Abstract
Background
Men with advanced prostate cancer (APC) face multiple challenges including poor prognosis, poor health-related quality of life (HRQOL), and elevated symptom burden. This study sought to establish the efficacy of a tablet-delivered, group-based psychosocial intervention for improving HRQOL and reducing symptom burden in men with APC. We hypothesized that men randomized to cognitive-behavioral stress management (CBSM) would report improved HRQOL and reduced symptom burden relative to men randomized to an active control health promotion (HP) condition. Condition effects on intervention targets and moderators of these effects were explored.
Methods
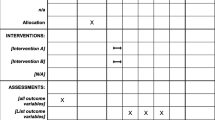
Men with APC (N = 192) were randomized (1:1) to 10-week tablet-delivered CBSM or HP, and followed for 1 year. Multilevel modeling was used to evaluate condition effects over time.
Results
Changes in HRQOL and symptom burden did not differ between groups. Men in both groups improved across several intervention targets; men in the CBSM condition reported greater increases in self-reported ability to relax, and both conditions showed improvements in cancer-related anxiety, cancer-related distress, and feelings of cohesiveness with other patients over time. Moderating factors included baseline interpersonal disruption, fatigue, and sexual functioning.
Conclusions
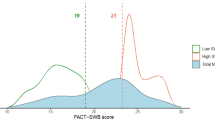
Tablet-delivered CBSM and HP were well received by men with APC. The hypothesized effects of CBSM on HRQOL and symptom burden were not supported, though improvements in intervention targets were observed across conditions. Participants reported high-baseline HRQOL relative to cancer and general population norms, possibly limiting intervention effects. The identified moderating factors should be considered in the development and implementation of interventions targeting HRQOL and symptom burden.
Trial Registration
ClinicalTrials.gov Identifier: NCT03149185
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most commonly diagnosed cancer among men in the United States (US) [1]. Unlike men diagnosed with early-stage prostate cancer who have a nearly 100% 5-year survival rate, men diagnosed with advanced prostate cancer (APC) have an approximately 30% 5-year survival rate [1]. In addition to facing a poor prognosis, men with APC face many disease- and treatment-related symptoms (e.g., sexual dysfunction, impotence, anemia, fatigue, pain, incontinence, hot flashes) and poor health-related quality of life (HRQOL), as well as psychosocial concerns (e.g., mood changes, cancer-related distress) [2,3,4,5]. These challenges may be exacerbated by concerns related to the cancer itself, such as the need for ongoing monitoring of disease progression and worse odds for survival, as well as treatment effects. Androgen deprivation therapy (ADT) is the standard of care for APC [6]. Although this approach is effective for delaying cancer progression, ADT results in numerous adverse physical and psychosocial side effects and has been shown to exacerbate worsened HRQOL [7].
There is considerable evidence to support the salutary effects of psychosocial interventions on improving the symptom burden and HRQOL of patients with cancer [8, 9]. For example, psychosocial interventions such as cognitive-behavioral stress management (CBSM) have been associated with improved emotional well-being, HRQOL, and sexual functioning outcomes in men with localized prostate cancer [10, 11]. However, despite the many symptoms and challenges faced by men with APC, most psychosocial interventions in prostate cancer have been limited to men with localized disease [12]. Given the heightened psychosocial burden of APC relative to localized disease, there is an urgent need for identification of effective strategies to improve symptom burden and promote well-being in this population. However, standard delivery of extant interventions may not meet the unique needs of this population. For example, requiring in-person participation may not be feasible for men with APC given increased functional impairment and disease burden.
The present study investigated a web-based intervention that consisted of a 10-week CBSM condition adapted to be particularly relevant for men with APC as opposed to localized disease, compared with a 10-week health promotion (HP) condition, among a racially diverse group of men with APC receiving androgen deprivation therapy (ADT). The web-based administration permitted participation from home, without requiring in-person attendance. The primary aim of this randomized controlled trial was to establish the efficacy of CBSM for improving HRQOL and reducing symptom burden outcomes relative to HP. It was hypothesized that participants randomized to the CBSM condition would have statistically improved scores on measures of HRQOL and symptom burden relative to participants randomized to the HP condition. It was also hypothesized that intervention targets (i.e., stress management, anxiety, positive affect, interpersonal disruption, stress) would be significantly improved for participants in the CBSM condition relative to the HP condition. Finally, it was hypothesized that participants randomized to CBSM who endorsed high-baseline levels of cancer-related anxiety, perceived stress, depressive symptoms, interpersonal disruption, and relationship dysfunction, and with metastatic disease, would have significantly greater improvements on HRQOL and symptom burden outcome measures relative to men participating in HP who demonstrated such elevated scores upon entry into the study.
Method
Participants
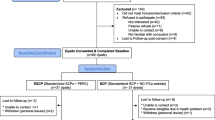
The study CONSORT flow diagram is shown in Fig. 1. Men with APC were recruited from Northwestern Memorial Hospital and the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Rush University Medical Center, the Jesse Brown Veterans Affairs Medical Center, and two Northwestern Medicine locations in Lake County, IL: Lake Forest Hospital and the Grayslake Outpatient Center. Participants were enrolled between January 2013 and November 2016.
Eligible men were 50 years of age or older, fluent in English at the 6th grade level or higher, initially diagnosed with stage III or IV prostate cancer, and had undergone ADT and experienced an ADT-related symptom (e.g., hot flashes, fatigue) within the 12 months immediately prior to study enrollment. Men were excluded if they (1) underwent treatment for any cancer other than prostate cancer or a non-melanoma skin cancer (e.g., basal cell carcinoma) within the past 5 years, (2) reported inpatient psychiatric treatment for mental illness within the past 6 months or were displaying overt signs of severe psychopathology at the time of screening, (3) reported active substance or alcohol dependence issues that would interfere with study participation (per the discretion of the Principal Investigator), (4) were diagnosed with an acute or chronic immune system condition such as lupus or rheumatoid arthritis, (5) had an anticipated life expectancy < 12 months (i.e., the duration of participants’ study participation), or (6) received a score < 20 on the Mini-Mental State Examination at the time of screening [13].
Procedures
The study protocol is available at ClinicalTrials.gov (NCT03149185). Institutional review board approval was received from each study site prior to enrollment, and all participants provided informed consent prior to participation. At baseline (T1), 6 months post-baseline (T2) and 12 months post-baseline (T3) participants attended in-person appointments during which they completed a battery of psychosocial assessments via Assessment CenterSM. Assessment CenterSM is a secure, HIPAA-compliant, online tool for study-specific data capture. In addition, participants provided biological specimens (i.e., blood and saliva samples) in-person, and clinical information was obtained from participants’ medical records at each of these time points. Participants also reported their sociodemographic information at baseline. Participants were recruited and individually randomized (1:1) in groups of 10 to the CBSM [14] or HP condition (n = 5 per condition) using the website www.random.org/lists. Groups containing fewer than 10 men were randomized at the group level to CBSM or HP to ensure sufficient sample size in each group. Research staff enrolled participants and generated the random allocation sequence for randomization. Groups were stratified by disease status (advanced vs. metastatic disease) to address heterogeneity in disease characteristics, such as prognosis. Ultimately, groups were each comprised of four to ten men. Following each weekly meeting, participants completed online assessments of group satisfaction and psychosocial functioning for the duration of the 10-week program via Assessment CenterSM on a study-provided tablet (Samsung Galaxy 2 with 4G connectivity), which was returned post-program with prepaid shipping materials. Assessment completion rates were > 50% at both week 1 and week 10 of the intervention period [15]. Participants were compensated $100 for each in-person assessment and an additional $5 for each weekly post-session online assessment completed.
Multiple accommodations were made to maximize participants’ comfort and success with completing the 10-week program, including (1) providing extensive education about the study’s purpose and goals, (2) providing transportation for in-person assessments and compensation for travel-related expenses, (3) traveling to the site of enrollment for each participants’ in-person assessments, (4) providing flexible scheduling for group sessions, and (5) providing device-specific training for using the study’s technology.
Study Conditions
The CBSM and HP conditions were both group based, manualized, and delivered once per week over the course of 10 weeks via a HIPAA-compliant, web-based platform that was built within the Purple Development Environment [16]. Participants accessed the weekly groups and study-related content on the study-provided tablet. During weekly group sessions, participants had the opportunity to interact with their group facilitator and fellow prostate cancer survivors via WebEx video conferencing software. For rare cases in which participants were not able to attend the video meeting (e.g., low tablet battery or poor connectivity), participants were permitted to call in using a personal phone. Between sessions participants were instructed to review didactic material (e.g., session content) and expert videos (e.g., symptoms of ADT discussed by a urologist), and complete weekly assessments of group satisfaction and psychosocial functioning on the program’s website. Direct links to each of these components were included on the home screen of the study-provided tablet.
CBSM Condition
>CBSM integrates cognitive-behavioral stress- and self-management skills (e.g., cognitive restructuring) with relaxation skills training (e.g., deep breathing) to improve HRQOL and reduce symptoms [14]. We adapted CBSM for men with APC by including disease-relevant examples and didactics (e.g., hot flashes and challenges with sexual functioning) and providing additional skills relevant for men with more advanced disease (e.g., existential concerns and life review). Each weekly group session lasted approximately 90 min. Sessions began with practicing a relaxation technique (30 min) followed by discussion and practice of stress management techniques (60 min). See Table 1 for details of the CBSM condition content. Participants were encouraged to practice the skills taught each week between sessions by completing simple, task-based homework assignments, which were reviewed in the following group session.
HP Condition
The HP condition involved didactic presentations of both general health information and health information specifically relevant to APC. Men randomized to the HP condition were not exposed to any of the stress- or self-management techniques included in the CBSM condition. Each group meeting lasted approximately 60 min. The content of sessions was related to living with APC, and most modules had substantive APC-relevant content (see Table 1 for details). Participants were encouraged to ask questions to assure understanding of the content presented.
Intervention Fidelity
Group facilitators were master’s- or doctoral-level therapists who completed an in-person facilitator training on the manualized treatments. Sessions were audio and video recorded and reviewed in weekly supervision with licensed clinical psychologists who were trained in CBSM and HP.
Measures
Primary Outcome Measures
Quality of Life
Quality of life was measured with the 27-item Functional Assessment of Cancer Therapy-General (FACT-G) scale [17]. Participants indicate the extent to which each item has applied to them over the past 7 days using a five-point scale ranging from not at all to very much, with higher scores indicating better quality of life. The measure yields four subscales reflecting physical, social, emotional, and functional well-being, which can be summed for a total score. The four subscale scores were used for the present analysis. A minimal clinically important difference of two points has been identified for the subscales [18]. The FACT-G is a psychometrically strong measure that is commonly used with oncologic samples. Internal consistency in the present sample was good (subscale αs ranged from 0.73 to 0.84).
Symptom Burden
Prostate Cancer-Specific Symptom Burden
The 50-item Expanded Prostate Cancer Index Composite (EPIC) was used to assess prostate cancer-specific symptom burden, including urinary and sexual functioning [19]. The EPIC was adapted from the widely used UCLA Prostate Cancer Index, and the measure has been extensively used to evaluate symptom burden among men undergoing ADT. The measure evaluates disease-specific components of prostate cancer and its treatment as reflected by four domains: urinary, bowel, sexual, and hormonal. Each domain has a function and bother subscale, which can be summed to yield a summary score. Responses are provided using a Likert scale and are subsequently linearly transformed to a 0–100 scale. Transformed item scores are averaged to yield subscale scores, with higher scores representing less symptom burden. For the present analysis, only the urine bother and function scores and the sexual bother and function scores were used. The urine bother (α = 0.76), sexual bother (α = 0.93), and sexual function (α = 0.89) subscales all evidenced strong internal consistency, and the urine function subscale evidenced acceptable internal consistency (α = 0.67).
Depression
Depression was assessed using the Patient-Reported Outcome Measurement Information System (PROMIS) Depression Item Bank computer adaptive test (CAT) [20]. PROMIS assessments are t scored, so that a mean score of 50 with a standard deviation of 10 represents the average U.S. population score. Higher scores represent more symptoms of depression. The measure has been well validated for use in cancer samples [21, 22].
Fatigue
Fatigue was evaluated with the Fatigue Symptom Inventory [23], a 14-item self-report measure. The perceived interference score, calculated as the average of the seven items assessing the degree to which fatigue has interfered with daily life in the past week, was used in the present analysis. Higher scores indicate greater fatigue. The measure has strong psychometric properties [24]. Internal consistency in the present sample was excellent (α = 0.94).
Pain
Pain was assessed with the short form of the McGill Pain Questionnaire [25]. This measure consists of 15 descriptors, 11 of which evaluate the sensory component of pain and four of which evaluate the affective component thereof. Each is rated on an intensity scale ranging from none to severe. Items are summed to yield a total score, with higher scores indicating more pain. The measure also includes two items assessing overall current pain intensity, which were not included in the present analysis. The measure has good psychometric properties [26], and internal consistency in the present sample was very good (α = 0.89).
Intervention Targets
Stress Management Skills Self-Efficacy
Self-efficacy regarding stress management skills was assessed using select scales from the Measure of Current Status (MOCS) [27], which was specifically developed to assess the effects of CBSM. The measure has two sections. Part A measures participants’ current self-efficacy for skills targeted by CBSM, including relaxing when desired, identifying stressful situations, restructuring maladaptive cognitions, assertively communicating needs, appropriately and effectively expressing anger, and choosing adaptive coping strategies. Part B evaluates possible non-specific CBSM effects, including feelings of normalcy, cohesiveness with other cancer patients, perceptions of care from others, and a view of oneself as being better off than other cancer patients. For the present analysis, the relaxation, awareness of tension, and assertiveness subscales of part A, and the feeling cared for, downward comparison, and bonding subscales of part B were used. The downward comparison subscale demonstrated marginal internal consistency (α = 0.61). All other subscales evidenced strong internal consistency (αs ranged from 0.80 to 0.90).
Cancer-Related Anxiety
The Memorial Anxiety Scale for Prostate Cancer (MAX-PC) is an 18-item self-report measure that assesses symptoms of anxiety in prostate cancer patients [28]. It yields three subscales assessing general anxiety related to prostate cancer, anxiety specific to prostate specific antigen (PSA) testing, and fear of cancer recurrence. Subscales can be summed to yield a total score. Respondents rate the frequency of relevant thoughts and behaviors during the prior week on a scale ranging from not at all to often, with higher scores indicating greater anxiety. The measure has been previously validated in prostate cancer samples. In the present sample, the prostate cancer anxiety (α = 0.93), and fear of recurrence (α = 0.87) subscales both evidenced excellent internal consistency, and the PSA anxiety subscale evidenced poor internal consistency (α = 0.58). Of note, men with metastatic disease were excluded from all analyses evaluating the fear of recurrence subscale.
Positive Affect
A 20-item modified version of the Affect Balance Scale (ABS) was used to assess positive affect [29]. Participants rated the frequency with which they felt various emotions during the past week on a scale ranging from never to always. Items assessing negative affect were reverse coded and then summed to yield a total score, with higher scores indicating greater positive affect. The measure demonstrated excellent internal consistency (α = 0.92).
Interpersonal Disruption
Participants completed a 16-item modified version of the social subscale of the Sickness Impact Profile (SIP) [30]. Participants responded yes or no to items reflecting social withdrawal/disruption, and the percentage of items endorsed was computed. Internal consistency of the items was strong (α = 0.89).
Perceived Stress
The 14-item Perceived Stress Scale (PSS) was used to assess the degree to which participants’ appraised their lives as stressful [31]. Participants rate the frequency with which they experienced thoughts and feelings related to their lives over the prior month on a scale ranging from never to very often. Items that are positively worded are reverse coded prior to scoring, and items are then summed to yield a single total score with higher scores indicating greater stress. The measure had strong internal consistency (α = 0.82).
Cancer-Specific Distress
The 22-item Impact of Events Scale-Revised (IES-R) was used to evaluate cancer-specific distress [32]. Participants rate the level of distress caused by intrusive thoughts, avoidance, and hyperarousal over the prior week on a five-point response scale ranging from not at all to extremely. The measure yields three subscales and one total score, with higher scores reflecting greater distress. The measure has adequate psychometric properties in cancer samples [33], and evidence was found for excellent internal consistency reliability in the present sample for the intrusions (α = 0.85), avoidance (α = 0.82), and hyperarousal (α = 0.81) subscales, as well as the total score (α = 0.92).
Moderators
In addition to the measure listed below, select primary outcomes and intervention targets were evaluated as potential moderators, including cancer-related anxiety, perceived stress, depression, and interpersonal disruption. Group stratification (i.e., metastatic vs. advanced disease) was also explored as a potential moderator.
Relationship Functioning
The six-item sexual functioning subscale of the self-report version of the Psychosocial Adjustment to Illness Scale (PAIS) [34] was used to evaluate relationship and sexual functioning among participants who reported being in a committed relationship. The measure contains items evaluating sexual interest, frequency, quality of performance, and degree of satisfaction, with higher scores indicating greater sexual and relationship functioning. Internal consistency reliability was good (α = 0.78).
Covariates
Demographic variables including age, marital status, race, employment status, and family income were collected via participant self-report at baseline. Medical variables including receipt of any cancer treatment at each time point and years since cancer diagnosis were abstracted from electronic medical records. Additionally, at each time point, patients reported the date of their most recent ADT treatment and provided information about medical comorbidities. These comorbidities were combined into a single, weighted index score using the weighting scheme from the Charlson Comorbidity Index [35], wherein higher scores indicate greater medical comorbidity.
Analytic Plan
Multilevel modeling (MLM) with restricted maximum likelihood estimation was used to evaluate significant mean differences in primary study outcomes and intervention targets over time between the CBSM and HP groups. MLM was selected rather than other mean-comparison approaches, such as ANOVA, as it enables inclusion of participants with missing data at some time points, allowing for utilization of all available data. All analyses were conducted using an intent-to-treat approach. The required sample size was calculated using two-group latent growth models where the effects of interest were change over time in HRQOL and symptom burden. For power > 0.85 for these outcomes and an alpha level of 0.05, 150 participants were required at T3.
In the present analyses, time was treated as a continuous variable (0, 1, 2) and study condition was dummy coded (reference = HP). Models evaluating changes in the primary study outcomes and the intervention targets included all main effects as well as a time-by-condition interaction term. Significant cross-level two-way interactions were probed by calculating simple slopes using a publicly available online calculator (http://www.quantpsy.org/interact/hlm2.htm) [36]. Models where the time-by-condition interaction was not statistically significant were re-specified without the interaction term to enable evaluation of time and condition main effects. Main effects were not interpreted in the presence of significant two-way interactions.
In addition to evaluating intervention effects on the primary study outcomes and intervention targets, secondary analyses were conducted in which six variables were evaluated as potential moderators of the intervention effects. These moderators included baseline scores on measures of cancer-related anxiety (MAX-PC total score), perceived stress (PSS), depression (PROMIS depression CAT), interpersonal disruption (SIP), and relationship functioning (PAIS), as well as group stratification by disease stage (advanced vs. metastatic disease; effect coded). These moderation models included a three-way time-by-condition-by-moderator interaction, and all relevant two-way interactions and main effects. Significant three-way interactions were again probed using a publicly available online calculator (http://www.quantpsy.org/interact/hlm3.htm) [36]. Two-way time-by-condition interactions predicting the study’s primary outcomes, as described above, were not interpreted in the presence of significant three-way interactions.
Across all analyses models controlled for the sociodemographic and disease-related variables that were significantly associated with the model’s outcome. The number of days between the patient’s scheduled session 10 and their T2 assessment and group stratification were also included as covariates when associated with a given model’s outcome. In all analyses, categorical covariates were effect coded and continuous covariates were grand mean centered prior to analysis.
Results
Participant characteristics are presented in Table 2. The mean age of the sample was approximately 68 years, and more than one-third identified as Black. The majority of participants were married or living equivalently, had an annual household income ≥ $35,000, and were not working. Slightly less than half of the sample participated in a group for men with metastatic (vs. advanced) disease, and the average time since diagnosis approached 5 years. There were no statistically significant differences across groups on baseline sociodemographic or medical covariates. Compared with participants in HP, those in CBSM had significantly lower EPIC sexual function scores (t[162] = − 2.00, p = 0.048 [MCBSM = 9.80; MHP = 14.97]), lower MOCS assertiveness scores (t[186] = −2.91, p = 0.004 [MCBSM = 2.47; MHP = 2.91]), higher MAX-PC total scores (t[169] = 2.30, p = 0.023 [MCBSM = 13.07; MHP = 9.39]), and higher MAX-PC fear of recurrence scores (t[98] = 2.63, p = 0.010 [MCBSM = 4.67; MHP = 3.22]) at baseline. There were no other statistically significant differences across conditions at baseline.
Treatment Attendance and Attrition
The vast majority of the sample (81%) completed at least six of the ten weekly sessions, with an average attendance of more than seven sessions. Of the men assigned to CBSM, 52 (54.7%) attended nine or ten sessions, 19 (20.0%) attended seven or eight sessions, 14 (14.7%) attended between two and six sessions, and 10 (10.6%) attended between zero and one sessions. Of the men assigned to HP, 59 (60.8%) attended nine or ten sessions, 17 (17.5%) attended seven or eight sessions, 14 (14.4%) attended between two and six sessions, and seven (7.2%) attended between zero and one sessions.
Participants who were lost to follow-up prior to the T3 assessment significantly differed from those who completed all study assessments on numerous variables. Specifically, those who were lost to follow-up were more likely to be in a metastatic (vs. advanced disease) group (χ2(1) = 5.61, p = 0.018) and were more likely to have received some form of cancer treatment between T2 and T3 (χ2(1) = 7.00, p = 0.008). Additionally, relative to those who were retained, participants who were lost to follow-up attended significantly fewer weekly sessions (t[45] = − 3.48, p = 0.001 [MRetained[R] = 8.12; MLost to follow-up[LTF] = 5.86], and demonstrated worse functioning at baseline on most primary outcome and intervention target variables (see Table 3).
Results for Covariates Included in All Models
Table 4 shows the results of models predicting the primary outcomes as a function of only the covariates. Age and comorbidity were related to multiple study outcomes, in that participants who were older and had less medical comorbidity reported better HRQOL and less symptom burden. Men in a metastatic (vs. advanced disease) group reported better urinary functioning and less sexual bother. Married men also reported less sexual bother, as well as higher social well-being and less pain. Finally, White participants reported lower emotional well-being, worse sexual function, and greater depressive symptoms, and men reporting higher incomes also reported greater depressive symptoms.
Intervention Effects on Primary Outcomes
Table 5 shows the estimated marginal means and associated standard errors for the primary outcome variables, which were estimated at the means of the included covariates.
Quality of Life
There were no statistically significant main effects or interactions on changes in FACT-G scores.
Symptom Burden
There was a significant main effect of time for the EPIC Sexual Function subscale after controlling for marital status, race, receipt of any cancer treatment prior to T1, age, and years since cancer diagnosis (F[1, 316] = 5.16, p = 0.024). Across both conditions, sexual functioning scores decreased over time (b = − 1.81, SE = 0.80; see Table 5). No other main effects or interactions were associated with changes in the other symptom burden subscales.
Intervention Effects on Intervention Targets
Table 6 shows the estimated marginal means and associated standard errors for intervention targets, which were estimated at the means of the included covariates.
There was a significant group-by-time interaction on changes in the MOCS relaxation subscale (F[1, 306] = 12.74, p < 0.001). Simple slopes analysis demonstrated that scores significantly increased over time for the CBSM group (b = 0.43, p < .001), though there was no significant change over time for the HP group (b = 0.05, p = 0.491). There were no other significant group-by-time interactions on changes in other intervention targets.
However, there were significant main effects of time on changes of MAX-PC, IES-R, and MOCS scores. Specifically, there were significant main effects of time on the MAX-PC total score after adjusting for age and years since diagnosis (F[1, 275] = 15.35, p < 0.001), the MAX-PC prostate cancer anxiety subscale after adjusting for age and years since diagnosis (F[1, 314] = 12.23, p = 0.001), the MAX-PC PSA anxiety subscale after adjusting for years since diagnosis (F[1, 311] = 10.96, p = 0.001), and the MAX-PC fear of recurrence subscale after adjusting for age (F[1, 176] = 7.68, p = 0.006). Across all MAX-PC subscales, scores decreased over time for both study groups (total score: b = − 1.08, SE = 0.28; prostate cancer anxiety: b = − 0.74, SE = 0.21; PSA anxiety: b = − 0.17, SE = 0.05; fear of recurrence: b = − 0.32, SE = 0.11; see Table 6).
Similarly, there were significant main effects of time on changes of the IES-R total score after adjusting for age and comorbidities (F[1, 320] = 3.91, p = 0.049), the IES-R intrusion subscale after adjusting for age, comorbidities, and years since diagnosis (F[1, 313] = 6.65, p = 0.010), and the IES-R hyperarousal subscale after adjusting for age, comorbidities, and years since diagnosis (F[1, 298] = 6.26, p = 0.013). Across all IES-R subscales, scores decreased over time for both study groups (total score: b = − 0.75, SE = 0.38; intrusion: b = − 0.05, SE = 0.02; hyperarousal: b = − 0.05, SE = 0.02; see Table 6).
Finally, there was a significant main effect of time on changes on the MOCS bonding subscale after adjusting for comorbidities (F[1, 336] = 6.29, p = 0.013), with scores increasing over time for both study groups (b = 0.09, SE = 0.04). There was also a main effect of study condition on changes of the MOCS assertiveness scale after adjusting for months since most recent ADT treatment (F[1, 186] = 6.19, p = 0.014), with men in the CBSM condition reporting less baseline assertiveness than men in the HP condition (see Table 5). There were no other main effects of time or study condition on changes in the other intervention targets.
Moderation Models
Of the potential moderators explored, three significant three-way interactions emerged.
Group Stratification
There was a significant three-way interaction with group stratification (advanced vs. metastatic disease) as the moderator for the model predicting FSI scores after adjusting for comorbidities (F[1, 313] = 8.37, p = 0.004). Fatigue scores significantly increased over time for men in HP who were in a metastatic disease group (b = 2.07, p = 0.042), but scores did not change for men in CBSM in an advanced disease group (b = 1.21, p = 0.143), men in CBSM in a metastatic disease group (b = −1.05, p = 0.334), or men in HP in an advanced disease group (b = − 1.17, p = 0.168).
Interpersonal Disruption
There was a significant three-way interaction with SIP scores as the moderator for the model predicting PROMIS depression scores after adjusting for race, prostate cancer treatment history, age, and comorbidities (F[1, 314] = 6.39, p = 0.012). Depression scores significantly increased among men in CBSM who reported low baseline interpersonal disruption (b = 2.22, p < 0.001), whereas depression scores significantly decreased among men in CBSM who reported high-baseline interpersonal disruption (b = − 1.63, p = 0.014). Depression scores did not change over time for men in HP who reported low (b = 0.76, p = 0.201) or high (b = − 0.17, p = 0.778) baseline interpersonal disruption.
Relationship Functioning
There was a significant three-way interaction with PAIS sexual function subscale scores as the moderator for the model predicting FACT social well-being after adjusting for marital status, race, and income (F[1, 195] = 4.00, p = 0.047). Social well-being significantly improved for men in CBSM who reported low baseline sexual functioning (b = 1.00, p = 0.006), and there was a trend toward increased social well-being for men in HP who reported high-baseline sexual functioning (b = 0.74, p = 0.073). Social well-being did not change over time for men in HP who reported low baseline sexual functioning (b = − 0.23, p = 0.594) or for men in CBSM who had high-baseline sexual functioning (b = 0.39, p = 0.326).
Discussion
The present study compared the efficacy of a 10-week, web-based CBSM intervention program with a 10-week, web-based HP active control condition. This work extends the literature by evaluating the longitudinal efficacy of CBSM over 12 months, targeting men with APC rather than those with localized disease, and testing a web-based adaptation of CBSM. The web-based administration allowed participants the flexibility of joining the therapist-led group sessions from their homes or other locations, and therefore addressed a significant obstacle for individuals who may otherwise be unable to pursue psychosocial care.
The hypothesized impact of CBSM, relative to HP, on the study’s primary outcomes was not supported. Men randomized to the CBSM group did not demonstrate significant improvements in HRQOL or symptom burden over time relative to those in the HP group. Prior unpublished analysis has suggested that six sessions of CBSM are the minimum therapeutic dose needed to yield observable changes in outcomes. Therefore, all analyses examining the relationships of study condition to the primary study outcomes were repeated including only those men who completed at least six of the ten weekly group sessions. Furthermore, given that the intervention had not previously been explored in a large trial among men with advanced disease, we also conducted these analyses with men who had attended at least seven and at least eight of the ten weekly sessions to allow for the possibility that the minimum effective treatment dose may be higher in this population. However, results did not differ from the intent-to-treat analyses, indicating that these findings were not related to intervention drop out. Of note, the observed baseline mean scores on the FACT-G were higher in this sample than the established population norms, both for patients with cancer and for the general population [37]. This may help explain the lack of significant findings across groups, as these high-baseline levels of HRQOL likely diminished the opportunity for HRQOL improvement. These findings are discrepant from prior research demonstrating the efficacy of CBSM in improving HRQOL and symptom burden among men with localized prostate cancer [10, 11, 38]. However, this discrepancy may be reflective of methodological differences in study design. Prior studies of CBSM among men with localized prostate cancer have generally utilized more passive control conditions, such as single-day or half-day educational seminars. The present study incorporated an attention-matched, active comparison condition wherein participants received notably more resources than in prior studies. Thus, intervention effects may have been limited by improvements observed in men randomized to the active comparison condition, as has been seen in other studies with cancer survivors [39]. An additional finding was that sexual functioning scores declined over time. Given that all participants enrolled in the study were receiving or had recently received ADT, the decline in sexual functioning may be reflective of treatment-related side effects [40]. However, despite this observed decline in sexual functioning, sexual bother scores did not significantly change. Therefore, it is possible that despite worsening sexual functioning, the group-based participation in both CBSM and HP contributed to normalized expectations.
Regarding observed changes in intervention targets, relative to men in the HP condition, men in the CBSM condition evidenced a significant increase in self-reported ability to relax when desired. Studies have demonstrated that CBSM supports enhanced relaxation skills in individuals with HIV [41], increased benefit finding and HRQOL in localized prostate cancer patients [38], and lower cancer-specific anxiety in women with breast cancer [42]. In addition, significant decreases in anxiety related to prostate cancer, anxiety specific to PSA testing, distress caused by intrusive thoughts and hyperarousal, and fear of cancer recurrence, as well as a significant increase in reported feelings of cohesiveness with other cancer patients were observed across groups, suggesting that men in both conditions benefitted from participating in the groups. In the present study, both groups received information to enhance understanding of APC, including information on managing hormone-related side effects, accessing health information, and the importance of follow-up care given documented deficits in knowledge of appropriate APC management [43]. This psychoeducation may have improved understanding of APC, thus contributing to decreased distress, across groups [44]. Additionally, participants in both conditions met in small groups with other individuals going through similar life experiences. This supportive social environment may have increased perceived social support for all participants regardless of group assignment. Social support has previously been linked with positive psychological adjustment and higher mental and physical HRQOL in individuals with cancer [45,46,47] and thus may have contributed to the observed improvements in intervention targets across conditions.
Several moderating factors were identified. While individuals in the CBSM condition who reported low baseline interpersonal disruption demonstrated a significant increase in depression scores, individuals in the same condition with high-baseline interpersonal disruption demonstrated a significant decrease in depression scores. This distinction could be reflective of the material presented in the CBSM group, which may have brought to light interpersonal struggles commonly experienced by men with APC. Such insight could have contributed to increased distress among men with low baseline interpersonal disruption, while helping those individuals already aware of their relational difficulties. Additionally, men in the CBSM condition reported a constant level of fatigue over time regardless of disease stage, whereas men with metastatic disease (as opposed to advanced disease) in the HP condition demonstrated worse fatigue over time. This indicates that CBSM may have buffered against worsening fatigue for men with more severe illness, while HP did not. Lastly, men in the CBSM condition with low baseline levels of sexual functioning reported significantly improved levels of social well-being over time. As the CBSM condition included a more extensive discussion of sexual functioning than the HP condition, men low in sexual functioning may have derived more benefit from this material. These findings suggest the need for more personalized and nuanced psychosocial interventions to target outcomes in a more efficacious, direct manner.
Sociodemographic moderators were not evaluated in the present analysis; however, Bouchard and colleagues [48] previously evaluated the efficacy of CBSM by race using data also reported by the present sample. These authors found support for the feasibility and efficacy of CBSM across Black and non-Hispanic White participants, demonstrating that study retention and group attendance did not significantly differ by race, and that both CBSM and HP were rated as acceptable by all study participants. Additionally, prostate cancer-specific anxiety significantly decreased over time among Black men randomized to the CBSM condition, but not among Black men randomized to the HP condition or non-Hispanic White men in either study condition. These authors also found that race was closely related to recruitment site, with significantly more Black participants recruited from the VA medical center as opposed to an academic medical center, as well as to indicators of socioeconomic status, including income and education. Their findings suggest that other sociodemographic variables may be significant moderators of treatment effects in the present sample. Formal exploration of this is warranted in future analyses.
Of particular note, significant differences were observed between men who completed study participation and those who were lost to follow-up. Men who did not complete the T3 assessment demonstrated significantly more symptom burden and were generally more medically compromised at baseline. Additionally, these men attended significantly fewer intervention sessions and on average received less than the six sessions posited to achieve intervention efficacy. The high demand of study participation may have contributed to retention of only high functioning, highly motivated, and relatively healthier participants. This result combined with the overall high-baseline HRQOL of the sample suggests that men who were lost to follow-up may have been too ill to benefit from this group-based intervention, while those who engaged in the full study protocol were potentially too healthy to derive significant benefit related to HRQOL and symptom burden. This highlights the importance of tailoring interventions to patients’ baseline level of need, and providing more intensive intervention to those with the greatest deficits in HRQOL and overall functioning.
There are several notable strengths of this study including the longitudinal design, inclusion of an active control condition (HP), a large and racially diverse sample of participants, and the novel aspect of a web-delivered intervention. There are also several limitations worth noting. Study findings are limited to men receiving ADT for APC. Furthermore, all men in the study were provided with a tablet which limits the generalizability of the study findings.
In summary, findings from this study suggest that a web-based adaptation of CBSM for men with APC was well received among study participants. The lack of statistically significant improvement in HRQOL across both study conditions may be attributed to the high levels of HRQOL at study baseline, as well as attrition of those patients with more severe symptoms at baseline. Significant improvements in intervention targets were observed among men randomized to both the CBSM and HP conditions, perhaps due in part to the supportive, group-based delivery of the interventions and the specific psychoeducation provided related to living optimally with APC. Furthermore, several moderating factors were identified that should be considered for future development and implementation of interventions that are tailored to patients’ initial levels of HRQOL and symptom burden.
References
American Cancer Society. Cancer Facts & Figures 2018. Atlanta: American Cancer Society; 2018.
Chen RC, Chang P, Vetter RJ, et al. Recommended patient-reported core set of symptoms to measure in prostate cancer treatment trials. J Natl Cancer Inst. 2014;106:dju132.
Sonn GA, Sadetsky N, Presti JC, Litwin MS. Differing perceptions of quality of life in patients with prostate cancer and their doctors. J Urol. 2013;189:S59–65.
Warde P, Mason M, Ding K, et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet. 2011;378:2104–11.
Zajdlewicz L, Hyde MK, Lepore SJ, Gardiner RA, Chambers SK. Health-related quality of life after the diagnosis of locally advanced or advanced prostate cancer: a longitudinal study. Cancer Nurs. 2017;40:412–9.
Perlmutter MA, Lepor H. Androgen deprivation therapy in the treatment of advanced prostate cancer. Rev Urol. 2007;9(Suppl 1):S3–8.
Potosky AL, Reeve BB, Clegg LX, Hoffman RM, Stephenson RA, Albertsen PC, et al. Quality of life following localized prostate cancer treated initially with androgen deprivation therapy or no therapy. J Natl Cancer Inst. 2002;94(6):430–7.
Sheinfeld Gorin S, Krebs P, Gadr H. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol. 2012;30:539–47.
de la Torre-Luque A, Gambara H, López E, Cruzado JA. Psychological treatments to improve quality of life in cancer contexts: a meta-analysis. Int J Clin Health Psychol. 2016;16:211–9.
Penedo FJ, Dahn JR, Molton I, Gonzalez JS, Kinsinger D, Roos BA, et al. Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer. 2004;100:192–200.
Traeger L, Penedo FJ, Gonzalez JS, Dahn JR, Lechner SC, Schneiderman N, et al. Illness perceptions and emotional well-being in men treated for localized prostate cancer. J Psychosom Res. 2009;67:389–97.
Parahoo K, McDonough S, McCaughan E. Psychosocial interventions for men with prostate cancer: a Cochrane systematic review. BJU Int. 2015;116:174–83.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Penedo FJ, Antoni MH, Schneiderman N. Cognitive-behavioral stress management for prostate cancer recovery facilitator guide. New York: Oxford University Press; 2008.
Fox RS, Moreno PI, Yanez B, et al. Integrating PROMIS® computerized adaptive tests into a web-based intervention for prostate cancer. Health Psychol. 2019;38:403–9.
Schueller SM, Begale M, Penedo FJ, Mohr DC. Purple: a modular system for developing and deploying behavioral intervention technologies. J Med Internet Res. 2014;16:e181.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9.
Brucker PS, Yost K, Cashy J, Webster K, Cella D. General population and cancer patient norms for the functional assessment of cancer therapy-general (FACT-G). Eval Health Prof. 2005;28:192–211.
Wei JR, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905.
Ader DN. Developing the Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care. 2007;45:S1–2.
Schalet BD, Pilkonis PA, Yu L, et al. Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. J Clin Epidemiol. 2016;73:119–27.
Clover K, Lambert SD, Oldmeadow C, et al. PROMIS depression measures perform similarly to legacy measures relative to a structured diagnostic interview for depression in cancer patients. Qual Life Res. 2018;27:1357–67.
Hann DM, Jacobsen PB, Azzarello LM, Martin SC, Curran SL, Fields KK, et al. Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7:301–10.
Donovan KA, Jacobsen PB. The fatigue symptom inventory: a systematic review of its psychometric properties. Support Care Cancer. 2011;19:169–85.
Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7.
Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill Pain Questionnaire: an overview of psychometric properties. Phys Ther Rev. 2005;10:123–8.
Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, et al. How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psychol. 2006;74:1143–52.
Roth AJ, Rosenfield B, Kornblith AB, et al. The Memorial Anxiety Scale for Prostate Cancer: validation of a new scale to measure anxiety in men with with prostate cancer. Cancer. 2003;97:2910–8.
Bradburn N. The structure of psychological well-being. Chicago: Aldine; 1969.
Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19:787–805.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Weiss DS, Marmar CR. The impact of event scale – revised. In: Wilson JP, Tang CS, editors. Psychological trauma and PTSD. New York: Guilford Press; 1997. p. 399–411.
Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, et al. Outcomes from the moving beyond cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23:6009–18.
Derogatis LR. The psychosocial adjustment to illness scale (PAIS). J Psychosom Res. 1986;30:77–91.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51.
Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:437–48.
Pearman T, Yanez B, Peipert J, Wortman K, Beaumont J, Cella D. Ambulatory cancer and US general population reference values and cutoff scores for the functional assessment of cancer therapy. Cancer. 2014;120:2902–9.
Penedo FJ, Molton I, Dahn JR, Shen BJ, Kinsinger D, Traeger L, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31:261–70.
Greer JA, Jacobs J, Pensak N, MacDonald J, Fuh CX, Perez GK, et al. Randomzied trial of a tailored cognitive-behavioral therapy mobile application for anxiety in patients with incurable cancer. Oncologist. 2019;24:1111–20.
Huang GJ, Sadetsky N, Penson DF. Health related quality of life for men treated for localized prostate cancer with long-term follow-up. J Urol. 2010;183:2206–12.
Antoni MH. Stress management effects on psychological, endocrinological, and immune functioning in men with HIV infection: empirical support for a psychoneuroimmunological model. Stress. 2003;6:173–88.
Antoni MH, Lechner S, Diaz A, et al. Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain Behav Immun. 2009;23:580–91.
Walker LM, Tran S, Wassersug RJ, Thomas B, Robinson JW. Patients and partners lack knowledge of androgen deprivation therapy side effects. Urol Oncol. 2013;31:1098–105.
Wu PH, Chen SW, Huang WT, Chang SC, Hsu MC. Effects of a psychoeducational intervention in patients with breast cancer undergoing chemotherapy. J Nurs Res. 2018;26:266–79.
Karnell LH, Christensen AJ, Rosenthal EL, Magnuson JS, Funk GF. Influence of social support on health-related quality of life outcomes in head and neck cancer. Head Neck. 2007;29:143–6.
Filazoglu G, Griva K. Coping and social support and health related quality of life in women with breast cancer in Turkey. Psychol Health Med. 2008;13:559–73.
Leung J, Pachana NA, McLaughlin D. Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology. 2014;23:1014–20.
Bouchard LC, Yanez B, Dahn JR, et al. Brief report of a tablet-delivered psychosocial intervention for men with advanced prostate cancer: acceptability and efficacy by race. Transl Behav Med. 2019;9:629–37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Penedo, F.J., Fox, R.S., Oswald, L.B. et al. Technology-Based Psychosocial Intervention to Improve Quality of Life and Reduce Symptom Burden in Men with Advanced Prostate Cancer: Results from a Randomized Controlled Trial. Int.J. Behav. Med. 27, 490–505 (2020). https://doi.org/10.1007/s12529-019-09839-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-019-09839-7