Abstract
The health care sector is highly data and information intensive. For clinicians, efficient management of information is a key resource. Patient-specific medication information is one of the essential parts of information used to support the clinical decision-making. This multi-method study at hand combines qualitative and quantitative data to investigate Finnish physicians’ perceptions of EPRs and their use, mainly focusing on the management of medication information. Based on the empirical material, the EPRs had an important role in clinical practice, and the physicians used them in managing patients’ medication information. However, the results also reveal that the clinicians were not considerably satisfied with the quality of the current EPRs. The findings of this study highlight the need for improving the quality of the systems and increasing the physicians’ satisfaction to materialize the benefits from the EPRs to avoid further disappointment and frustration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The global trend of health care organizations is to aim at producing health care services more efficiently. Many areas in the health care sector are highly information-rich and data-intensive in nature [16, 26]. Consequently, the collection, transmission, storage, and retrieval of information are essential in a majority of activities performed in the health care sector. Therefore, efficiently managed information is one of the most important resources in clinical practice [22]. Information technology (IT) is often seen as a part of the solution in achieving the goal of making the health care sector more competitive [7].
The availability of information is essential in many sectors, but in health care, the consequences of failing to provide professionals with accurate information can be more serious than just financial losses. According to an estimate, more than 1.5 million people are hurt every year by preventable medication errors in the U.S. [20]. Consequently, information related to medication is highly essential for health care professionals. The most important part of it is a patient’s current medication regimen; in addition to that, whether or not he/she takes them according to the physician’s orders. Medication information refers to a patient’s current medication regimen, including e.g. medication history, the generic and commercial name of the drug, the dosage, the use indication, and an individual’s medication-taking practices. This information also covers a patient’s risks information e.g. drug allergies [1].
Electronic patient records (EPRs) have an important role in managing patient-specific medication information. EPR refers to a system that “contains all or most of a patient’s clinical information from a particular hospital” ([18], p.295). The medication information presented in the EPRs is critical for securing safe and high-quality health care [39]. However, despite the undoubtedly essential role of the EPR, the literature describing its ability to support prescribing and other medication information-related activities is limited [12, 18].
The Finnish health care sector is characterized by universal public health services. Since the market is fairly small and language unique, it is not the most attractive market for service providers developing EPRs. However, there are several different EPRs in use in Finnish primary and secondary care. In terms of number of users, six systems dominate the Finnish EPR market. Recent studies conducted in Finland, but also internationally (cf. [8]) have revealed the weaknesses of the EPRs and also certain problems related to medication information. Despite the increased research interest, the current research focusing on EPRs in supporting the management of medication information from physicians’ perspectives has thus far remained scant.
To fill in the aforementioned gaps in the literature, we take a deeper look at the electronic management of medication information by exploring physicians’ perceived need for medication information, quality of medication information recorded in the EPR, availability of the medication information and finally the benefits achieved from the use of EPR from the physicians’ points of view. We take a multi-method approach by first analyzing a series of in-depth interviews and use the findings to develop a survey measuring the physicians’ perceptions of EPRs. Consequently, the research question is stated as follows: how do Finnish physicians perceive EPRs in the management of medication information?
The paper is organized as follows; after the introduction, a brief review of prior literature on EPRs is given. In chapter 3, the empirical research is reported. First, the analysis of the interview is presented. Based on the findings from the interviews, a research model and the research hypotheses are developed, followed by reporting the quantitative data collection and data analysis. In the final chapter, the main findings are presented, followed by the theoretical and practical implications. Finally, the limitations of the study and avenues for further research are discussed.
2 Related research
EPRs have been studied rather extensively. The research has often been concerned with EPR adoption among health care professionals [6] or effects of the systems on information quality [18]. There is a set of definitions for the often even interchangeably used terms EPR, electronic health record (EHR) and electronic medical records (EMR). According to the definition of Häyrinen et al. [18, p. 293], EHR is “a repository of patient data in digital form, stored and exchanged securely, and accessible by multiple authorized users”, whereas EPR refers to patient-specific clinical information from a certain health care organization.
The expected benefits from using information systems (IS) in health care can be related to e.g. improved quality of patient care, access to patient medical information and efficiency, financial savings and decreased number of medical errors, e.g. adverse drug events [31, 40]. Contrary to what is often promoted, the benefits of eHealth technologies related to both cost effectiveness and patient outcomes in fact still remain to be proven [4]. With regard to the assessment of specific information systems, a literature review conducted on EHRs revealed that the most often used criteria for health care IS quality were completeness and accuracy, and ease of use. Added to that, physicians’ use of EHRs was the most often studied topic. [18]
Both, primary and secondary care organizations use EPRs [18]. As an important stakeholder group, clinicians, and especially physicians, are in an essential role when assessing EPRs since the information achieved from the record is used to support their decision making. Or, at least it should be supporting it: studies conducted on the issue give diverse answers to that. In a Norwegian multi-method study conducted among general practitioners, physicians were commonly satisfied using the EPR. Despite the overall satisfaction, there were features that, from the physicians’ point of view, needed improvement. Functionality was one issue that was mentioned. Furthermore, the availability of the information within the EPR was not self-evident [8]. A recent study conducted in Finland is in line with this; it was found that the EPRs do not support physicians’ clinical work as expected. An alarming result of the study is that the poor functionality combined with poor usability can even lead to lowered patient safety [37]. Furthermore, another study uncovered that in some cases EPRs can be even a complicating factor when it comes to the physicians’ work [38]. These studies are in line with earlier ones in regard to patient safety; for instance, adverse drug events cannot be prevented even in computerized hospitals [25].
In large, the research on information technology adoption in the health care context has largely employed and adapted the Technology Acceptance Model (TAM) [9, 10]. Handy et al. [17] argue that the characteristics typical for health care context need to be taken into account and, therefore, added individual, organizational and system characteristics to the model since those were reported to have a strong influence on user acceptance. Menachemi et al. [21] have studied the adoption of EHR in the U.S. and argue that recent adopters are less likely to use all the system functionalities than early adopters. Therefore, the adoption rate as such does not tell the whole truth. According to them, the less enthusiastically adopted functionalities include those that have a major effect on processes and workflow, e.g. electronic prescribing. Although the respondents of this paper are from Finland, and basically mandated to “adopt” and use the different system functionalities, changes in workflow can be expected to affect also their attitudes to use EPR. Morton and Wiedenbeck [23, 24] found, in their two-part study conducted at an ambulatory care unit, that even, surprisingly, a physician’s characteristics, such as age, specialty, or the level of computer skills are not related to his/her attitude towards the EHR. They also found that EHRs should be flexible and ready for customization. Furthermore, they underline the importance of the co-operation between IT professionals developing the systems and caregivers, as there is not yet a very strong tradition for the system development.
3 Research design
3.1 Qualitative study
In order to increase knowledge of the Finnish physicians’ perceptions of EPRs in the management of medication information, a set of interviews was arranged. The interviews were conducted in a primary care organization consisting of one main health center and dispersed sub-units within one Finnish 174.000 habitants’ municipality. After a lengthy negotiation round, five physicians with varying work experience were selected for the interviews. The interviewed physicians worked mainly in the daytime and treated patients from a fixed geographical area on 15- to 20-minute, pre-booked visits.
The interviews consisted of semi-structured questions that also allowed new themes to be brought up. The core themes and the structure of interview themes were adopted based on a concept-centric review of prior research [36] examining electronic medical records (e.g. [5, 28, 35]) and substantiated with information obtained from research reports and professional magazines. Thereafter, the interview questions were reviewed by an expert panel consisting of medical professionals, hospital managers, healthcare IT specialist and e-health researchers to ensure that the interview themes are relevant and cover the most important aspects related to the clinicians’ use of EPRs.
Each of the interviews lasted from one to two hours; all the interviews were recorded and transcribed by one of the authors. QSR NVivo 8 software was used in the analysis. The interviews uncovered several interesting aspects of the electronic management of medication information, of which few appeared repeatedly. These aspects are developed next.
The interviews revealed, among other things, that medication information is highly important in clinical work. That was proven, as all the interviewees mentioned needing the information very often and with almost every patient. One of the physicians summed up the comments of the physicians concerning the need of information: “I want to know the patient’s medication information as extensively as possible; well, there is not much about the medication information I wouldn’t like to know.” Another one described the meaning of the information as follows:”The [information that is needed] is what the patient really puts down his/her throat, the real medication in practice. This is because the EPR is full of different kinds of patient-specific medication lists that you can’t rely on.” This comment leads us to the core problem: There is a great need for medication information, and a lot of information is available electronically, but it is not reliable. When a patient first arrives at a health care facility, there might be information about his/her medications, but it is not up-to-date. In cases where the patient is then referred to secondary care, he/she goes there with incomplete information. One of the interviewed told how she proceeded in these situations:”…I’ve examined the patient and found out that there’s no information available as to their medication, and I sometimes write on the referral that ‘we don’t know anything about the medication, but here comes the patient’. Or, I write that possibly the following medication is being used, based on the list from EPR, but I can’t be sure.”
However, the EPR itself is not the only source of uncertainty, but there are, of course, also human factors involved. These problems are related both to the motivation of the health care professionals to update medication information and to the characteristics of the information system. The interviewed physicians explained that the EPR does not make it easy to keep the patient-specific medication information updated: “…it’s hard work when you do it and a bother to update it [the list of medication on the computer], and it’s something that does not necessarily motivate you.” When it comes to the comments on hard work and lowered motivation of the physicians, they said that one of the reasons for not updating the information on each patient visit is that all the medications are on the same list, no matter whether the patients is on them or not. For instance, removing unnecessary medications from the list requires a lot more than just deleting them from the list: each medication row needs to be opened for that and handled one by one. Some of the experienced physicians said that they preferred to include a list of patients’ current medications to the free-text summary section. There are also situations where updating the patient-specific medication information does not fit the work flow:”…at least I don’t trust that it [medication information] is noted in there [patient information system] with sufficient accuracy. My personal experience is that all the medication information is not necessarily recorded on the computer, at least when renewing prescriptions.” This is often the case when the prescription is paper-based and has been originally prescribed by someone else than the renewing physician. However, there will be a solution to this problem as the national electronic prescription system is fully in operation. Furthermore, only entering the medication module leaves a sign that gives an impression of an updated list of medications. These are naturally, at some level, problems related to the organization (e.g. motivation of the physicians) and system. However, all these issues are closely connected with the requirement level physicians have for the information systems they use.
The need for information is especially emphasized in critical situations as medication has an effect on many treatment decisions. Consequently, there should be easy access to the information: “Yeah, on-call. They may bring an unconscious, old, sick patient…and we start thinking, has he/she been treated somewhere, does he/she have any illnesses, and what medication has he/she taken and what’s the dosage, it’s essential—this is the most difficult situation, you are extremely busy and you can’t reach anyone on Saturday night.” However, availability of information is essential in every situation where there is only a limited time for each patient, but in critical situations, even a patient’s life could be threatened in an extreme situation. One of the interviewees described how she would like to acquire the information:”The faster, the better, of course but we’ve got 15 min per patient, and there [on-call] even less.” In other words, there should not be any obstacles hindering the access to information. In light of the comment presented next, 15 min for a patient visit would not be enough for extensive information searching: “Medication information on the drugs taken daily can be very challenging… it can take 10 min to find out what the patient is really taking.”
Most of the physicians’ comments were related either to the desired characteristics of medication information or were complaints about the functionality of the EPR. Often these characteristics were expressed in negative relation since there were many difficulties in regard to the current quality of medication information. The desired characteristics were described for instance in the following comment:”…that you don’t get the information from anywhere, reliable information. If there was a medication list [in the EPR] that would be updated according to a basic rule you would know that it is complete for sure, there would not be any problems…” Another physician was suspicious about the information recorded in the EPRs: “…at least I don’t trust that it [medication information] is recorded there accurately enough”. According to the physician, for instance, changes in the dosage were not always entered into the EPR properly since the instructions were often given verbally. Therefore, the interviewees were often suspicious to the relevancy of the information acquired from the EPR and did not always find it relevant enough to support treatment decisions. Added to that, one of the physicians commented: “of the amount of the information that is currently recorded, I would say that 90 % is irrelevant, and from a patient’s [treatment’s] point of view at least 80 % is useless. The essential information should be winnowed out, it should jump out.” Summing up the above-presented findings, the medication information desired should be reliable, up-to-date, complete, and relevant.
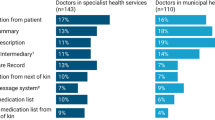
Since the quality of the information achieved electronically is not always as expected, health care professionals need to find other ways to define a patient’s medication information. Something about the reliability of the electronic information tells us that most of the physicians mentioned the patient as an extremely essential source of medication information. That is understandable, as the patient or his/her family member are the only ones who can tell about, for instance, the medication-taking habits of the patient. As to the list of medications, the information provided by the patient serves the health care professional and is often even a highly necessary part of the information-seeking process. Unbelievably, still these days, when electronic patient records are available, a list of medications on a piece of paper written by the patient is essential as can be seen from the following citation: “It [the possible medication list in the EPR] is looked through always, like:‘Ah! This kind of medication is available; does it correlate with the medication list on the piece of paper provided by the patient at all? No, it doesn’t.’” In other words, when prescribing medications for a patient, instead of taking a glance at the computer and getting the medication information, the care giver goes through a series of comparisons and checking before defining the patients list of medication.
In regard to the perceived benefits, the interviewed physicians were not extremely satisfied with EPRs, however, they still found positive aspects of the use. For instance, patient safety was commented as follows by one of the interviewees: “Well, it has probably enhanced.” Another one also found positive sides of the EPR:”I must admit that there are some benefits from the ADP (automatic data processing) issues. We have a system that is, however, full of failures,…, but it has been advantageous for real a couple of times when I’ve prescribed a medicine,…,and I have forgotten that the patient is taken this [drug],…, I have avoided many mistakes when the computer has alerted me [of possible adverse effects].” Despite the less enthusiastic opinions, the interviewed would probably not be ready to go back to the time before electronic patient records; thus, it can be expected that there must be at least some benefits of using it.
To summarize the findings of the interviews, four core themes emerged repetitively. First of all, when discussing the key attributes of quality of EPRs, the respondents underscored that the information offered by the system must be reliable and available at all times. The need for this information was also clearly addressed, potentially also because of the dissatisfaction with the current EPRs and their functionality. Moreover, the value of high-quality medication information in the clinical work was addressed in a number of instances.
3.2 Research hypotheses
In the following, we develop the research hypotheses. Rather than testing a priori theory, we have taken an exploratory approach and ground the research hypotheses on the findings from the interviews.
Based on the analysis of the data obtained from interviewing the physicians, we substantiated the qualitative analysis with a quantitative study. We used four emergent themes from the interviews to build the constructs for the quantitative part of the study. The first to constructs were related to the effective use of the EPR, namely the availability of information and information quality. The third construct was the need for obtaining medication information, i.e. the task the EPRs are designed to fulfill.The fourth construct perceived benefits, encompasses the value of the EPR in managing patients’ medication information. Thus, rather than testing a strong a priori theory in a strict confirmatory setting, the purpose of the quantitative study is to explore the relationships between constructs extracted from the qualitative analysis to develop a testable research model. To substantiate the development of the research hypotheses with grounding on prior research, we have used the literature on the adoption and use of IT to guide the research model.
Altogether, we have constructed the research model in a way that EPRs are viewed as task-oriented systems designed to fulfill a core set of needs and hence increase work performance. Consequently, the perceived quality of the IT artifact is viewed to have a positive effect on the physicians’ work performance. This line of reasoning has been extensively used in prior technology adoption research. (see e.g. [9, 14, 32–34])
Given the exploratory nature of the present study and the limited literature focusing specifically on the core properties and value of EPRs for user’s perspective, the research hypotheses are drawn based on the findings from the qualitative analysis of the interviews as well as prior IT adoption literature from other contextual settings.
Benbasat and Zmud [3] have addressed the importance of usage context in understanding the usage decisions. Hence, we used the data from the interviews to operationalize the four key research constructs. The need for medication information from the EPR was operationalized to consist of information about the usage of over the counter drugs, patient’s medication history, information about the current medication and potential risk factors such as allergies. Increased patient safety, increased work efficiency, and enhanced quality of the clinical work were used as the variables measuring the perceived benefits of the EPR.
Altogether, the respondents addressed their dissatisfaction with various aspects of the EPRs they are currently using. Given their critical approach toward the EPRs, it is plausible to interpret that when the medication information is needed extensively, the users are more critical towards the system. Hence, the following hypothesis is postulated:
-
H1:
Need for medication information negatively affects the perceived benefits of the EPR.
Based on the information obtained from the interviews, the information quality and availability of the medication information, as well as availability, were used to capture the perceived quality of the EPR. Prior IS research has demonstrated information quality as being an important contributor to system utilization and hence, organizational impact [11]. As a result, we put forward the following hypotheses:
-
H2:
Information quality of the medication information obtained from the EPR positively affects the perceived benefits of the EPR.
-
H3:
Availability of the medication information positively affects the perceived benefits of the EPR.
The physicians addressed the importance and need for medication information in their work but at the same time mentioned several problems associated with the EPRs. Thus, the more the physicians need information from the EPR, the more prevalent the problems and shortcomings more are. In consequence, the relationship between need and information quality of the EPR is likely to be negative.
-
H4:
The need for medication information negatively affects the perceived reliability of the information obtained from the EPR.
We assert that the extensive use of the EPR to obtain medication information makes the physicians savvier with the features and functionalities of the EPR, suggesting a positive relationship between the needs and availability of the information. Thus, we propose the following:
-
H5:
The need for medication information positively affects the perceived availability of the medication information.
Based on the information obtained from interviewing the physicians, accessing the information quickly and easily were found as key aspects of availability of the medication information in the EPR. Also, prior literature offers evidence that systems that are considered easy to use are also perceived as more useful [10]. As a result, the final hypothesis is postulated:
-
H6:
Availability of the medication information positively affects information quality.
3.3 Data collection for the quantitative study
The empirical data to test the research model was collected with an online survey that was administered to 500 physicians belonging to the Finnish medical society Duodecim. The invitation to participate in the research was first emailed to two professionally well-known physicians representing the medical society who then forwarded the invitation to their professional networks. The researchers and representatives of the medical society jointly designed a questionnaire that went through many assessment rounds. The survey consisted of 19 multiple choice and short answer questions. Those were mostly 5-point Likert-scale questions anchoring from “Do not agree at all” to “Agree completely” and from “With every patient” to “Never”. The participation was voluntary, and the answers were anonymous, containing background information on their age, gender, professional experience and specialty.
The final sample consisted of 131 Finnish physicians of which 68 were male and 63 female. The respondents were relatively experienced; the median value for the professional experience was 20 years (see Table 1 presenting the characteristics of the respondents).
As can be seen from Table 2, presenting the means, standard deviations and factor loadings for the observed variables, the respondents were not particularly satisfied with their EPRs. This is also in line with the interview results, though the interview material consists only of primary care physicians, whereas the survey respondents represented both primary and secondary care physicians.
3.4 Analysis of the quantitative data
The data was analyzed using partial least squares (PLS) with SmartPLS M3 software [27]. The PLS method is typically recommended in situations in which there are no stable, well-defined theories to be tested in a confirmatory research setting and when the sample size is small [15]. In addition, Barclay et al. [2] suggest that PLS is viable for analyzing predictive research models that are in the early stages of theory development, as is the model in the present study.
The convergent validity was evaluated based on three criteria: 1) all indicator loadings of the four factors representing the research constructs should be significant and exceed 0.7, 2) composite reliabilities should exceed 0.80, and 3) average variance extracted (AVE) by each construct should be greater than the variance due to measurement error (AVE > 0.50) [13]. As can be seen from Table 2, altogether 3 items had factor loadings below 0.7, and they were dropped from the measurement. Other factor loadings exceeded 0.7 and were significant at the .01 level. After dropping the three items (INFOQUAL2, NEED2 & NEED3), all measures met the criteria for convergent validity.
Discriminant validity was investigated by examining whether the square root of AVE for each construct was higher than the squared correlation between it and all other constructs [13]. This test was met and hence the four factors were found to be empirically distinct from one another. The statistics for convergent and discriminant validity are presented in Table 3.
Of the hypothesized relationships, only three were statistically significant (t > 1.98). As a result, hypotheses 1, 4 and 5 are not supported. Figure 2 represents the results from the path analysis, and Table 3 summarizes the results of the hypothesis.
4 Discussion
4.1 Research implications
From an IS adoption perspective, the current situation with EPRs in Finland reflects a post-adoption scenario [19] where the system has been adopted in the organization and is actively used. Interestingly, however, at the same time, the problems with the system are widely acknowledged. Thus, instead of promoting the system and persuading the user to adopt it, the current challenge lies within developing the system to be utilized more effectively in order to fully materialize the benefits from the system usage [11]. In this regard, the present study underscores the importance of viewing IS adoption as an ongoing and adaptive process towards better utilization of the systems.
The results revealed a negative, albeit not statistically significant, relationship between the need for medication information and the perceived benefits of the EPR, confirming the findings from the interviews. The findings of the study are in line with prior research addressing the challenges with EPRs [8]. This reflects that EPRs have not reached a sufficient level of functionality to meet the expectations of the users, and that more emphasis needs to be put on managing the users’ needs and expectations to avoid further dissatisfaction.
From a theoretical standpoint, an interesting notion is the actual source of the dissatisfaction with current EPRs alongside the issues with reported functionality issues. The adoption of EPRs has caused changes to the work practices, but according to a literature review by Uslu & Stausberg [30], 11 studies out of 20 confirm that the time needed for administrative work has reduced. One could say that the number of confirmatory studies is not very high when many of the organizations implementing such a system expect it to bring financial savings. However, costs related to documentation, including for instance data acquisition, were reduced. Therefore, it might be reasonable to argue that the challenges related to poor functionality of EPRs manifest themselves for individual users, but on an organizational level, these issues are less visible. Furthermore, also in this study, the physicians identified situations where the EPR had a positive effect on their work. In any event, for highly educated and relatively well-paid professionals such as physicians, the poor functionality of the EPR may cause frustration and feelings of misuse of resources. In other words, despite the fact that Finland has a relatively high coverage of EPRs when compared internationally, only having a system implemented does not guarantee satisfaction for all the stakeholders.
4.2 Practical implications
The most important factor influencing several aspects of EPR use is the limited time. If there was unlimited time for searching and use of information, health care professionals would not face many of the current difficulties. However, since one of the drivers for using IT in health care settings is to produce gains in efficiency, the time required to manage patient-specific medication information should be decreased. If this goal does not materialize, and furthermore, if even the quality of the information is questionable, what is the point of using IT applications that neither support the clinical work nor produce gains in efficiency?
The results reveal that the patients’ medication history is not needed as extensively as the other aspects of medication information investigated here. Given that the physicians expect the most important information to be available quickly, this suggests that the medication history does not include the most important information appearing on the main screen of the patient’s record.
The analysis of the quantitative data demonstrated that the need for obtaining high-quality medication information, and at the same time, that the current EPRs do not meet the physicians’ needs. Because physicians understand the importance of the medication information, and because their organization mandates them to do so, EPRs are used. Moreover, acquiring information from other sources is difficult since, in practice, paper-based records do not exist anymore. The analysis of the qualitative data, however, revealed that in addition to the EPR, the patient acts as a source of medication information.
As stated earlier, some of the quality problems of medication information in the EPR are dependent on the physicians own activity and motivation. In regard to the motivation, for instance, updating of the medication list was found to be difficult and, therefore, not motivating. Most likely, the motivation of the physicians would be higher if the system would support their tasks in a positive way. Furthermore, a health care professional should not need to compare the information achieved from different sources but to get the accurate information. As this is not the case, perhaps close the co-operation claimed for instance by Morton & Wiedenbeck [23] between physicians and IS developers has failed. However, that would also require interest on the physicians’ part.
In the Finnish case, the clinicians are basically mandated to use the EPR; whereas, for instance, in the U.S. many private practitioners have chosen not to use their information systems and their key functions even if they have purchased one. [29] One can also ask, what is the effect of mandated use to the co-operation with developers? Would there be more interest in that if the physicians were independent entrepreneurs and responsible themselves for the purchasing of the EPR and other IS? And, most importantly, what would be the level of use if only those Finnish physicians considering EPRs satisfying used them?
4.3 Limitations & further research
There are a number of limitations in this research. The sample size for the quantitative analysis was small and the respondents not randomly selected. Therefore, the results of the study cannot be generalized in a statistical sense to represent all Finnish physicians. The Finnish, as well as the Nordic, health care system is characterized by public universal access and physicians being employees of the health care organizations to the service, contrary to e.g. the USA where the supply of the health care services is more complex and the physicians’ work on an entrepreneurial basis within the organizations. As a result, the context should be taken into account when considering the theoretical generalizability of the findings.
As regards the avenues for further research, the current study focused on investigating the physicians’ perceptions regarding EPRs in managing the medication information. Given that perceptions are ultimately subjective evaluations, further research investigating the “objective” performance of the EPR e.g. the length of downtimes, response times would be highly appropriate. In addition, future research could explicitly examine the gap between selected measures of system performance and the users’ evaluations of these measures. Third, critical incident technique could be employed to identify the encounters having the greatest significance in forming users’ perceptions of the performance of EPRs.
References
Aarnio E, Raitoharju R. The use of data sources of medication information - a Finnish primary care organization in the light of national e-Health scenarios. In: Oya M, Uda R, Yasunobu C, editors. IFIP international federation for information processing. Towards sustainable society on ubiquitous networks, vol. 286. Boston: Springer; 2008.
Barclay D, Higgins C, Thompson R. The Partial least squares approach to causal modeling, personal computer adoption and use as an illustration. Technol Stud. 1995;2:285–309.
Benbasat I, Zmud RW. The identity crisis within the is discipline: defining and communicating the discipline’s core properties. MISQ. 2003;27(2):183–94.
Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, et al. The impact of ehealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8(1):e1000387.
Berg M, Langenberg C, Berg I, Kwakkernaat J. Considerations for sociotechnical design: experiences with an electronic patient record in a clinical context. Int J Med Informat. 1998;52(1–3):243–51.
Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10(1):231–46.
Chiasson M, Reddy MC, Kaplan B, Davidson E. Expanding multi-disciplinary approaches to healthcare information technologies: What does information systems offer medical informatics? Int J Med Informat. 2007;76(S1):S89–97.
Christensen T, Grimsmo A. Instant availability of patient records, but diminished availability of patient information: a multi-method study of GP’s use of electronic patient records. BMC Med Informat Decis Making. 2008;8(1):12–20.
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MISQ. 1989;13(3):319–40.
Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: a comparison of two theoretical models. Manag Sci. 1989;35(8):982–1003.
DeLone WH, McLean ER. The DeLone & McLean model of IS succees: A ten-year update. J Manag Inform Syst. 2003;19(4):9–30.
Delpierre C, Cuzin L, Fillaux J, Alvarez M, Massip P, Lang T. A systematic review of computer-based patient record systems and quality of care: more randomized clinical trials or a broader approach? Int J Qual Health Care. 2004;16(5):407–16.
Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Market Res. 1981;18(1):39–50.
Goodhue DL, Thompson RL. Task-technology fit and individual performance. MIS Q. 1995;19(2):213–36.
Haenlein M, Kaplan A. A beginner's guide to partial least squares analysis, Understanding Statistics – Statistical Issues in Psychology, Education and the Social Sciences. 2004;3(4):283–297.
Hagland M. Intensive care: the next level for IT. Health Manag Technol. 1998;19(13):18–21.
Handy J, Hunter I, Whiddett R. User acceptance of inter-organizational electronic medical records. Health Informat J. 2001;7(2):103–7.
Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. (Int J Med Informat. 2008;77(5):291–304.
Jasperson J, Carter PE, Zmud RW. A comprehensive conceptualization of post-adoptive behaviors associated with information technology enabled work systems. MIS Q. 2005;29(3):525–57.
Laundro L. Incentives Push More Doctors to E-Prescribe. The Wall Street Journal. January 21, 2009. 2009. http://online.wsj.com/article/SB123249533946000191.html
Menachemi N, Ford EW, Beitsch LM, Brooks RG. Incomplete EHR adoption: late uptake of patient safety and cost control functions. Am J Med Qual. 2007;22(5):319–26.
Moen A. A nursing perspective to design and implementation of electronic patient record systems. J Biomed Informat. 2003;36(4/5):375–8.
Morton ME, Wiedenbeck S. A framework for predicting EHR adoption attitudes: a physician survey. Perspect Health Inform Manag. 2009;6(Fall):1a.
Morton ME, Wiedenbeck S. EHR acceptance factors in ambulatory care: a survey of physician perceptions. Perspect Health Inform Manag. 2010;7:1c (Winter 2010).
Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High rates of adverse drug events in a highly computerized hospital. Arch Intern Med. 2005;165:1111–6.
Reddy MC, Spence PR. Collaborative information seeking: a field study of a multidisciplinary patient care team. Inf Process Manag. 2008;44(1):242–55.
Ringle CM, Wende S, Will A (2005) Smart PLS 2.0M3. from www.smartpls.de.
Simon SR, Kaushal R, Cleary PD, Jenter CA, Volk LA, Orav EJ, et al. Physicians and electronic health records - a statewide survey. Arch Intern Med. 2007;167(5):507–12.
Simon SR, Soran CS, Kaushal R, Jenter CA, Volk LA, Burdick E, et al. Physicians’ use of key functions in electronic health records from 2005 to 2007: a statewide survey. J Am Med Informat Assoc. 2009;16(4):465–70.
Uslu AM, Stausberg J. Value of the electronic patient record: an analysis of the literature. J Biomed Informat. 2008;41(4):675–82.
Wang SJ, Prosser LA, Bardon CG, Spurr CD, Carchidi PJ, Kittlera AF, et al. A cost-benefit analysis of electronic medical records in primary care. Am J Med. 2003;114(5):397–403.
Venkatesh V. Determinants of perceived ease of use: integrating control, intrinsic motivation, and emotion into the technology acceptance model. Inform Syst Res. 2000;11(4):342–65.
Venkatesh V, Bala H. Technology acceptance model 3 and a research agenda on interventions. Decis Sci. 2008;39(2):273–315.
Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–78.
Ventres W, Kooienga S, Vuckovic N, Marlin R, Nygren P, Stewart V. Physicians, patients, and the electronic health record: an ethnographic analysis. Ann Fam Med. 2006;4(2):124–31.
Webster J, Watson RT. Analyzing the past to prepare for the future: writing a literature review. MIS Q. 2002;26(2):8–22.
Winblad I, Hyppönen H, Vänskä J, Reponen J, Viitanen J, Elovainio M, et al. Potilastietojärjestelmät tuotemerkeittäin arvioitu. Finnish Medical Journal, 2010;65(50–52):4185–94.
Vänskä J, Viitanen J, Hyppönen H, Elovainio M, Winblad I, Reponen J, et al. Lääkärien arviot potilastietojärjestelmistä kriittisiä. Finn Med J. 2010;65(50–52):4177–83.
Xu H, Stenner SP, Doan S, Johnson KB, Waitman LR, Denny JC. MedEx: a medication information extraction system for clinical narratives. J Am Med Informat Assoc. 2010;17(1):19–24.
Yamamoto LG, Khan ANGA. Challenges of electronic medical record implementation in the emergency department. Pediatr Emerg Care. 2006;22(3):184–91.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heiro, E., Mäntymäki, M. Managing medication information with electronic patient records – a Finnish clinicians’ perspective. Health Technol. 2, 113–122 (2012). https://doi.org/10.1007/s12553-012-0025-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-012-0025-4