Abstract
Fabry disease resulting from a deficiency of α-galactosidase A leads to the accumulation of globotriaosylceramide in various organs. Because the disease is an X-linked recessive disorder, males tend to develop more symptoms and more severe symptoms than females. There are also some variants of Fabry disease, and cardiac variant (cardiac Fabry disease) has the dysfunctions only in heart. Cardiac manifestations in Fabry disease are initially symmetrical and concentric left ventricular hypertrophy, and later progressive cardiac dysfunction with localized thinning of the basal posterior wall. In recent years, enzyme replacement therapy has been performed as a treatment for Fabry disease, and the initiation of this therapy is expected before the cardiac fibrosis develops. Therefore, early diagnosis of Fabry disease is essential, and echocardiography is an indispensable tool for clinical practice of this disease. Then, it is necessary to remember this disease as a differential diagnosis when encountering unexplained left ventricular hypertrophy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fabry disease, which is a lysosomal storage disease resulting from a deficiency of α-galactosidase A (α-Gal A), leads to the accumulation of globotriaosylceramide (Gb3) in skin, eye, heart, kidney, brain, vascular, and nervous systems. Clinical symptoms include painful extremities related to peripheral neuropathy, angiokeratoma, adiaphoresis, corneal opacities, auditory disturbance, renal disease, cerebrovascular disease, cardiac hypertrophy, and fatal arrhythmia. Because its heredity indicates an X-linked recessive disorder, males tend to develop more symptoms, and more severe symptoms, than females.
A cardiac variant of Fabry disease (cardiac Fabry disease), whose manifestations are limited to the heart, has been known and patients with this variant type of the disease have residual α-Gal A activity whereas it is a deficit in classic Fabry disease [1]. In both cardiac and classic Fabry diseases classified to secondary cardiomyopathy [2], the cardiac manifestations are initially cardiac hypertrophy, but later show progressive cardiac dysfunction with localized thinning of the basal posterior wall.
In recent years, enzyme replacement therapy (ERT) has been performed as a treatment for Fabry disease [3]. The initiation of this therapy is expected before the cardiac fibrosis develops. Therefore, early diagnosis of the disease is essential, and echocardiography [4] is an indispensable tool for clinical practice of this disease.
Epidemiology
Classic Fabry disease is considered to be an extremely rare disease of 1/40,000 to 1/60,000 men [5]. Due to the activity of α-Gal A in lysosome decreases, glycosphingolipid materials progressively accumulate to various organs and damage them. Fabry disease is inherited in an X-chromosome recessive heredity form, then it is a male that usually develop organ disorders, while the female becomes the carrier. However, cardiac involvement in Fabry disease may be seen even in heterozygous females when age advances [6, 7]. This is different from other X-linked recessive disorders including hemophilia.
The subtype where the accumulation of glycosphingolipid material is seen only in the heart is reported as cardiac Fabry disease, and it is found in approximately 3% of patients with left ventricular hypertrophy (LVH) and may not be a rare disease [1]. Table 1 shows the differences between classic and cardiac Fabry disease [8].
Clinical manifestations
In classic Fabry disease, a painful sensation in the extremities usually occurs prior to other symptoms in childhood or adolescence [5]. Symptoms including adiaphoresis and angiokeratoma, corneal opacities (cornea verticillata), hearing loss, and abdominal pain are seen as clinical findings in the early stage of classic Fabry disease. In accordance with the progression, the additional symptoms from cardiovascular, renal, and cerebrovascular disorders occur at a later stage.
In cardiac Fabry disease, patients with this variant type of the disease have residual α-Gal A activity, whereas it is a deficit in classic Fabry disease. It has been thought that this is one of the reasons why clinical manifestations of cardiac Fabry disease develop later than in classic Fabry disease.
LV diastolic dysfunction and LVH are observed to occur by around 40 years old. Thereafter, cardiac function decreases progressively with basal posterior wall thinning. The atrioventricular (AV) block by the glycosphingolipid accumulation to AV conducting system and lethal arrhythmia are also seen in the advanced stage [9].
In females heterozygous for Fabry disease, they should no longer be considered as asymptomatic carriers [10]. Clinical manifestations in females are similar but more variable, and show slower progression than males.
Diagnostic approach in Fabry disease
Figure 1 shows the algorithm for the diagnosis of Fabry disease. The assessment of the α-Gal A enzyme activity is essential for the diagnosis of Fabry disease, but the enzyme activity may become moderately decreased or around a threshold. Additional general evaluations are required including urinary Gb3 assay, genetic screening, and biopsy for a definitive diagnosis. Because of the disease characteristics with X-linked disorder, familial investigation is also important if a patient is diagnosed as having Fabry disease. A female whose father is diagnosed with Fabry disease (hemizygote) is a carrier (heterozygote) with 100% of probability, and each male and female can become hemi- and heterozygote with 50% of probability when their mother is a heterozygote.
Histological findings
The pathological evidence of Fabry disease is the accumulation of Gb3 to cells of systematic organs including skin, nervous systems, kidney, and heart. In cardiac involvement, accumulation of Gb3 occurs in cardiomyocytes, conduction system cells, valvular fibroblasts, endothelial cells, and vascular smooth muscle cells [5].
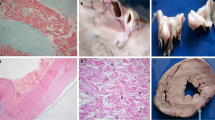
Figure 2 shows microscopic findings of hearts from patients with cardiac Fabry disease. Sarcoplasmic vacuolization of myocardial cells and diffuse fibrosis are seen in the septal wall, and marked fibrosis with almost no myocardial cells is seen in thin lesion of the LV posterior wall [11].
Cardiac histology in Fabry disease. Hematoxylin and eosin dyeing (×100): Sarcoplasmic vacuolization of myocardial cells and diffuse fibrosis are seen in the septal wall, and marked fibrosis with almost no myocardial cells is seen in thin lesion of the LV posterior wall. Toluidine—blue dyeing (×400): accumulation of strongly osmiophilic substance (Gb3) is observed in myocardial cells [11]
Cardiac morphology and echocardiography
Early stage of Fabry disease
One of the first signs of cardiac involvement in electrocardiac findings in Fabry disease is PQ interval shortening due to shortening of the P-wave duration [12]. Further abnormalities are PQ- and QRS-interval prolongation, repolarization abnormalities, and atrio-ventricular block. High voltage in electrocardiogram is not rare findings in Fabry disease despite low voltage in cardiac amyloidosis [13].
Echocardiography is a useful tool for screening, diagnosis, and follow-up evaluation in Fabry disease. Particularly in patients with cardiac Fabry disease that usually has few abnormality except heart, unexplained LVH is a clue for suspecting this disease [1, 14, 15]. Various LVH patterns are observed in these patients, and severity and symmetricity of LVH depends on each patient and stage of the disease ( Fig. 3). The most popular morphological pattern in Fabry disease is concentric LVH, but concentric remodeling, asymmetric septal hypertrophy, eccentric or normal pattern are also observed occasionally [16]. In addition, a patient who has LV outflow tract obstruction mimicking hypertrophic obstructive cardiomyopathy is rarely seen [17].
Cases of Fabry disease (early to middle stage). Left ventricles show mild to moderate concentric left ventricular hypertrophy (LVH). The severity and symmetricity of hypertrophy depend on cases and stages of Fabry disease. Case 1 A 27-year-old male with mild and symmetrical LVH. Case 2 A 44-year-old male, severe and symmetrical LVH. Case 3 A 52-year-old male with moderate and asymmetrical LVH
There is a report indicating the usefulness of the specific “binary appearance” which is the endocardial doubled brightness by the composure of the glycosphingolipid [18]. However, recent study demonstrated the difficulty of the differentiation by using this finding [19, 20]. They reported that the binary endocardial appearance lacks sufficient sensitivity and specificity for echocardiographic screening tool in Fabry disease by comparing with hypertrophic cardiomyopathy.
Fabry disease causes cardiac dysfunction before LVH develops, and tissue Doppler imaging is useful for evaluating it [21]. Furthermore, the strain and strain-rate analysis by speckle tracking methods can identify the cardiac dysfunction by Fabry disease more accurately compared to other methods [22].
Progression of myocardium fibrosis of Fabry disease also has differences between genders. In male patients, myocardial fibrosis occurs after LVH develops. On the other hand, the occurrence of myocardial fibrosis in females is delayed by approximately 10 years compared to males, but does not necessarily require myocardial hypertrophy [23].
Left atrium in Fabry disease expands and decreases its compliance prior to showing LVH. This suggests the possibility of the direct influence on atrium by Fabry disease [24]. Valvular thickening has also been reported, but most lesions are mild and do not need specific cardiac surgery [25]. Right ventricular (RV) involvement in Fabry disease is observed with thickened RV and a decrease of longitudinal strain rate in RV free wall [26], although the changes are milder than LV. This may be due to the differences in the degree of glycosphingolipid accumulation by each segment of heart [11].
Advanced stage in Fabry disease
When a stage of Fabry disease progresses, the voltage of the QRS wave in the electrocardiogram decreases and the intervals of PR and QRS are prolonged. LV enlargement and diffuse hypokinesia with posterior wall thinning, mimicking dilated phase of hypertrophic cardiomyopathy, is known as typical cardiac morphology in an advanced stage of the disease (Fig. 4).
In cardiac Fabry disease, the severity of cardiac dysfunction determines their prognosis though various factors that affect their prognosis in classic Fabry disease. Our laboratory reported that LV posterior wall thinning is an important echocardiographic finding that precedes heart failure and cardiac death in patients with Fabry disease (Fig. 5) [27].

Reproduced from Ref. [25] and modified
Asymmetrical LV wall thinning precedes heart failure and cardiac death in patients with Fabry disease. Kaplan–Meier curves showing that ventricular septum/posterior wall thickness ratio (VSth/PWth) >1.3 significantly preceded NYHA class III CHF (a) and cardiac death (b) in patients with cardiac Fabry disease. VS ventricular septal wall thickness, PW posterior wall thickness, NYHA New York Heart Association, CHF chronic heart failure.
The role of echocardiography in the era of ERT
ERT in Fabry disease improves cardiac function and morphology [28,29,30]. Earlier initiation of ERT is desirable before irreversible cardiac changes such as fibrosis develops. Then, echocardiography has an important role in the early detection of this disease and is also useful for the curative effect judgment.
Conclusions
In clinical practice of the secondary cardiomyopathy such as Fabry disease, echocardiographic examination has important roles in screening, diagnosis, and evaluation of cardiac function or hemodynamics. Since ERT is usually performed as a fundamental treatment for Fabry disease, an earlier checkup is desirable to treat it. Furthermore, a diagnosis of one patient with the disease may lead to diagnose other familial involvements. Fabry disease should be thought of as a differential diagnosis if you see unidentified LVH.
References
Nakao S, Takenaka T, Maeda M, et al. An atypical variant of Fabry’s disease in men with left ventricular hypertrophy. N Engl J Med. 1995;333:288–93.
Richardson P, McKenna W, Bristow M, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation. 1996;93:841–2.
Schiffmann R, Kopp JP, Austin HA 3rd, et al. Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA. 2001;285:2743–9.
Nakatani S, Akaishi M, Asanuma T, et al. Guidelines from the Japanese society of echocardiography: guidance for the management and maintenance of echocardiography equipment. J Echocardiogr. 2015;13:1–5.
Masson C, Cissé I, Simon V, et al. Fabry disease: a review. Joint Bone Spine. 2004;71:381–3.
Kampmann C, Baehner F, Whybra C, et al. Cardiac manifestations of Anderson–Fabry disease in heterozygous females. J Am Coll Cardiol. 2002;40:1668–74.
Chimenti C, Pieroni M, Morgante E, et al. Prevalence of Fabry disease in female patients with late-onset hypertrophic cardiomyopathy. Circulation. 2004;110:1047–53.
Desnick RJ, Banikazemi M, Wasserstein M. Enzyme replacement therapy for Fabry disease, an inherited nephropathy. Clin Nephrol. 2002;57:1–8.
Shah JS, Hughes DA, Sachdev B, et al. Prevalence and clinical significance of cardiac arrhythmia in Anderson–Fabry disease. Am J Cardiol. 2005;96:842–6.
Mehta A, Ricci R, Widmer U, et al. Fabry disease defined: baseline clinical manifestations of 366 patients in the Fabry outcome survey. Eur J Invest. 2004;34:236–42.
Takenaka T, Teraguchi H, Yoshida A, et al. Terminal stage cardiac findings in patients with cardiac Fabry disease: an electrocardiographic, echocardiographic, and autopsy study. J Cardiol. 2008;51:50–9.
Namdar M, Steffel J, Vidovic M, et al. Electrocardiographic changes in early recognition of Fabry disease. Heart. 2011;97:485–90.
Hoigné P, Attenhofer Jost CH, Duru F, et al. Simple criteria for differentiation of Fabry disease from amyloid heart disease and other causes of left ventricular hypertrophy. Int J Cardiol. 2006;111:413–22.
Sachdev B, Takenaka T, Teraguchi H, et al. Prevalence of Anderson–Fabry disease in male patients with late onset hypertrophic cardiomyopathy. Circulation. 2002;105:1407–11.
Monserrat L, Gimeno-Blanes JR, Marín F, et al. Prevalence of Fabry disease in a cohort of 508 unrelated patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2007;50:2399–403.
Wu JC, Ho CY, Skali H, et al. Cardiovascular manifestations of Fabry disease: relationships between left ventricular hypertrophy, disease severity, and alpha-galactosidase A activity. Eur Heart J. 2010;31:1088–97.
Geske JB, Jouni H, Aubry MC, Gersh BJ. Fabry disease with resting outflow obstruction masquerading as hypertrophic cardiomyopathy. J Am Coll Cardiol. 2014;63:e43.
Pieroni M, Chimenti C, DeCobelli F, et al. Fabry’s disease cardiomyopathy: echocardiographic detection of endomyocardial glycosphingolipid compartmentalization. J Am Coll Cardiol. 2006;47:1663–71.
Kounas S, Demetrescu C, Pantazis AA, et al. The binary endocardial appearance is a poor discriminator of Anderson–Fabry disease from familial hypertrophic cardiomyopathy. J Am Coll Cardiol. 2008;51:2058–61.
Mundigler G, Gaggl M, Heinze G, et al. The endocardial binary appearance (‘binary sign’) is an unreliable marker for echocardiographic detection of Fabry disease in patients with left ventricular hypertrophy. Eur J Echocardiogr. 2011;12:744–9.
Pieroni M, Chimenti C, Ricci R, et al. Early detection of Fabry cardiomyopathy by tissue Doppler imaging. Circulation. 2003;107:1978–84.
Shanks M, Thompson RB, Paterson ID, et al. Systolic and diastolic function assessment in Fabry disease patients using speckle-tracking imaging and comparison with conventional echocardiographic measurements. J Am Soc Echocardiogr. 2013;26:1407–14.
Niemann M, Herrmann S, Hu K, et al. Differences in Fabry cardiomyopathy between female and male patients: consequences for diagnostic assessment. JACC Cardiovasc Imaging. 2011;4:592–601.
Boyd AC, Lo Q, Devine K, et al. Left atrial enlargement and reduced atrial compliance occurs early in Fabry cardiomyopathy. J am Soc Echocardiogr. 2013;26:1415–23.
Nagueh SF. Anderson–Fabry disease and other lysosomal storage disorders. Circulation. 2014;130:1081–90.
Nieman M, Breunig F, Beer M, et al. The right ventricle in Fabry disease: natural history and impact of enzyme replacement therapy. Heart. 2010;96:1915–9.
Kawano M, Takenaka T, Otsuji Y, et al. Significance of asymmetric basal posterior wall thinning in patients with cardiac Fabry’s disease. Am J Cardiol. 2007;99:261–3.
Eng CM, Guffon N, Wilcox WR, et al. Safety and efficacy of recombinant human alpha-galactosidase A—replacement therapy in Fabry’s disease. N Engl J Med. 2001;345(1):9–16.
Weidemann F, Niemann Breunig F, et al. Long-term effects of enzyme replacement therapy on Fabry cardiomyopathy: evidence for a better outcome with early treatment. Circulation. 2009;119:524–9.
Weidemann F, Breunig F, Beer M, et al. Improvement of cardiac function during enzyme replacement therapy in patients with Fabry disease: a prospective strain rate imaging study. Circulation. 2003;108:1299–301.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuasa, T., Takenaka, T., Higuchi, K. et al. Fabry disease. J Echocardiogr 15, 151–157 (2017). https://doi.org/10.1007/s12574-017-0340-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-017-0340-x