Abstract
To determine the point of entrance of the thoracic duct in the venous system, as well as to evaluate some biometric measurements concerning its terminal portion, we conducted an anatomic study on 25 non-preserved cadavers. The termination of the thoracic duct occurred on the confluence between the left internal jugular vein and the left subclavian vein in 60 % of the individuals. The average results for the biometric measurements were: distance between the end of left internal jugular vein and omohyoid muscle 31.2 ± 2.7 mm; distance between the end of thoracic duct and the left internal jugular vein 0.0 ± 0.0 mm; distance between the end of thoracic duct and the left subclavian vein 3.6 ± 1.0 mm; distance between the end of thoracic duct and the left brachiocephalic vein 10.7 ± 3.1 mm. Moreover, it was identified that the left internal jugular vein length in level IV, measured between its entrance in the left subclavian vein and the omohyoid muscle, was able to predict the termination of the thoracic duct on the junction between the left internal jugular vein and the left subclavian vein (OR = 2.99) with high accuracy (79.3 %). In addition, the left internal jugular vein length at level IV was able to predict the localization of thoracic duct termination. Thus, this finding has practical value in minimizing the risk for a potential chyle leak during or after a left-sided neck dissection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical level IV corresponds to the lower jugular lymph nodes located around the lower third of the internal jugular vein. Its boundaries are the inferior border of the cricoid cartilage and the omohyoid muscle superiorly, the clavicle inferiorly, the posterior border of the sternocleidomastoid muscle posteriorly, and the lateral border of the sternohyoid muscle anteriorly. During a neck dissection involving this level on the left side, there is a risk of injury of the thoracic duct at its final segment, before entering the venous system. Albeit infrequent, being reported in 1–3 % of the cases, this complication may bring significant postoperative morbidity, with higher therapy-related costs and even higher risks for the patient’s health (Kaur et al. 2012; Skandalakis et al. 2007; Smoke and Delegge 2008).
An injury to the thoracic duct produces a chylous fistula, causing serious metabolic complications. It is associated with loss of tissue fluid, such as electrolyte imbalance, hypovolaemia, hypoproteinemia, periferic edema, lymphopenia, immunosuppression and coagulopathy. In addition, the lymph infiltration and its subsequent dissection of adjacent structures may affect the surgical wound, causing dehiscence and secondary infection of this site (Nowak et al. 2011). If the chyle accumulates in the pleural cavity, there may be also a significant impairment of the oxygenation resulting in cyanosis and dyspnea (Vaz and Fernandes 2006).
The chyle fistula is a severe neck dissection complication, and the best treatment is its prevention (Cernea et al. 2012). There are anatomic variations of the final segment of the thoracic duct, but, except for the knowledge of neck’s anatomy such as the sternocleidomastoid muscle and the clavicule, there are no helpful biometric measurements focusing on the point of entrance of the thoracic duct into the venous system available in the literature. Therefore, this anatomic study was designed to determine the point of entrance of the thoracic duct in the venous system, as well as to evaluate some biometric measurements on the left IV level, which could help the surgeon to predict the site of the thoracic duct’s termination.
Materials and methods
Ethics
The authors declare no conflict of interest and all the cadavers were treated with the highest respect. The research protocol was approved by Faculdade de Medicina da Universidade de São Paulo’s institutional review board (protocol number 312/13).
Anatomic study
A prospective non-randomized anatomic study was performed on 25 non-preserved cadavers who underwent necropsy at the Postmortem Inspection Service of the City of São Paulo. The sample comprised 64 % male and 56 % caucasian individuals, aged 71 ± 15.3 years old, with weight, high and BMI averages of of 57.3 ± 12.4 kg, 1.65 ± 0.1 m and 21.3 ± 4.9 kg/m2, respectively.
A wide cervico-thoracic incision was performed on each cadaver, from one pectoralis major muscle insertion to the other, 0.5–1 cm bellow the clavicles in order to prevent visible scars in their necks. Following the incision, the cutaneous flap was cranially dissected up to the hyoid bone, always as close as possible to the subcutaneous cellular tissue.
The left omohyoid muscle and the left internal jugular vein were then identified. Subsequently, the course of the left internal jugular vein (LIJV) until its confluence with the left subclavian vein (LSCV) was identified. Then, the brachiocephalic veins were also identified. Finally, the thoracic duct was searched and its localization was confirmed using the abdominal compression maneuver (Cernea et al. 2012). In this study, the thoracic duct was always found in the left side of the body.
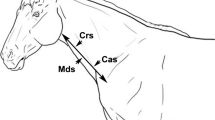
Using a pachymeter graduated in millimeters, the following biometric measurements were then obtained (Fig. 1): (#1) distance between the end of the thoracic duct and the intersection between the left internal jugular vein and the omohyoid muscle; (#2) distance between the end of the thoracic duct and the left internal jugular vein; (#3) distance between the end of the thoracic duct and the left subclavian vein; (#4) distance between the end of the thoracic duct and the middle third of the left brachiocephalic vein (the confluence of the left subclavian and left internal jugular veins); (#5) left internal jugular vein length in level IV, measured between its entrance in the left subclavian vein and the omohyoid muscle. The vascular measurements were performed on the lateral wall of internal jugular vein and in the superior wall of brachiocephalic and subclavian veins. These measurements were proposed to provide a practical guide for thoracic duct localization during a cervical operation and were always obtained by two investigators. If both agreed, the measurement was then registered. If there was any disagreement, the distance was double checked, corrected and then registered.
Biometric measurements: (#1) Distance between the end of the thoracic duct and the intersection between the left internal jugular vein and the omohyoid muscle; (#2) Distance between the end of the thoracic duct and the left internal jugular vein; (#3) Distance between the end of the thoracic duct and the left subclavian vein; (#4) Distance between the end of the thoracic duct and the middle third of the left brachiocephalic vein; (#5) Left internal jugular vein length in level IV, measured between its entrance in the left subclavian vein and the omohyoid muscle. Notes: In this illustration, the measurement of biometric parameters #2 and #3 are a point because when the termination of the thoracic duct occurred on the confluence between the left internal jugular vein and the left subclavian vein, these distances are equal to zero. The dotted lines in left brachiocephalic vein represent the division of this vein into three-thirds
Statistical analysis
The values of the qualitative variables were described using absolute and relative frequencies. Kolmogorov–Smirnov test was performed to determine the distribution of the quantitative variables, and the parametric ones were described using average and standard deviations for demographic data and using average and standard errors for biometric measurements in order to minimize discrepancies between a large range of values. Student’s t test and Mann–Whitney test were performed for the comparison between groups of, respectively, parametric and non-parametric quantitative data. Logistic regression was performed to determine risk stratification and odds ratio (OR), and confidence interval of 95 % (CI 95 %) were calculated. The receiver operating characteristic (ROC) curve was performed to validate the diagnosis tests and to determine the cutoff values. All these statistic analysis were done using the statistical software SPSS® version 17.0 (SPSS® Inc; Illinois, USA), and a significance level of 5 % was adopted (P ≤ 0.05).
Results
The termination of the thoracic duct occurred on the confluence between the left internal jugular vein and the left subclavian vein (Fig. 2) in 60 % (15 cases), directly on the left internal jugular vein in 36 % (nine cases), and on the left vertebral vein in 4 % (just one case). No anatomical variation, such as variations in numbers and courses of the thoracic duct, was found. Only a main route of the thoracic duct was observed in each specimen. The biometric measurements are described in Table 1.
There was only one case of termination of the thoracic duct on the left vertebral vein, and this case was excluded from further analysis; hence, the comparisons made in this study were only between the termination of the thoracic duct exactly on the confluence between the left internal jugular vein and the left subclavian vein versus directly on the left internal jugular vein (n = 24).
In this study, no statistically significant association was found between the termination of the thoracic duct and the following parameters: gender, age, body mass index, height and weight. Within the biometric measurements, the analysis showed a significant statistical association regarding only the distance between the intersection between the left internal jugular vein and the omohyoid muscle and the end of the thoracic duct on the confluence between the left internal jugular vein and the left subclavian vein, as well as with the left internal jugular vein length in level IV (Table 2).
Individuals with the terminal portion of the thoracic duct localized at the confluence between the left internal jugular vein and the left subclavian vein had higher measurements of left internal jugular vein length (measurement #5; p = 0.015—Student’s t test). Based on that, a logistic regression was performed, showing that for every 10 mm increment concerning the left internal jugular vein length, there was a chance of almost three times to find the termination of the thoracic duct on the left jugular-subclavian junction (OR = 2.99; CI 95 %: 1.1–8.2; p = 0.032). Similarly, in the present series, a cutoff value of 24 mm was established for this distance as a diagnostic test to predict the termination of the thoracic duct on the junction of the left internal jugular vein and left subclavian vein, with sensitivity of 100.0 % (CI 95 %: 78.2–100.0 %), specificity of 44.4 % (CI 95 %: 13.7–78.8 %), positive predictive value of 75.0 % (CI 95 %: 50.9–91.3 %), negative predictive value of 100.0 % (CI 95 %: 39.8–100.0 %) and area under the ROC curve of 79.3 % (CI 95 %: 58.4–93.1 %), as shown in Fig. 3.
Discussion
Although a thorough understanding of the anatomy of the thoracic duct is essential when performing neck dissection to prevent the complication chyle fistula, the “textbook” anatomy of the thoracic duct is found in only 50 % of individuals. In the other 50 % of cases, the thoracic duct anatomy may vary considerably (Hematti and Mehran 2011).
The real termination patterns of the thoracic duct vary greatly. According to different observers, the final drainage site of the terminal branches of the thoracic duct is the junction of the left subclavian and internal jugular veins in about 7.5–64.3 % of cases, the internal jugular vein in 4.8–85 % of cases, the external jugular vein in 7.1–28 % of cases, and the subclavian vein in 3.6–57.1 % of cases (Jdanov 1959; Kinnaert 1973; Langford et al. 1999; Shimada and Sato 1997; Skandalakis et al. 2007; Hematti and Mehran 2011). However, a recent systematic review with 12 studies and dissection of 532 ducts identified that the termination of thoracic duct occurs 46 % directly in internal jugular vein, 32 % in jugulo-venous angle, 18 % directly in subclavian vein and 4 % in other localizations (Phang et al. 2014). This anatomic study, performed in a Brazilian population, demonstrated that the most frequent termination of the thoracic duct was on the junction between the left internal jugular vein and the left subclavian vein, and no anatomical variations were found, probably due to the low number of specimens included.
The thoracic duct injury is a rare but serious complication that can occur during neck surgeries. The reported incidence of thoracic duct injury in such operations is 1–2.5 % of all cases, resulting in high mortality rates in untreated patients (Skandalakis et al. 2007; Smoke and Delegge 2008; Kaur et al. 2012).
Damage to the thoracic duct can be difficult to identify intra-operatively, as the rate of chyle flow is estimated to be only a couple of drops per second (Merrigan et al. 1997). Recently, a novel maneuver to allow detection of a chyle leak during neck dissection was described. Cernea et al. (2012) reported on a series of 206 patients, in which a manual abdominal compression maneuver allowed visualization of the thoracic duct leak at the end of neck dissection involving level IV. If a leak is identified during surgery, it should be immediately repaired. Despite the technological advances and new approaches described in the recent literature, there is no clear algorithm for anatomic identification of terminal portion of the thoracic duct in the neck (Campisi et al. 2013).
Therefore, the main objective of the present study was to present an important biometric measurement, the left internal jugular vein length, which can be easily obtained during a neck dissection including the left level IV, and has proved to be useful to predict the localization of thoracic duct termination. This is the most important anatomic parameter in the localization of the termination of the thoracic duct, offering additional information during a neck dissection, for example. There was a direct statistical relationship between increased length of the internal jugular vein and the termination of the thoracic duct exactly on the confluence between the left internal jugular vein and the left subclavian vein. In fact, there was an increased chance of nearly three times to find the termination of the thoracic duct on this location for every 10-mm increment. Thus, this finding has a practical value in order to minimize the risk for a potential chyle leak during or after a left-sided neck dissection. Moreover, an in vivo anatomical study must be conducted in order to validate these findings, especially because the marking points chosen as measurements were parts of soft tissues, and these could vary due to cadaveric rigidity.
References
Campisi CC, Boccardo F, Piazza C, Campisi C (2013) Evolution of chylous fistula management after neck dissection. Curr Opin Otolaryngol Head Neck Surg 21:150–156
Cernea CR, Hojaij FC, De Carlucci D Jr, Tavares MR, Araujo-Filho VJ, Silva-Filho GB, Brandao LG (2012) Abdominal compression: a new intraoperative maneuver to detect chyle fistulas during left neck dissections that include level IV. Head Neck 34:1570–1573
Hematti H, Mehran RJ (2011) Anatomy of the thoracic duct. Thorac Surg Clin 21:229–238
Jdanov DA (1959) Anatomy of the thoracic duct and of the main lymphatic vessels of the trunk in man. Acta Anat (Basel) 37:20–47
Kaur D, Jain M, Dhall U, Singh K (2012) An unusual course of the thoracic duct in relation to the vertebral vessels. Singapore Med J 53:e1–e2
Kinnaert P (1973) Anatomical variations of the cervical portion of the thoracic duct in man. J Anat 115:45–52
Langford RJ, Daudia AT, Malins TJ (1999) A morphological study of the thoracic duct at the jugulo-subclavian junction. J Craniomaxillofac Surg 27:100–104
Merrigan BA, Winter DC, O’Sullivan GC (1997) Chylothorax. Br J Surg 84:15–20
Nowak K, Wierzbicka M, Szyfter W (2011) Chylous leakage–rare but still dangerous complication after neck surgery. Otolaryngol Pol 65:128–131
Phang K, Bowman M, Phillips A, Windsor J (2014) Review of thoracic duct anatomical variations and clinical implications. Clin Anat 27:637–644
Shimada K, Sato I (1997) Morphological and histological analysis of the thoracic duct at the jugulo-subclavian junction in Japanese cadavers. Clin Anat 10:163–172
Skandalakis JE, Skandalakis LJ, Skandalakis PN (2007) Anatomy of the lymphatics. Surg Oncol Clin N Am 16:1–16
Smoke A, Delegge MH (2008) Chyle leaks: consensus on management? Nutr Clin Pract 23:529–532
Vaz MA, Fernandes PP (2006) Chylothorax. J Bras Pneumol 32(Suppl 4):S197–S203
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have read and approved the final manuscript and do not have actual, potential, or apparent conflict of interest with regard to the manuscript submitted for review, confirm that the manuscript has been submitted solely to Anatomical Science International and is not submitted, in press, or published elsewhere until the editorial board has decided whether to publish the article.
Rights and permissions
About this article
Cite this article
Louzada, A.C.S., Lim, S.J., Pallazzo, J.F. et al. Biometric measurements involving the terminal portion of the thoracic duct on left cervical level IV: an anatomic study. Anat Sci Int 91, 274–279 (2016). https://doi.org/10.1007/s12565-015-0295-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12565-015-0295-9