. Conversely, LVET was significantly decreased after the camp. Significant alterations were not seen in systolic and diastolic BP, pulse pressure, PEP, QS2, and PEP/LVET. haPWV (Pre: 676 ± 55 vs. Post: 694 ± 54 cm/s, P < 0.05) and baPWV (Pre: 987 ± 129 vs. Post 1015 ± 125 cm/s, P < 0.05) were significantly increased (Fig. 1). The change value in haPWV was 18 ± 50 cm/s and baPWV was 28 ± 71 cm/s.
Changes in HR did not correlated significantly with changes in either haPWV (r = 0.09, ns) or baPWV (r = −0.001, ns). Changes in LVET significantly correlated with corresponding changes in haPWV (r = −0.62, P = 0.0001) but not with changes in baPWV (r = −0.26, ns). Changes in PEP/LVET significantly correlated with corresponding changes in haPWV (r = 0.54, P < 0.01, Fig. 2) but not in baPWV (r = 0.25, ns). Difference in running distance between normal training and training camp did not correlated with changes in either haPWV (r = −0.16, ns) or baPWV (r = −0.07, ns).
Discussion
The major findings of the present study are that, in regularly highly-trained endurance athletes, arterial stiffness increased significantly after a training camp which was characterized by relatively higher-intensity exercise and greater training volume (i.e., longer running distance) than normal, and that the individual changes in arterial stiffness correlated with the corresponding changes in myocardial contractility
To the best of our knowledge, this is the first study to demonstrate an increase in arterial stiffness after a short-term training camp mainly consisting of repeated bouts of high intensity and prolonged exercise. Although the precise mechanisms for arterial stiffening could not be clarified, they might be attributed to changes in the functional elements rather than structural ones because the change was for a short period. Thereby, we are able to speculate about some possible mechanisms. First, the intense exercise training-induced systemic inflammation might raise arterial stiffness. Barnes et al. [14] demonstrated that acute limb eccentric exercise induced systemic inflammation, which was associated with the delayed increase in central arterial stiffness (i.e., 48 h after the exercise). In the present study, the training distance during the camp was substantially longer than normal. Running movement involves both concentric and eccentric muscle contractions. Note that the intrinsic eccentric component of running, especially downhill, has the potential for high levels of inflammation from high volume exposure [15]. With regard to this, Vlachopoulos et al. [7] investigated the acute effect of full marathons on arterial stiffness in regularly trained marathon runners. Fifteen minutes after the full marathon race, BP was significantly lowered but aortic PWV did not change compared with those before the race. Unchanged arterial stiffness might be explained by not only the postexercise hypotension but also the small effect of inflammation; the inflammatory response is gradually enhanced following an intense exercise bout (i.e., eccentric exercise) and archives peak approximately 48 h after the event. Taken together, it is plausible that vigorous training-induced muscle damage leads to systemic inflammation and may contribute to an increase in arterial stiffness.
Another possible mechanism is the increase in sympathetic vasoconstrictor tone. The compliance of central and peripheral conduit arteries is regulated tonically by the sympathetic nervous system. Thus, the removal of sympathetic nervous activity produces an increase in arterial compliance [16, 17]. Conversely, arterial compliance is reduced by an increased sympathetic drive such as a cold presser test and mental arithmetic [18, 19]. Several studies [20, 21] have demonstrated that overload training causes an imbalance of the autonomic nervous system tone toward a predominance of sympathetic activity. Therefore, the change in the sympathetic/vagal activity balance might be associated with the alteration of arterial stiffness via sympathetic vasoconstrictor tone.
It should be emphasized that individual responses of haPWV, but not baPWV, were positively associated with changes in the PEP/LVET ratio, an index of blunted LV contractility; haPWV in fact decreased in some runners but was also accompanied by a reduction in PEP/LVET ratio, although it did not alter significantly presumably due to the large variability of individual responses. These phenomena are of physiological importance because haPWV but not baPWV includes the central elastic artery (i.e., the ascending aorta). Thus, these results suggest that the extent of LV contractility change could be partly explained by individual responses of central arterial stiffness.
In the present study, we could not identify the relationship between changes in training volume (i.e., increase in running distance) and PWV. These findings might suggest that the dose–response varies among athletes. On the other hand, as we did not obtain the data reflecting exercise intensity, such as exercise HR, the impact of exercise intensity during the camp remains to be identified.
Training programs of elite athletes are planned with the repetition of training cycles composed of intense training periods followed by a shorter recovery period, such as the repetition of over-reaching and supercompensation. The imbalance between training and recovery can lead to an advanced fatigue state (i.e., the overtraining syndrome). In athletic conditioning, therefore, useful markers to detect fatigue are needed for the prevention of overtraining for athletes [22, 23]. For example, substantial body weight loss reflects dehydration or overtraining. In addition, high resting HR and BP and low resting HR and BP are well-known symptoms of sympathetic-type and parasympathetic-type overtraining syndromes. In this study, no subject exhibited such symptoms. In this context, our findings of (1) the increase in arterial stiffness without substantial HR and BP changes and (2) the association between arterial stiffness and myocardial contractility responses may have important implications for athletic conditioning.
However, in addition to no observations during regular training periods, we did not follow up the recovery of impaired arterial compliance and LV contractility after the training camp period. Furthermore, in this investigation, we did not evaluate concomitant changes in biochemical parameters (i.e., inflammation biomarker) nor aerobic capacity or exercise performance. To confirm if haPWV might be acceptable as an early predictor of blunted myocardial contractility, further investigations, such as monitoring intra-individual variability of arterial compliance, LV contractility, and exercise performance throughout the training period, are warranted to confirm the usefulness of haPWV for athletic conditioning.
A methodological limitation should be mentioned. Based on the physiological role of central artery properties (e.g., extension and retraction), we hypothesized that increased arterial stiffness induced the blunted LV contractility. However, the product–moment correlation analysis could not rule out the possibility that the training camp elicited malfunctions of heart and artery, separately.
In conclusion, in regularly highly-trained endurance athletes, arterial stiffness increased significantly after a training camp characterized by greater training volume (vs. regular training), and that the individual changes in arterial stiffness correlated with the extent of change in LV contractility. These results suggest that the extent of LV contractility change could be partly explained by individual responses of central arterial stiffness.
References
Nichols WW, McDonald DA (2011) McDonald’s blood flow in arteries : theoretic, experimental, and clinical principles, 6th edn. Hodder Arnold, London
Safar ME, London GM (2000) Therapeutic studies and arterial stiffness in hypertension: recommendations of the European Society of Hypertension. The Clinical Committee of Arterial Structure and Function. Working Group on Vascular Structure and Function of the European Society of Hypertension. J Hypertens 18:1527–1535
Vaitkevicius PV, Fleg JL, Engel JH, O’Connor FC, Wright JG, Lakatta LE, Yin FC, Lakatta EG (1993) Effects of age and aerobic capacity on arterial stiffness in healthy adults. Circulation 88:1456–1462
Otsuki T, Maeda S, Sugawara J, Kesen Y, Murakami H, Tanabe T, Miyauchi T, Kuno S, Ajisaka R, Matsuda M (2006) Age-related reduction of systemic arterial compliance relates to decreased aerobic capacity during sub-maximal exercise. Hypertens Res 29:759–765
Hayashi K, Sugawara J, Komine H, Maeda S, Yokoi T (2005) Effects of aerobic exercise training on the stiffness of central and peripheral arteries in middle-aged sedentary men. Jpn J Physiol 55:235–239
Burr JF, Drury CT, Phillips AA, Ivey A, Ku J, Warburton DE (2014) Long-term ultra-marathon running and arterial compliance. J Sci Med Sport 17:322–325
Vlachopoulos C, Kardara D, Anastasakis A, Baou K, Terentes-Printzios D, Tousoulis D, Stefanadis C (2010) Arterial stiffness and wave reflections in marathon runners. Am J Hypertens 23:974–979
Aslani A, Babaee Bigi MA, Moaref AR (2009) Effect of extreme exercise on myocardial function as assessed by tissue Doppler imaging. Echocardiography 26:1036–1040
Douglas PS, O’Toole ML, Hiller WD, Hackney K, Reichek N (1987) Cardiac fatigue after prolonged exercise. Circulation 76:1206–1213
Kim WJ, Park CY, Park SE, Rhee EJ, Lee WY, Oh KW, Park SW, Kim SW, Song S (2012) The association between regional arterial stiffness and diabetic retinopathy in type 2 diabetes. Atherosclerosis 225:237–241
Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA, Tanaka H (2005) Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens 19:401–406
Kimoto E, Shoji T, Shinohara K, Inaba M, Okuno Y, Miki T, Koyama R, Emoto M, Nishizawa Y (2003) Preferential stiffening of central over peripheral arteries in type 2 diabetes. Diabetes 52:448–452
Weissler AM, Garrard CL Jr (1971) Systolic time intervals in cardiac disease. I. Mod Concepts Cardiovasc Dis 40:1–4
Barnes JN, Trombold JR, Dhindsa M, Lin HF, Tanaka H (2010) Arterial stiffening following eccentric exercise-induced muscle damage. J Appl Physiol 109:1102–1108
Schiff HB, MacSearraigh ET, Kallmeyer JC (1978) Myoglobinuria, rhabdomyolysis and marathon running. Q J Med 47:463–472
Failla M, Grappiolo A, Emanuelli G, Vitale G, Fraschini N, Bigoni M, Grieco N, Denti M, Giannattasio C, Mancia G (1999) Sympathetic tone restrains arterial distensibility of healthy and atherosclerotic subjects. J Hypertens 17:1117–1123
Mangoni AA, Mircoli L, Giannattasio C, Mancia G, Ferrari AU (1997) Effect of sympathectomy on mechanical properties of common carotid and femoral arteries. Hypertension 30:1085–1088
Boutouyrie P, Lacolley P, Girerd X, Beck L, Safar M, Laurent S (1994) Sympathetic activation decreases medium-sized arterial compliance in humans. Am J Physiol 267:H1368–H1376
Perret F, Mooser V, Waeber B, Yanik T, Jean-Jacques M, Mooser E, Nussberger J, Brunner HR (1989) Effect of cold pressor test on the internal diameter of the radial artery. Am J Hypertens 2:727–728
Pichot V, Busso T, Roche F, Garet M, Costes F, Duverney D, Lacour JR, Barthelemy JC (2002) Autonomic adaptations to intensive and overload training periods: a laboratory study. Med Sci Sports Exerc 34:1660–1666
Pichot V, Roche F, Gaspoz JM, Enjolras F, Antoniadis A, Minini P, Costes F, Busso T, Lacour JR, Barthelemy JC (2000) Relation between heart rate variability and training load in middle-distance runners. Med Sci Sports Exerc 32:1729–1736
Johnson MB, Thiese SM (1992) A review of overtraining syndrome-recognizing the signs and symptoms. J Athl Train 27:352–354
Lehmann MJ, Lormes W, Opitz-Gress A, Steinacker JM, Netzer N, Foster C, Gastmann U (1997) Training and overtraining: an overview and experimental results in endurance sports. J Sports Med Phys Fit 37:7–17
Acknowledgments
We thank all subjects of this study and their team staffs.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tomoto, T., Sugawara, J., Hirasawa, A. et al. Impact of short-term training camp on arterial stiffness in endurance runners. J Physiol Sci 65, 445–449 (2015). https://doi.org/10.1007/s12576-015-0383-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-015-0383-6