Abstract
Background
Quality of life (QOL) impairments are common in patients undergoing dialysis, and have been strongly associated with significant clinical outcomes like mortality and morbidity. Despite this, little is known about the course of QOL over time, especially for patients on peritoneal dialysis (PD).
Purpose
This prospective study was set to explore course and determinants of QOL over 12 months in PD patients.
Methods
A total of 115 PD patients completed the SF-12 and Kidney Disease Quality of Life Short Form (KDQOL-SF) at baseline and 12 months later. Intra-individual changes in physical (physical component summary, PCS), mental (mental component summary, MCS), and Kidney Disease Component Summary scores (KDCS) were identified based on the minimally important clinical difference threshold. Clinical information was extracted from medical records.
Results
Of the patients, 74–80 % reported physical QOL impairments, as compared to 29–33 % who reported mental/emotional QOL impairments. PCS and MCS scores remained stable across 12 months. Significant deterioration was noted in the domains of patient satisfaction, staff encouragement, and social support, while there were significant increases in the perceived effects of kidney disease. Intra-individual trajectory analyses indicated that one in three patients reported deteriorating QOL. No sociodemographic or clinical variables were found to be associated with course of outcomes.
Conclusions
Although PD offers the convenience of home-based care, it is associated with persisting QOL impairments and diminishing QOL over time, especially in domains related to quality of care and support. This highlights the need for improving or maintaining standards of care and support for PD patients as they become increasingly established on their regimes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For the majority of patients with end-stage renal disease, dialysis is a lifelong treatment commonly associated with increased impairments in their quality of life (QOL) [1, 2]. Home-based modalities like peritoneal dialysis (PD) are thought to offer enhanced opportunities for autonomy, rehabilitation, and return to work, with flexibility in dialysis schedules in addition to cost savings and good clinical outcomes [3]. Attention has therefore been directed to increase the uptake of PD, which, in most settings, still remains underutilized relative to hemodialysis (HD) [4].
From the patients’ perspective, however, the PD regimen is often seen as time- and labor-intensive [5, 6]—involving the onerous commitment to daily self-care or caregiver-administered dialysis exchanges, alongside fluid and diet restrictions, and the management of multiple medications [7]—which often results in dwindling motivation, non-adherence, and a deteriorating QOL. Because of strong associations between poor QOL and clinical endpoints [8–10], such as hospitalization and mortality [11–14], QOL measures provide important information on the effectiveness of PD [15]. Various efforts have been initiated to improve patients’ QOL, such as adjusting dialysis prescription, controlling comorbidities, treating anemia, and alleviating depression [16]; however, while necessary [17], little is known about the progress of QOL over time.
The literature on QOL in PD patients is dominated by cross-sectional studies [18–20], with only a handful of longitudinal studies investigating the course of QOL over time [21], and even then, with conflicting evidence. Studies on incident PD patients in Brazil, USA, or Netherlands reported either no change for patients [22], improvements [23], or declines in physical but not mental health-related QOL (HRQOL) over 12 months [24]. Studies on prevalent PD patients reported either no changes [25] or steady declines in both physical and mental HRQOL, as well as in disease-specific QOL (DSQOL) of symptoms and burden of kidney disease and patient satisfaction over 2 years [15]. At present, there are no longitudinal studies in Asian PD patients, despite suggestions that Indo-Asian immigrants score lower on QOL measures than their Caucasian counterparts [15]. This is particularly important given the higher prevalence rates of ESRD in Asian populations, the growth of PD in China and Asia [26], and the surge of Asian minorities in Western settings.
Furthermore, only limited conclusions can be drawn from previous work, as group-based analyses may mask variation in individuals; it is thus possible that while QOL improves over time for some patients, for others, QOL impairments can persist or even worsen. It is therefore imperative to document both group and individual patterns of change and identify factors that may be associated with course of QOL outcomes to guide clinical care.
The aims of this prospective study were (1) to document the course of QOL outcomes over 12 months in Asian patients already on PD in Singapore, (2) to determine individual trajectories of QOL outcomes over time, and (3) to investigate the associations between course of outcomes and various sociodemographic and clinical variables. Because evidence is lacking and inconsistent, no a priori directional hypotheses with respect to changes of QOL over time or potential correlates were formulated; this exploratory study therefore sought to generate hypotheses for future research.
Methodology
Design
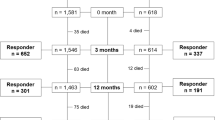
This study is part of a larger prospective study on maintenance dialysis patients receiving outpatient treatment from the largest national PD center in Singapore [27, 28]. The present study reports data on PD patients from the baseline cohort (N = 201) that were reassessed 12 months later using the same instruments.
Participants and Procedures
All eligible participants from baseline cohort were recruited for follow-up during their regularly scheduled appointments at the Peritoneal Dialysis Centre at Singapore General Hospital between October 2011 and June 2012 (at 12.0 ± 3.3 months since baseline assessment). Patients were included if aged 21 or over, on PD for a minimum of 3 months, and able to communicate verbally and provide informed consent. Patients who were no longer on PD, those diagnosed with dementia or other cognitive impairment, or those hospitalized at the time of assessment were excluded. The study was approved by Centralized Institutional Review Board, SingHealth Research Facilities (reference number: 2010/588/E), and informed consent was obtained from all individual participants included in the study.
Of the 201 patients recruited at baseline, a total of 86 (43 %) were no longer eligible or available to participate: 19 were deceased (survival rate = 91 %), 18 were no longer on PD (14 switched to HD and 4 had a kidney transplant), 11 were uncountable, hence lost to follow-up, and the remainder declined participation (n = 38), most commonly citing loss of interest or motivation. Non-responders were found to be older (p = 0.004), and those who had passed away reported lower levels of physical QOL at baseline as compared to those who had followed-up (p = 0.1); no other significant differences were found. The final study sample comprised the 115 patients on PD (55 % continuous ambulatory PD [CAPD]; 55 % women; 70 % married; 67 % unemployed) who completed both the baseline and 12-month follow-up questionnaires (follow-up rate = 54 %; response rate = 75 %). Table 1 summarizes the participants’ baseline sociodemographic and clinical characteristics of the total sample at follow-up used in the present study.
Study Instruments
Quality of Life
HRQOL was operationalized with version 1.3 of the Kidney Disease Quality of Life Short Form (KDQOL-SF) [29]. The SF-36 in the original KDQOL-SF questionnaire was replaced by its shorter version [30], SF-12 [31], as done elsewhere [32], to reduce participants’ burden of completion. As per scoring procedures [33], two summary scores, the physical component summary (PCS) and mental component summary (MCS) scores were calculated. PCS and MCS scores ranged from 0 to 100, with higher scores representing better physical and mental/emotional well-being, respectively. These scores were then compared against available local SF-36 PCS and MCS norms [34, 35], as justified elsewhere [19]; scores below one standard deviation of local norms were considered impaired. The ESRD-specific portion of the KDQOL-SF measuring DSQOL consisted of 31 items across six domains: symptoms, effects, and burden of kidney disease; patient satisfaction; staff encouragement; and social support. Scores on each domain was transformed to a scale of 0–100, with higher scores indicating better QOL. As per scoring guidelines [29], an aggregate was also calculated to determine a Kidney Disease Component Summary (KDCS) score.
Demographics and medical information
Participants reported information on age, gender, relationship status, race/ethnicity, employment status, educational level, and household monthly income. Medical notes were reviewed to record serological data (e.g., serum potassium and phosphate levels), comorbidities, and other relevant clinical or treatment details (e.g., primary cause of ESRD, PD modality, dialysis vintage, residual renal function markers, etc.). The Charlson Comorbidity Index (CCI) was used to consolidate comorbidity burden, computed pursuant to ESRD-specific methods [36, 37].
Data Analysis
Data were analyzed using SPSS Version 22 (SPSS Inc., Chicago, IL), and all p values below .05 were considered statistically significant. Missing data were infrequent and randomly distributed; mean scores were computed only if patients answered at least half of the items in the same domain. McNemar’s test determined changes in the proportions of QOL impairments over time. QOL was determined to have improved or declined if it exceeded the threshold for the clinically significant difference (i.e., ±0.5 SD of baseline) [38, 39].
Previous work has used various statistical techniques to evaluate the course of QOL over time. Because of the modest sample size, as previously done elsewhere [15], the present study employed analyses of covariance (ANCOVAs) to determine changes in QOL over time, controlling only for sociodemographic and clinical variables that were significantly associated with QOL at p < .05. To determine these univariate associations, Pearson’s correlations, independent samples t tests, one-way analyses of variance (ANOVAs) with Tukey-corrected post hoc analyses, and chi-square analyses were employed (as appropriate for data).
Results
Prevalence of HRQOL Impairments from Baseline to Follow-up
Preliminary analyses revealed that close to four in five patients (baseline, 74 %; follow-up, 80 %) experienced significant physical QOL impairments (as compared to the general local population) over 12 months (PCS, Z = −0.5, p = 0.6). One in three patients (baseline, 33 %; follow-up, 29 %) experienced mental/emotional QOL impairments across the same time period (MCS, Z = −0.7, p = 0.5). Both PCS and MCS scores were thus significantly lower than local population norms at both baseline and follow-up (PCS, ts[113] = −16.2, ps < .001; MCS, ts[114] = −2.8 to −16.2, ps ≤ .006); PCS scores were also significantly more impaired than MCS scores across the time period (t[113] = −7.8 to −8.0, p < .001; see Table 2).
Associations between QOL and Sociodemographic and Clinical Variables
There were some significant associations between QOL domains and socio-demographic and clinical parameters, albeit not consistently across all QOL domains.
PCS scores were affected by age (r[114] = −.22, p = .03), dependence on caregiver (t[112] = 2.58, p = .01), diabetes as a primary cause for ESRD (p < .001), pill burden (r[114] = −.22, p = .02), CCI (r[114] = −.36, p < .001), creatinine levels (r[114] = −.25, p = .009), and dialysis adequacy (r[114] = .27, p = .003). MCS scores were significantly associated with unemployment (t[112] = −2.66, p = .009), dependence on a caregiver (t[112] = 2.03, p < .05), pill burden (r[114] = −.21, p = .03), and albumin levels (r[114] = .19, p = .04).
KDCS scores and symptoms of kidney disease were associated with dependence on a caregiver status (t[113] = 2.03, p = .02) and CCI (r[115] = −.19, p = .04). Effects of kidney disease was only significantly associated with male gender (t[113] = −2.11, p = .04), and burden of kidney disease was only significantly associated with unemployment (t[113] = −2.07, p = .04) and CCI (r[115] = −.25, p = .008). Finally, staff encouragement was significantly associated Chinese ethnicity (t[90.05] = 4.54, p < .001), dependence on a caregiver (t[113] = 2.18, p = .03), and time on dialysis (r[115] = −.22, p = .02). All these variables were controlled for in subsequent analyses examining the course of QOL over time.
Changes in QOL Over 12 Months
Repeated measure ANCOVAs indicated that HRQOL remained stable across time for PCS (F[1,102] = 0.77, p = 0.38) and MCS scores (F[1,108] = 0.50, p = 0.48; see Table 2). Intra-individual analyses, however, revealed that almost one in three patients had deteriorating HRQOL across 12 months (31–32 %), although a similar proportion of patients also reported HRQOL improvements (35–37 %; see Table 2).
ANCOVA findings revealed significant decreases in DSQOL (indicative of worse DSQOL), particularly in the domains of: satisfaction with care (F[1,113] = 6.33, p = 0.01), staff encouragement (F[1,111] = 16.17, p < 0.001), and effects of kidney disease (F[1,113] = 4.62, p = 0.03). A marginally significant decreasing trend was noted for social support (F[1,114] = 3.64, p = 0.06) (see Table 2).
MCID analyses revealed variation in outcomes with deterioration DSQOL for at least a third of participants (24–42 %) with highest rates for the domains of satisfaction with care and staff encouragement, although almost a third (22–38 %) were observed to report DSQOL improvements.
Associations with Intra-individual Trajectories of QOL Change
No baseline sociodemographic and medical variables (presented in Table 1) were associated with mean change scores or intra-individual trajectories of change in any of the QOL domains or summary scores.
Discussion
This study is one of the few to examine and compare the course of QOL over time in patients on different PD modalities. Similar to other studies [40, 41], our data shows poorer HRQOL in PD patients relative to the general population; a recent review revealed that PD patients’ HRQOL are influenced by a wide range of concerns related to body image, sleep disturbances, family burden, physical limitations, and inability to fulfill social roles [6]. Our data also suggests that these impairments are more pronounced in physical, relative to mental/emotional, HRQOL [18–20]: over the 12 month observation period, impairment rates for PCS scores ranged 74–80 %, while the rates of MCS impairments ranged 29–33 % across the 12 months. These physical QOL impairments may perhaps be related to poor nutritional status in our sample: a total of 70 % of patients in our sample were malnourished (indicated by an albumin level of <3.5 g/dL); nutritional status has been shown to be a critical determinant of physical QOL in previous work [42, 43]. The less dramatic impact on emotional HRQOL is encouraging as it suggests a less profound effect of treatment on emotional well-being in established PD patients. As our sample comprised stock PD patients, it is likely that over time, the negative impacts on mental QOL may have been ameliorated, given that patients may have psychologically adapted to the chronic condition and demands of treatment [44]. This is also consistent with the theory of cognitive adaptation to life-threatening events [45]. However, while there may not have been a worsening HRQOL, patients in our sample still reported increasing effects of the kidney disease on their lives.
Our study findings also indicate that the observed HRQOL impairments do not improve over time. While the lack of further decline is positive, the persistence of QOL impairments is disconcerting: it suggests that these remain largely undetected or unresponsive to usual renal care over 1 year. As shown in other settings [11–13], poor physical HRQOL may explain: first, the lowered 1- and 5-year survival rates for PD (87 and 35 %, respectively), compared to HD patients (90 and 60 %, respectively); second, why only 17 % of incident dialysis patients opted for PD as of 2009; and third, why only 13 % of prevalent dialysis patients were found to be on PD in Singapore [28]. With a rising trend worldwide for the utilization of PD over HD, especially amongst the less independent [46], and with the Singapore government estimating that it would save SGD 25 million per year if the PD utilization rate increases to 40 % [47], the issue of improving QOL is becoming an increasingly pertinent one.
Clinical care in PD is typically structured around achieving clinical targets, reducing PD infections, and improving retention and technique survival; however, more attention should therefore be directed to monitoring QOL levels and potentially tailoring care and services towards incentivizing QOL improvements, strategically expanding the focus on improving patient experience, as these are linked to clinical outcomes like mortality and hospitalization [11–13].
Paramount to this goal is the delivery and perceived quality of care for the established PD patients. Study findings indicate significant declines over the 12 months of observation in patient-reported satisfaction with care and perceived staff encouragement, but stable HRQOL levels. Reduced care satisfaction in stock PD patients was noted in previous work alongside greater HRQOL decline [15], contrasting with cross-sectional data from the CHOICE study in which incident PD patients were 50 % more likely than HD patients to rate their care as excellent [48].
It is thus interesting to speculate on plausible explanations about the deterioration in interpersonal aspects of QOL for prevalent patients. It is plausible that may reflect methodological issues: in the present study, participants were recruited from the largest PD center in Singapore which caters for over more than 500 PD patients [28]. Although it is likely that large settings in general may be linked to increased waiting times and time-restrained consultations, which may influence patient satisfaction [49], all patients were seen by the same consultant and team, so there was continuity in care and, presumably, in rapport. Renal care and support services for PD in the center are in line with other renal settings. These include care by a multi-disciplinary team comprising nurses, clinicians, social workers, and renal dieticians, PD training course for patients and at least one family member to ensure PD competency in the household followed by home visits by nurses, and routine clinic appointment and access to 24-h support line for any queries or emergencies. As such, the observed declines in patient satisfaction and ratings of staff encouragement may reflect aspects of care other than organizational factors or availability of services.
Thus, it may be likely that, over time, with patients becoming long established on PD, the content of front care and consultations may either change towards a format that is no longer as well-aligned with, or not swiftly adapting to, the expectations and needs of PD survivors (e.g., care remaining too static and stale, or becoming more routinized). Pertinent to this are the expectations of both parties, recipients, and providers of care. The success in PD technique survival, albeit commendable and indicated by a reduction in the perceived burden of kidney disease in our sample, may lead to assumptions or expectations of mastery and self-sufficiency in renal health care teams. For instance, healthcare providers (HCPs) may assume mastery of PD procedures for their long-term established patients and hence may not as actively pursue further support and encouragement as with incident patients. The reassurance that patients have been maintained on PD for long might also lead HCPs to become less vigilant or responsive to patients’ needs for sustained education, guidance, empowerment, or affirmation.
Likewise, it could also be that expectations of patients for support by HCPs may increase over time, either due to complications, PD-related burnout in themselves or their family [50–52], or dwindling support from their family. There was a trend of decreased social support in our sample, which implies that as family/interpersonal support wanes over time, patients may place higher expectations towards their renal team. More work is clearly needed to explore these important issues and inform the efforts to maintain and improve quality care over the course of PD.
Study limitations should be noted. Because of the overall attrition rate, sample may have been biased; this is partly due to the high turnover of PD patients, with close to 5 % of the original sample being switched to HD, another 5 % not contactable, and 20 % who were not interested in participating in the follow-up assessment because of poor health and hospitalization. These may have led to an underestimation of the magnitude of QOL effects. Caution should also be taken in interpreting the study findings, as significance levels were not adjusted for multiple comparisons, thereby inflating type I error. The strategy adopted in this study was to be exploratory and generate hypotheses for further research. Because of the modest sample size and power of the analyses, the present study only controlled sociodemographic and clinical variables with significant associations with QOL. Replication with larger samples is hence warranted. Finally, this is a single center study that may limit generalizability in other settings, although the hospital from which the sample was drawn has the largest PD unit catering for the majority of PD patient in Singapore; it is important to note, however, that the socio-demographic and clinical profile (i.e., comorbidities) was comparable to the national PD registry data, allowing some confidence concerning the generalizability of our findings [28] While our Asian patient population is of particular interest due to its high incidence of ESRD and the substantial rates of Asian minorities in Western countries, the widespread generalizability of our observations to other settings or other ethnic populations is unknown and should be explored in future work. Future studies should also look to the influence of caregivers on QOL outcomes; as PD is a home-based therapy, the QOL of the caregivers or cohabiting family members may affect patient outcomes.
References
Billington E, Simpson J, Unwin J, Bray D, Giles D. Does hope predict adjustment to end-stage renal failure and consequent dialysis? Br J Health Psychol. 2008;13:683–99.
Czyżewski L, Sańko-Resmer J, Wyzgał J, Kurowski A. Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant. 2014;19:576–85.
François K, Bargman JM. Evaluating the benefits of home-based peritoneal dialysis. Int J Nephrol Renovasc Dis. 2014;2014:447–55.
Jain AK, Blake P, Cordy P, Garg AX. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–44.
Griva K, Li ZH, Lai AY, Choong MC, Foo MWY. Perspectives of patients, families, and health care professionals on decision-making about dialysis modality-the good, the bad, and the misunderstandings! Perit Dial Int. 2013;33:280–9.
Tong A, Lesmana B, Johnson DW, Wong G, Campbell D, Craig JC. The perspectives of adults living with peritoneal dialysis: thematic synthesis of qualitative studies. Am J Kidney Dis Elsevier Inc. 2013;61:873–88.
Hailey BJ, Moss SB. Compliance behaviour in patients undergoing haemodialysis: a review of the literature. Psychol Health Med. 2000;5:395–406.
Afsar B, Elsurer R, Sezer S, Ozdemir NF. Does metabolic syndrome have an impact on the quality of life and mood of hemodialysis patients? J Ren Nutr National Kidney Foundation, Inc. 2009;19:365–71.
Birmelé B, Le Gall A, Sautenet B, Aguerre C, Camus V. Clinical, sociodemographic, and psychological correlates of health-related quality of life in chronic hemodialysis patients. Psychosomatics Elsevier Inc. 2012;53:30–7.
Santos PR, Daher EF, Silva GB, Libório AB, Kerr LR. Quality of life assessment among haemodialysis patients in a single centre: a 2-year follow-up. Qual Life Res. 2009;18:541–6.
Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH. Association among SF36 quality of life measures and nutrition, hospitalization, and mortality in hemodialysis. J Am Soc Nephrol. 2001;12:2797–806.
Lowrie EG, Curtin RB, LePain N, Schatell D. Medical outcomes study short form-36: a consistent and powerful predictor of morbidity and mortality in dialysis patients. Am J Kidney Dis. 2003;41:1286–92.
Mapes DL, Bragg-Gresham JL, Bommer J, Fukuhara S, McKevitt P, Wikstrom B, et al. Health-related quality of life in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2004;44:54–60.
Lim HA, Griva K. Health-related quality of life outcomes among patients on maintenance dialysis. In: Theophilou P, editor. Outcomes Assess. end-stage kidney Dis. Meas. Appl. Clin. Pract. Sharjah, U.A.E.: Bentham Science Publishers; 2013. p. 47–79.
Bakewell AB, Higgins RM, Edmunds ME. Quality of life in peritoneal dialysis patients: decline over time and association with clinical outcomes. Kidney Int. 2002;61:239–48.
Ross EA, Hollen TL, Fitzgerald BM. Observational study of an Arts-in-Medicine Program in an outpatient hemodialysis unit. Am J Kidney Dis. 2006;47:462–8.
Teixeira JP, Combs SA, Teitelbaum I. Peritoneal dialysis: update on patient survival. Clin Nephrol. 2015;83:1–10.
Bohlke M, Nunes DL, Marini SS, Kitamura C, Andrade M, Von-Gysel MPO. Predictors of quality of life among patients on dialysis in southern Brazil. Sao Paulo Med J. 2008;126:252–6.
Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening Options for Long-term Dialysis in the Elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant. 2010;25:3755–63.
De Wit GA, Merkus MP, Krediet RT, de Charro FT. A comparison of quality of life of patients on automated and continuous ambulatory peritoneal dialysis. Perit Dial Int. 2001;21:306–12.
Joshi VD. Quality of life in end stage renal disease patients. World J Nephrol. 2014;3:308–16.
Dos Santos Grincenkov FR, Fernandes N, Chaoubah A, da Silva FN, Bastos K, Lopes AA, et al. Longitudinal changes in health-related quality of life scores in Brazilian Incident Peritoneal Dialysis Patients (BRAZPD): socio-economic status not a barrier. Perit Dial Int. 2013;33:687–96.
Wu AW, Fink NE, Marsh-Manzi JVR, Meyer KB, Finkelstein FO, Chapman MM, et al. Changes in quality of life during hemodialysis and peritoneal dialysis treatment: generic and disease specific measures. J Am Soc Nephrol. 2004;15:743–53.
Merkus MP, Jager KJ, Dekker FW, de Haan RJ, Boeschoten EW, Krediet RT. Quality of life over time in dialysis: the Netherlands Cooperative Study on the Adequacy of Dialysis. NECOSAD Study Group Kidney Int. 1999;56:720–8.
Mittal SK, Ahern L, Flaster E, Mittal VS, Maesaka JK, Fishbane S. Self-assessed quality of life in peritoneal dialysis patients. Am J Nephrol. 2001;21:215–20.
Fang W, Ni Z, Qian J. Key factors for a high-quality peritoneal dialysis program—the role of the PD team and continuous quality improvement. Perit. Dial. Int. 2014; 34 Suppl 2:S35–42.
Griva K, Kang AW, Yu ZL, Mooppil NK, Foo M, Chan CM, et al. Quality of life and emotional distress between patients on peritoneal dialysis versus community-based hemodialysis. Qual Life Res. 2014;23:57–66.
Health Promotion Board. Eighth report of the Singapore renal registry 2009. Singapore; 2012.
Hays RD, Kallich JD, Mapes DL, Coons SJ, Amin N, Carter WB, et al. Kidney Disease Quality of Life Short Form (KDQOL-SFTM), Version 1.3: a manual for use and scoring. Rand: Santa Monica, CA, USA; 1997.
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care. 1992;30:473–83.
Ware Jr JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
De Abreu MM, Walker DR, Sesso RC, Ferraz MB. Health-related quality of life of patients recieving hemodialysis and peritoneal dialysis in São Paulo, Brazil: a longitudinal study. Value Heal Elsevier Inc. 2011;14:S119–21.
Ware Jr JE, Kosinski M, Keller SD. SF-12: How to score the SF-12 physical and mental health summary scales. New England Medical Center. Quality Metric, Incorporated: The Health Institute; 1998.
Thumboo J, Fong KY, Machin D, Chan SP, Leong KH, Feng PH, et al. A community-based study of scaling assumptions and construct validity of the English (UK) and Chinese (HK) SF-36 in Singapore. Qual Life Res. 2001;10:175–88.
Thumboo J, Chan SP, Machin D, Soh CH, Feng PH, Boey ML, et al. Measuring health-related quality of life in Singapore: normal values for the English and Chinese SF-36 Health Survey. Ann Acad Med Singapore. 2002;31:366–74.
Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000;108:609–13.
Beddhu S, Zeidel ML, Saul M, Seddon P, Samore MH, Stoddard GJ, et al. The effects of comorbid conditions on the peritoneal dialysis. Am J Med. 2002;112:696–701.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92.
Farivar SS, Liu H, Hays RD. Half standard deviation estimate of the minimally important difference in HRQOL scores? Expert Rev Pharmacoeconomics Outcomes Res. 2004;4:515–23.
Griva K, Lai AY, Lim HA, Yu Z, Foo MWY, Newman SP. Non-adherence in patients on peritoneal dialysis: a systematic review. Cameron DW, editor. PLoS One. 2014;9, e89001.
Ashby M, op’t Hoog C, Kellehear A, Kerr PG, Brooks D, Nicholls K. Renal dialysis abatement: lessons from a social study. Palliat Med. 2005;19:389–96.
Bilgic A, Akman B, Sezer S, Ozisik L, Arat Z, Ozdemir FN, et al. Predictors for quality of life in continuous ambulatory peritoneal dialysis patients. Nephrology. 2008;13:587–92.
Chiu Y-W, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol. 2009;4:1089–96.
Andrykowski MA, Hunt JW. Positive psychosocial adjustment in potential bone marrow transplant recipients: cancer as a psychosocial transition. Psychooncology. 1993;2:261–76.
Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol. 1983;38:1161–73.
Dimkovic N, Oreopoulos DG. Assisted peritoneal dialysis as a method of choice for elderly with end-stage renal disease. Int Urol Nephrol. 2008;40:1143–50.
Walker DR, Chen L, Bhattacharyya SK. The impact of higher peritoneal dialysis utilization on Singapore’s government expenditures. Hiroshima, Japan: Third Asian Chapter Meet. Int. Soc. Perit. Dial; 2007.
Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291:697–703.
Young GJ, Meterko M, Desai KR. Patient satisfaction with hospital care: effects of demographic and institutional characteristics. Med Care. 2000;38:325–34.
Finkelstein FO, Sorkin M, Cramton CW, Nolph K. Initiatives in peritoneal dialysis: where do we go from here? Perit Dial Int. 1991;11:274–8.
Tsai T-C, Liu S-I, Tsai J-D, Chou L-H. Psychosocial effects on caregivers for children on chronic peritoneal dialysis. Kidney Int. 2006;70:1983–7.
Moore R, Teitelbaum I. Preventing burnout in peritoneal dialysis patients. Adv Perit Dial. 2009;25:92–5.
Acknowledgments
The authors would like to express their sincere gratitude to the participants of this study, as well as the various study team members and renal healthcare professionals who have assisted with and supported the study. This research was supported by grants from the Singapore National Kidney Foundation Research Fund (NKFRC2008/07/24) and Singapore Ministry of Education–National University of Singapore Academic Research Fund (Start-Up; FY2007-FRC5-006) to K.G., both of which we gratefully acknowledge. Study sponsors had no role in study design, data collection, analyses, or interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Authors’ Contributions
KG and MWYF were responsible for the research idea and study design. YZ and AWCK were involved in the data acquisition. HAL and KG participated in data analyses/interpretation. HAL was responsible in statistical analyses. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. KG takes responsibility that this study has been reported honestly, accurately, and transparently; that no important aspects of the study have been omitted; and that discrepancies from the study as planned (and, if relevant, registered) have been explained.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lim, H.A., Yu, Z., Kang, A.W.C. et al. The Course of Quality of Life in Patients on Peritoneal Dialysis: A 12-month Prospective Observational Cohort Study. Int.J. Behav. Med. 23, 507–514 (2016). https://doi.org/10.1007/s12529-015-9521-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-015-9521-z