Abstract
The anatomy of the superior orbital fissure is very important because of the spaces it connects, the regions it is adjacent to, and the structures it contains. We aimed to study the width, length and types of the structure, their change according to gender, body sides, and age. The fissure shape has many variations that are not easy to systematize. Therefore, it was aimed to classify them with various reference points determined for the first time, identify their types and determine their incidence. An objective and comprehensive classification was used on 3-dimensional images using multidetector computed tomography. We retrospectively evaluated the orbit and paranasal sinus computerized tomography images of 200 individuals (age range: 3 months-90 years;106 female, 94 male). The shape of fissure were identified and classified, it is length and width were measured. There was no statistical difference in the length of the fissure according to gender on both sides, and in width only on the left (p˃0.05). On the right side, it was statistically significantly wider in female (p˂0.05). While the fissure types were grouped based on observation in the literature, they were defined more comprehensively according to different shape features by giving a certain reference lines by us for the first time and evaluated over seven types. The most common shape for both sides was racket-shaped type (right: 24.5%, left: 26%), while the least common was narrow type (right: 1%, left: 2%). Thus, the shape variations of structure have gained a systematic typing criterion for the first time with the definitions in our study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Superior orbital fissure (SOF) is a small but functionally very important structure through which important neurovascular structures related to sight pass (Natori and Rhoton, 1995). The oculomotor nerve, trochlear nerve, ophthalmic nerve, and abducens nerve enter orbit from here, while a branch of lacrimalis that goes to the superior ophthalmic vein and dura mater passes into the cranial cavity (Standring 2008). The SOF connects the orbit with the middle cranial fossa and continues with the anterior part of the cavernous sinus. Since the size and variations of this opening can affect the structures it contains, detailed information about its anatomical structure is critical for the correct diagnosis and local disorders treatment (Govsa et al. 1999). The SOF shape has many variations that are not easy to systematize. These differences may affect not only the clinical expression but also the approach to treatment after the injury (Gasco et al. 2009).
Located in the posterior half of the superolateral corner of the orbit, the SOF has a racket-like shape (Wolff et al. 1997). Its cone-shaped part on its superolateral extends to the os frontale, while the inferomedial part is large and resembles a comma (Pickard 2006). Shapiro and Janzen’s study (1960) is the first study to examine the SOF shape by dividing it into 6 types, Sharma et al. (1988) added three different types to this study, and then Govsa et al. (1999) used Sharma et al.’s (1988) classification in their study. In their study, Reymond et al. (2008) divided the structure into nine different types. However, they reported basically only 2 different types of this structure as follows: “type a” with a characteristic of narrowing and “type b” which lacks this narrowing and is significantly shorter than “type a.” According to these studies, SOF can be in the form of a racket or an egg (Sharma et al. 1988; Reymond et al 2008). A wide range of different intermediate shapes can be observed between these 2 different types (Regoli and Bertelli 2017). Therefore, unlike previous studies, reference points were determined, and the necessary definitions were made when typing in our study. With multidetector computed tomography (MDCT), which is an advanced system, a more objective and comprehensive classification was used on 3-dimensional images. In addition, its development according to age groups was also examined.
Materials and methods
Scans were performed with a 256-slice MDCT scanner (Siemens Somatom Flash, Erlangen, Germany). Imaging parameters were as follows: kV = 120; mA = 160; rotation time = 0.5 s; collimation = 64 × 0.625; FOV = 220 mm. Images that included the orbit and paranasal sinus were analyzed retrospectively on a workstation (Snygo Via, Siemens, Germany). According to the results of the power analysis using the GPower 3.1.9.4.program, the sample size was determined in 200 cases when the effect size was 0.75, the reliability was 0.95, and the power was 0.95. This single-center retrospective study was approved by the local institutional review board with a waiver of the requirement for written, informed consent.
The data of 355 patients who underwent orbital or paranasal CT imaging for different complaints between 2013 and 2021 were evaluated for the SOF analysis. In these images, a total of 155 cases, including orbital fractures (26 cases), pathology in orbital structures (21 cases), tumors (5 cases), patients who underwent orbital surgery (24 cases), foreign body in the relevant region (22 cases), and poor image quality (57 cases), were not included in the study. Images of a total of 200 individuals (400 sides), 94 male and 106 female, were used in the study. In these cases, prepubertal age was accepted as below 15 years old, postpubertal age was accepted as above 15 years old, and geriatric age limit was accepted as 60 years old (Alkofide 2007; Chauhan et al. 2014). Furthermore, they were examined according to the gender, the side of the orbit, and the anatomical structures development. Considering these limits, the cases were evaluated in eight different groups as 0–9 years old, 10–14 years old, 15–19 years old, 20–29 years old, 30–39 years old, 40–49 years old, 50–59 years old, and over 60 years old. Images of the same cases were transferred to the Syngo.via workstation, and three-dimensional images were obtained. It was ensured that the obtained images cover the entire area to be measured, and that the image quality was clear and understandable. For morphometric measurements, in the anterior view of the orbit, the position in which the frontozygomatic suture, supraorbital foramen (notch), anterior and posterior lacrimal crist of maxilla, infraorbital foramen, and vomer were on the same plane and clearly visible was determined (Fig. 1). The SOF length and width were measured in these images, and the variations were evaluated, defined according to their shapes, and were classified.
The position in which the SOF is evaluated. The supraorbital foramen (notch) on the supraorbital margin bone line (1), the anterior edge of the lacrimal fossa flor (2), the frontozygomatic suture (3), lateral margin of orbit (4), the infraorbital margin (5), the level of infraorbital foramen (6), the point of junction of the infraorbital margin and the medial magrin (7) and the medial margin bone line (8)
Length and width of the SOF
The longest distance between the corners of the structure was measured for the SOF length (Fig. 2a). On the other hand, the largest distance between the medial and lateral walls was measured for the SOF width (Fig. 2b). This process was repeated for both sides separately, and each parameter was measured three times and was then averaged.
Classification the SOF by shape
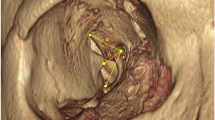
Unlike the previous studies, the SOF shape was classified into seven types by determining the reference points on three-dimensional images in our study. Descending perpendicularly to the line following its lateral edge from the optic canal, the SOF was divided into two parts, which are the upper opening and lower opening. The classification was made according to the relations of these two openings with each other. If the upper opening above this line was curved laterally, it was named as curved type (type 1) (Fig. 3). On the other hand, if the upper and lower openings lay on the same plane, it was named as straight type (type 2) (Fig. 4). In the racket-shaped type (type 3), a narrow and straight upper opening and a rather wide lower opening were detected (Fig. 5). The group in which the lower and upper openings were largeand symmetrical to each other was named as the eight-shaped type (type 4) (Fig. 6). The key-shaped type was named due to there dented appearance of the medial and lateral walls of the upper opening and the similarity in shape of the width of the lower opening together (type 5) (Fig. 7). The type with medial and lateral walls close to each other in both the upper and lower openings was also named as narrow type (type 6) (Fig. 8). The type in which no narrowing was observed between the two parts of the SOF, where the upper and lower openings could not be distinguished and the two openings were observed together as a triangle, was named as the triangular type (type 7) (Fig. 9). With these typings, the condition of the SOF type on both sides was evaluated. Furthermore, it was observed that the SOF shapes in the cases were the same type on both sides as well as different from each other.
Statistical analysis
The data conformity to the normal distribution was tested with the Shapiro Wilk test. Student’s t-test (for normally distributed variables) and Mann–Whitney u test (for non-normally distributed variables) were used in the comparison of numerical variables in two groups. The Kruskal Wallis test and Dunn’s multiple comparison test (for non-normally distributed variables) were used to compare numerical variables in more than two groups. The relationships between categorical variables were evaluated using the chi-square test. The SPSS for Windows version 24.0 program was used in the analysis, and the p-value less than 0.05 was considered statistically significant.
Results
In our study, data from 400 orbit of a total of 200 individuals, 94 male (47%) and 106 female (53%), were evaluated. Individuals aged between 3 months old and 90 years old were examined in eigth different age groups. An average of 23 individuals were included in each age group, and the distribution of age groups by gender was similar (p = 0.344). The SOF morphometric evaluation was performed, and its anatomical shapes were also investigated. The SOF types were classified with the reference lines and definitions determined by us by making formal examinations in the light of the existing literature. The reference values of these structures in healthy individuals were determined by making measurements on three-dimensional images. The morphological and morphometric findings were evaluated according to gender, side, and age. The incidence of anatomical SOF types was expressed as the percentages.
Length and width of the SOF
The SOF mean length was found to be greater in males than in females on the right side, but this difference was not statistically significant (p˃0.05). On the left side, mean measurements were found to be similar in both genders (p˃0.05). The SOF width was found to be greater in females than in males on both sides. While this difference was statistically significant on the right side (p˂0.05), it was not significant on the left side (p˃0.05) (Table 1). The SOF length was a minimum of 0.99 cm and 0.95 cm on the right side and left side, respectively, and a maximum of 2.2 cm and 2.16 cm on the right side and left side, respectively. The SOF width was a minimum of 0.33 cm and 0.18 cm on the right side and left side, respectively, and a maximum of 1.07 cm and 0.97 cm on the right side and left side, respectively.
The mean length and mean width of the SOF are given in Table 2 according to these age groups. When the length and width measurements were compared according to age groups, no statistically significant difference was observed between the sides (p˃0.05).
Classification the SOF by shape
The SOF shape was examined by considering the relative positions of its 2 openings, the features of its edges, and their relations with each other. While the SOF types were grouped without giving any lines or reference points based on observation in the literature, they were defined more comprehensively according to different shape features by giving a certain line and reference points by us for the first time and evaluated over seven types (Fig. 10).
While it was observed that the SOF shape was generally the same type according to the side where it was located (60.5%), it was found that some individuals had different types (39.5%). The difference of the sides in terms of shape was observed more in females (55.7%) than in males (44.3%). Among all the individuals, the most common shape for both sides was type 3 (right: 24.5% and left: 26%), while the least common was type 6 (right: 1% and left: 2%) (Fig. 11).
It was determined that the frequency of SOF shapes on both sides did not differ statistically in terms of gender (p˃0.05). The most common shape for both sides is type 4 in males and type 3 in females, while the least common type was type 6 in both genders and sides (Figs. 12 and 13).
Discussion
SOF is the easiest way for tumors to pass from the middle cranial fossa to the orbit (Moore et al. 2010). Surgery for the optic canal or SOF is performed behind the orbit in posttraumatic optic neuropathy injury, angioma, neuroma, malignant tumor, meningioma, tumors of lesser and greater wing of the sphenoid bone, and ophthalmic artery aneurysms with intracanal extension (Govsa et al. 1999).
Studies on the SOF in the available literature have generally been conducted with adults, and few studies have evaluated only the young population. In our study, both pediatric and adult individuals were examined. Prepubertal age was accepted as below 15 years old, postpubertal age was accepted as above 15 years old, and geriatric age limit was accepted as 60 years old (Alkofide 2007; Chauhan et al. 2014). Individuals of these 3 different periods were also examined in eight different age groups. It is thought that the evaluations made according to age in this morphometric study will contribute to the clinical evaluation and applications.
SOF is a small but functionally very important structure through which nerves providing afferent and efferent information about vision and vessels pass (Natori and Rhoton 1995). It is the largest opening connecting the orbit to the middle cranial fossa. Detailed knowledge of the anatomical structure of this region is critical for the correct diagnosis and local disorders treatment (Govsa et al. 1999). In the study of Natori and Rhoton (1995), the distance between the superomedial and superolateral corners of the SOF was measured in 15 cadavers and was reported as 1.59 cm. In the study of Reymond et al. (2008), 2 different shapes were reported as “type a” with a characteristic of narrowing and “type b” which lacks this narrowing and is significantly shorter than type a. It was stated that while the lengths of both types of structures were significantly different, there was no significant difference between their widths. In the study of Reymond et al. (2008), the mean SOF length was reported as1.747 cm in type a and 1.248 cm in type b (mean: 1.562 cm). In our study, the mean SOF length was found to be 1.6 ± 0.23 cm on the right side and 1.58 ± 0.22 cm on the left side. In the study of Reymond et al. (2008), the mean SOF width was found to be 0.731 cm in type a and 0.786 cm in type b. In our study, mean SOF width was found to be 0.63 ± 0.13 cm on the right side and 0.64 ± 0.13 cm on the left side.
The term SOF syndrome or Rochon–Duvigneaud syndrome generally covers lesions located just anterior to the orbital apex, including structures arising from the anulus of Zinn and structures outside the ring (Bailey et al. 2006). Among the nontraumatic causes of SOF syndrome, the SOF size is one of the risk factors, and the narrow opening andsoft tissue edema in the orbit can cause direct compression of the nerves (Fujiwara et al. 2009; Park and Kim 2017). The causes of SOF syndrome are classified as traumatic and nontraumatic. In traumatic injuries, the broken parts and hematoma directly compress the nerves, causing infection, edema, and blood circulation disruption around this structure (Fujiwara et al. 2009). Among the nontraumatic causes, the SOF size is one of the risk factors. Narrow SOF or soft tissue edema in the orbit can cause direct compression of the nerves. Therefore, surgeons should be careful with patients with a congenitally narrow superior orbital (Fujiwara et al. 2009; Park and Kim 2017). Located in the posterior half of the superolateral corner of the orbit, the SOF has a racket-like shape (Wolff et al. 1997). The shape of this structure has many variations that are not easy to standardize. These differences may affect not only the clinical expression but also the approach to be chosen in postinjury treatment (Gasco et al. 2009). Shapiro and Janzen (1960) is the first to examine the SOF shape by dividing it into six types. Sharma et al. (1988) added three different types to this study and then analyzed them in 9 types. In the study of Govsa et al. (1999), the Sharma et al.’s classification was used. Reymond et al. (2008) divided the SOF into nine different types, but they only reported two different forms of this structure, namely “type a” with a characteristic of narrowing and “type b” which lacks this narrowing and is significantly shorter than type a. According to these stuides, the SOF can be in the shape of a racket or an egg (Sharma et al. 1988; Reymond et al. 2008). A wide range of different types can be observed between these two different types, so subtypes are variable and very difficult to determine (Regoli and Bertelli 2017). For this reason, unlike previous studies, we determined reference points while typing in our study and used a more objective and comprehensive classification considering the types reported in the current literature. According to the reference lines we determined, we classified them as curved type (type 1), straight type (type 2), racket type (type 3), eight-shaped type (type 4), key-shaped type (type 5), narrow type (type 6), and triangular type (type 7). In their study, Sharma et al. (1988) and Govsa et al. (1999) reported types found without stating the classification criteria and definitions. However, in these studies, type 6 was the most common according to their own classification, and the incidence of this type was reported as 48.6% and 35.4%, respectively. The type 6 in these studies can be compared to the key-shaped SOF (type 5) in our study, and the incidence in our study was 12.5% on the right side and 11% on the left side. In their study, Reymond et al. (2008) reported that morphological types did not differ statistically in terms of gender and side. Generally, the structure shape was the same on both sides of the skull. In their study, Burdan et al. (2011) stated that the SOF shape is generally symmetrical; although, it has a wide morphological diversity. In our study, the incidence of shape differences according to the body side was found to be 39.5%. In addition, we thought that the existence of two types in the study of Reymond et al. (2008) is a decision about the evaluation method. As in the related study, there are different variations within the types with or without narrowings in many studies and in our study. These variations gained a systematic typing criterion with the definitions in our study.
Our study, evaluating the SOF length and width in terms of gender, side, and age is the most comprehensive study in the current literature. While the length of the fissure on both sides and the width only on the left side did not differ according to gender (p˃0.05), SOF was statistically significantly wider in females on the right side (p˂0.05) than in males. In addition, the SOF was statistically significantly longer on the right side than on the left side (p˂0.05).
Conclusions
The region anatomy of the SOF is very important because of the spaces it connects, the regions it is adjacent to, and the structures it contains. Due to the changing size and variations of this complex anatomy among individuals, it has been investigated by anatomists and clinicians for many years. Our study presented the reference ranges of the SOF morphometry in healthy individuals and evaluated them separately according to gender, body side, and developmental age. We thought that the measurements in our study will provide useful information for surgeons in the lesions treatment involving the lesser wing and greater wing of sphenoid, the posterior of the orbit, the SOF, and the optic canal. Although the fact that it has a narrow area and it contains neurovascular structures constitutes a limitation for surgical procedures, the change in its size during growth increases the importance of this region.
Data statement
All data supporting the findings of this study are available upon request.
References
Alkofide EA (2007) The shape and size of the sella turcica in skeletal class I, class II, and class III Saudi subjects. Eur J Orthod 29(5):457–463
Bailey BJ, Johnson JT, Newlands SD (2006) Head and neck surgery—otolaryngology. Lippincott Williams & Wilkins, Philadelphia
Chauhan P, Kalra S, Mongia SM, Ali S, Anurag A (2014) Morphometric analysis of sella turcica in North Indian population: a radiological study. Int J Res Med Sci 2(2):521–526
Fujiwara T, Matsuda K, Kubo T, Tomita K, Yano K, Hosokawa K (2009) Superior orbital fissure syndrome after repair of maxillary and naso-orbito-ethmoid fractures: a case study. J Plast Reconstr Aesthet Surg 62(12):e565–e569
Gasco J, Hooten K, Ridley RW, Rangel-Castilla L, Adewumi A, Nauta HJ, Resto VA (2009) Neuronavigation-guided endoscopic decompression of superior orbital fissure fracture: case report and literature review. Skull Base 19(3):241–246
Govsa F, Erturk M, Kayalioglu G, Pinar Y, Ozer M, Ozgur T (1999) Neuro-arterial relations in the region of the optic canal. Surg Radiol Anat 21(5):329–335
Moore KL, Dalley AF, Agur AMR (2010) Clinically oriented anatomy. Wolters Kluwer; Lippincott Williams and Wilkins, Philadelphia
Natori Y, Rhoton AL Jr (1995) Microsurgical anatomy of the superior orbital fissure. Neurosurgery 36(4):762–775
Park Y, Kim Y (2017) A statistical analysis of superior orbital fissure width in korean adults using computed tomography scans. Arc Craniofac Surg 18(2):89–91
Pickard JD (2006) Advances and technical standards in neurosurgery. Springer Wien, New York
Regoli M, Bertelli E (2017) The revised anatomy of the canals connecting the orbit with the cranial cavity. Orbit 36(2):110–117
Reymond J, Kwiatkowski J, Wysocki J (2008) Clinical anatomy of the superior orbital fissure and the orbital apex. J Craniomaxillofac Surg 36(6):346–353
Shapiro R, Janzen AH (1960) The normal skull: a Roentgen study. Hoeber, New York
Sharma P, Malhotra V, Tewari S (1988) Variations in the shape of the superior orbital fissure. Anat Anz 165(1):55–56
Standring S (2008) Gray’s anatomy: the anatomical basis of clinical practice. Elsevier Health Sciences, London
Wolff E, Bron A, Tripathi R, Tripathi B (1997) The bony orbit and paranasal sinuses Wolff’s anatomy of the eye and orbit. . Chapman and Hall Medical, London
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval (approval number 2020/01) was given by the Local Ethics Committee of the Medical Faculty. This single-center retrospective study was approved by the local institutional review board with a waiver of the requirement for written, informed consent. This study was conducted at Selcuk University Faculty of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pirinc, B., Fazliogullari, Z., Koplay, M. et al. Morphometric evaluation and classification of the superior orbital fissure on 3D MDCT images. Anat Sci Int 98, 196–203 (2023). https://doi.org/10.1007/s12565-022-00687-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12565-022-00687-2