Abstract
Purpose
Associations of behaviorally modifiable factors like physical activity (PA), sedentary behaviors, and sleep with cardiovascular diseases (CVDs) are complicated. We examined whether membership in latent classes (LCs) differentiated by PA and sleep profiles (real-life clustering of behaviors in population subgroups) associate with metabolic risk factors and CVD risk.
Methods
The National FINRISK 2012 Study comprise a cross-sectional sample of 10,000 Finns aged 25 to 74 years. Analyses included participants with complete data on a health questionnaire, a health examination, who had no prevalent CVD (n = 4031). LCs with PA and sleep profiles were previously defined using latent class analysis. Ten metabolic risk factors and the Framingham 10-year CVD risk score were compared between the LCs.
Results
PA and sleep class profiles were substantially similar for genders. Compared to LC-1, with a profile including high PA and sufficient sleep, membership in LC-4, with a profile including sedentariness and insufficient sleep was associated with high metabolic risk factors in women but not in men. In women, also membership in LC-2, with a profile including light PA, sufficient sleep, and high sedentariness was associated with high metabolic risk factors. The Framingham 10-year CVD risk score was highest in LCs 2 and 4 in both genders.
Conclusions
Membership in LCs differentiated by PA and sleep profiles was associated with metabolic risk factors merely in women, suggesting gender differences in the interrelationships of health behaviors and metabolic risk factors. Total CVD risk differed between the LCs despite of gender; however, the effect was small.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physical activity (PA) decreases the risk of cardiovascular diseases (CVDs) [1] and is protective against metabolic risk factors [2]. Scientific evidence also suggests sleep and sedentary time as potentially modifiable risk factors for CVD. To some extent, it seems that sufficient sleep of good quality and PA have a synergistic positive effect, while sedentary behaviors have a contrasting effect on metabolic risk factors [3]. Sleep duration alone shows a U-shaped association with CVD mortality and morbidity and metabolic consequences [4–6] while prolonged sedentary behaviors, most often sitting, show direct associations with impaired cardiovascular health [7–9].
The prediction of multiple health-related outcomes has been improved by including also sleep duration into a lifestyle risk index with PA, alcohol use, diet, and smoking [10]. Indeed, a combination of low PA and short sleep duration, compared to high PA and mid-range sleep duration, increased the risk of insulin resistance in healthy adults [11] and the risk of metabolic syndrome and inflammation in adolescents [12]. In adult Americans, those who reported frequent insufficient sleep were more likely to have a poorer general health, activity limitations, depressive symptoms, and to be physically inactive than those with sufficient sleep [13]. It is suggested that the U-shaped association between sleep duration and health may result from different underlying correlates such as PA [14, 15]. Very recently, it was observed in two different studies [16, 17] that short sleep duration was associated with increased CVD mortality independently of PA level, with the other study confirming that long sleep duration was detrimental only among those with a low PA level [17]. Xiao et al. [16] also observed that an increasing number of unhealthy behaviors, i.e., short sleep, low moderate-to-vigorous PA, high television viewing time, and elevated body mass index (BMI), associated with greater CVD mortality risk.
Often, associations between behavioral risk factors and health are studied by variable-oriented methods, i.e., formulating statements in terms of variables. This kind of approach focuses on the relationship between variables leaving interindividual differences without attention, i.e., assuming them to be random [18]. A person-oriented method does not focus on the variables but on the individuals or homogenous subgroups of individuals in the population, assuming their uniqueness and person-specific behaviors [18, 19]. So far, it has also been more common to study multiple health behaviors by co-occurrence than by clustering methods [20]. To understand the less studied clustering, we modeled and already published the interrelationships between PA and sleep in the adult population in Finland, using a person-oriented, clustering method, the latent class analysis (LCA) [21]. We found four latent classes (LCs) based on PA and sleep behavior patterns (referred hereby as “class profiles”). The most prevalent LC (LC-1) had a profile characterized by high levels of leisure time PA, low leisure time sitting, and self-rated sufficient sleep around 7 to 8 h per night. The least prevalent LC (LC-4) had a profile characterized by self-rated poor sleep of less than 6 h, no leisure time PA, and high sitting time [21].
The prevalence of ideal cardiovascular health, as defined by the American Heart Association, is low in Finland (8.8 % in women and 3 % in men), exposing the need for further reducing the CVD burden at a population level [22]. Therefore, it is important to study how different behavioral population subgroups are related to cardiovascular health and to implement strategies that improve the situation. We studied how membership in the four LCs with different PA and sleep profiles is associated with metabolic risk factors and total CVD risk in adults in Finland.
Methods
Participants
Data comprised the National FINRISK 2012 Study in Finland. A cross-sectional stratified random sample of 10,000 adults, aged 25 to 74 years, were sent a health questionnaire and invited to a health examination. The participation rate was 64.9 % (n = 6424). The final analytical sample included those (n = 5858) without prevalent CVD diagnosis or treatment (including myocardial infarction, stroke, bypass surgery, angioplasty, angina pectoris, and heart failure), who also underwent the health examination (n = 4905), and were without acute infection and had information on all dependents and important covariates (n = 4031). The FINRISK study protocol that is described elsewhere [23] has been repeated in 5-year intervals since 1972. The study closely follows the WHO MONICA protocol [24] and the later recommendations of the European Health Risk Monitoring Project [25]. The coordinating ethics committee of Helsinki and Uusimaa hospital district gave their approval for the study protocol. All participants gave their written, informed consent.
CVD Risk Factors
At the health examination site, a trained nurse measured height, weight, waist circumference, and blood pressure. Blood pressure was measured three times, using mercury sphygmomanometers, from the right upper arm while the participant was in a seated position, and the average of the second and third measurements was computed. Height was measured to the nearest 0.1 cm. Weight was measured in light clothing to the nearest 100 g with a beam balance scale. Waist circumference was measured at the midpoint of the lowest rib and iliac crest. A blood draw was taken and analyzed in the laboratory of the National Institute for Health and Welfare, (Helsinki, Finland) using standardized, validated methods. Serum total cholesterol, high-density lipoprotein cholesterol (HDL-cholesterol), and triglycerides were analyzed using enzymatic methods (Abbott Laboratories, Abbott Park, Illinois, USA). Low-density lipoprotein cholesterol (LDL-cholesterol) was calculated using the Friedewald algorithm [26]. High-sensitivity C-reactive protein (CRP) and glycated hemoglobin A1c (HBA1C) were determined by immunoturbidimetrics (Abbott Laboratories, Abbott Park, Illinois, USA).
All continuous risk factors were dichotomized into low (within recommendations) and high (above recommended levels) according to the national and international guidelines [27–31]. Total cholesterol was coded as high if total cholesterol ≥5 mmol/l or if the participant was taking cholesterol-lowering medication. HDL-cholesterol for men was coded as high if HDL-cholesterol ≥1.00 mmol/l and for women if HDL-cholesterol ≥1.20 mmol/l. LDL-cholesterol was coded as high if LDL-cholesterol ≥3.00 mmol/l or if the participant was using cholesterol-lowering medication. Triglycerides were coded as high if triglycerides were ≥1.70 mmol/l or if the participant was using lipid medication. Total cholesterol/ HDL-cholesterol ratio was coded as high if it was >5.00 for men and >4.18 for women. CRP was coded as high if CRP was between 3.00 and 10.00 mg/l. Those with a CRP ≥10.00 mg/l were excluded from analyses as having an acute infection. HBA1C % was dichotomized as high when HBA1C % >6.00 % or if the participant had been diagnosed with diabetes.
BMI was calculated as weight in kilograms divided by squared height in meters and was coded as high, if BMI ≥30 kg/m2. Waist circumference was coded as high for men if ≥102 cm and for women if ≥89 cm. High blood pressure was determined as systolic blood pressure ≥140 mmHg or as diastolic blood pressure ≥90 mmHg or if the participant was taking blood pressure medication.
The total CVD risk was assessed by calculating a Framingham 10-year CVD risk score, according to D’Agostino et al. [32]. The Framingham risk score is a sex-specific index, estimating percentage risk of CVD within the next 10 years, based on age, the levels of total cholesterol, HDL-cholesterol, and systolic blood pressure, use of blood pressure medication, diabetes, and smoking.
Covariates
All information on employment status, education, smoking, alcohol consumption, and diabetes, medication for cholesterol, blood pressure and diabetes, and menopausal status for women was assessed by the questionnaire. Employment was coded as employed or not employed with the latter including all retired, unemployed, and homemakers irrespective of their reason for unemployment. Education in years was divided into thirds by birth cohort. Smoking was categorized as non-smoking, former smoker ≤6 months, former smoker >6 months, and smoking. A person was considered to use cholesterol-lowering medication if they reported using medication according to a doctor’s order. Blood pressure medication was considered used if the person reported use within the past week. A person was considered diabetic if they had either a doctor’s diagnosis of diabetes or reported the use of diabetes medication. Alcohol consumption was assessed as portions of alcohol beverages consumed during the past week and was further transformed into grams of alcohol per kilogram of weight. Menopausal status of women was coded as those with normal menstruation, those who were postmenopausal with hormone replacement therapy, and those who were postmenopausal without hormone replacement therapy. Postmenopausal was defined as having no regular menstruation within the last 12 months.
Statistical Analyses
Previously, we defined four LCs and their class profiles in this sample using LCA [21]. Indicator variables for the LCA included employment status (working, not working), leisure time PA (inactive, light, moderate-to-high), occupational PA (inactive, light, moderate-to-high), commuting PA (inactive, light, moderate-to-high), screen time, i.e., time spent sitting in front of a television or computer screen in leisure time (lowest third, mid-third, highest third), napping (0, ≤0.5, >0.5 h), sleep sufficiency (no, yes), weekend-weekday difference in time in bed (≤0.5, >0.5 h), sleep duration (<6, 6–6.9, 7–7.9, 8–9, >9 h), use of sleep drugs (no, yes), and chronotype (morning type, more morning-than-evening type, more evening-than-morning type, evening type). A more detailed description of the variables in LCA is given in a supplementary table. In the present study, gender-specific associations of class membership with metabolic risk factors were determined using weighted logistic regression models (IBM SPSS statistics v.22), with posterior probabilities of class membership as weights to get more accurate estimates between the LCs and metabolic risk factors. The most prevalent LC, LC-1 (45 % in men, 47 % in women) was chosen as the reference category in both genders. Models were adjusted for age, educational level, alcohol consumption, smoking, and menopausal status in women. The Framingham 10-year CVD risk score levels were compared between LCs by weighted analysis of covariance using Bonferroni adjustment for multiple comparisons, adjusting for age, education level, alcohol consumption, smoking, BMI, and menopausal status in women. BMI was not adjusted for in the logistic models since BMI was one outcome in these models. Significance level was set at p < 0.05.
Results
The main characteristics of the class profiles were similar between genders, including employment status, leisure time PA, and sleep sufficiency, but also, some gender differences in the profiles were found. The characteristics of all class profiles are shown in Table 1. Generally, high probabilities for working, high leisure time PA, and self-reported sufficient sleep describe the LC-1 profile. Not working, light leisure time PA, sufficient sleep, and high screen time describe the LC-2 profile, and working, moderate-to-high occupational PA, insufficient sleep, and over 30 min weekend-weekday difference in time in bed describe the LC-3 profile. The LC-4 profile is described by no leisure time PA, high screen time, and insufficient sleep. A more detailed explanation of the class profiles is given elsewhere [21].
Background characteristics of all initially CVD-free participants are given by LCs in Tables 2 and 3. In men, the LCs differed significantly in age, educational years, alcohol consumption, and smoking but not in weight. In women, the LCs differed significantly in age, educational years, weight, alcohol consumption, and menopausal status but not in smoking.
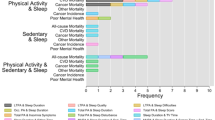
In the crude logistic regression models in men, compared to membership in LC-1, membership in LC-2 and in LC-4 was associated with an increased risk of high blood pressure, high triglycerides, high HBA1C, high BMI, and a large waist circumference (Table 4). Membership in LC-2 was also significantly associated with an increased risk of high total cholesterol and high LDL-cholesterol. When adjusting for age, smoking, alcohol consumption, and education, only the risk of high HBA1C in LC-4 (odds ratio (OR) = 2.17, 95 % confidence intervals (CI) = 1.09–4.35) compared to LC-1 remained statistically significant.
In women, when compared to membership in LC-1, membership in LC-2 and in LC-4 was significantly associated with an increased risk of high total cholesterol, high blood pressure, high LDL-cholesterol, high total cholesterol/HDL-cholesterol ratio, high triglycerides, high HBA1C, high BMI, and large waist circumference (Table 5). Membership in LC-4 was also significantly associated with an increased risk of high CRP and low HDL-cholesterol levels. In the fully adjusted models, membership in LC-2 remained significantly associated with a risk of high total cholesterol (OR = 1.67, 95 % CI = 1.22–2.30), high LDL-cholesterol (OR = 1.46, 95 % CI = 1.10–1.94), and high triglycerides (OR = 1.39, 95 % CI = 1.04–1.88). Also, membership in LC-4 remained significantly associated with a risk of elevated blood pressure (OR = 1.49, 95 % CI = 1.06–2.10), low HDL-cholesterol (OR = 0.57, 95 % CI = 0.36–0.90), high triglycerides (OR = 1.48, 95 % CI = 1.03–2.12), high HBA1C (OR = 2.21, 95 % CI = 1.22–3.99), high CRP levels (OR = 1.82, 95 % CI = 1.28–2.58), high BMI (OR = 1.49, 95 % CI = 1.05–2.10), and large waist circumference (OR = 1.56, 95 % CI = 1.14–2.13).
Comparisons of the Framingham 10-year CVD risk score between the LCs in men revealed statistically significant differences (Table 6). LC-1 and LC-3 had a significantly lower risk score than both LC-2 and LC-4 (F = 289.65, df = 3, p < .001, η 2 = 0.332). These differences remained in the fully adjusted models, with the highest risk score found in LC-4 (F = 23.79, df = 3, p < .001, η 2 = 0.039). In women, the Framingham 10-year CVD risk score was significantly highest in LC-2, differing from all other LCs in the crude (F = 271.48, df = 3, p < .001, η 2 = 0.265) and the fully adjusted model (F = 37.64, df = 3, p < .001, η 2 = 0.048) (Table 6). The risk score in LC-4 also was significantly higher than the risk score in LC-1 and LC-3 throughout the models. After adjusting for confounding variables, the Framingham risk scores were consistently lower in women than in men.
Discussion
Membership of LCs (differentiated by PA and sleep profiles reflecting real-life combinations of PA and sleep behaviors) was associated with metabolic CVD risk factors in women but practically not in men. Differences in the Framingham 10-year CVD risk score between the LCs were found in both genders, but the effect sizes were small. This indicates that among the CVD healthy adult population, the sleep and PA-based LC clustering provided little new ability to identify persons at risk for future CVD when other pertinent risk factors were accounted for. In women, membership in the inactive and poorly sleeping LC-4 was associated with a risk of hypertension, low HDL-cholesterol, high triglycerides, high HBA1C, high CRP, high BMI, and large waist circumference when compared to membership in the high active, sufficiently sleeping LC-1. However, in men membership in LC-4 was associated only with increased risk of high HBA1C. Furthermore, in women, membership in the lightly active, sufficiently sleeping LC-2 was associated with an increased risk of high total cholesterol, high LDL-cholesterol, and high triglycerides. The Framingham 10-year CVD risk score was significantly lower in the LC-1 and LC-3 than in the LC-2 and LC-4 in both genders. In men, the Framingham risk score was highest for members of LC-4 (significantly different from LC-1 and LC-3) and in women for members of LC-2 (significantly different from all other LCs).
The gender differences observed in our study suggest that real-life combinations of behaviors occur differently and are differently associated with heart health between genders. The estimated prevalence of LC-4, described by inactivity and poor sleep, was 11 % in women vs. 5 % in men. It is known that adherence to [33] and patterns of health behaviors vary between men and women [34]. In a large, nationally representative sample of US adults [34], women were more likely than men to adhere to recommendations concerning alcohol use and smoking but less likely to adhere to exercise recommendations. In Finland, women have a higher prevalence of ideal cardiovascular health, defined as an optimal level in seven cardiovascular metrics, with only the prevalence of optimal PA level being higher in men [22]. In our study, adjustment for smoking and alcohol use attenuated the associations between LCs and metabolic risk factors in men, indicating that these traditional risk factors account for most of the differences in metabolic risk factors. Sleep duration and causes of mortality may be differently associated between genders in Finland, with a U-shaped association between sleep duration and total mortality in both genders but associations to CVD mortality only in women [35]. Similar findings exist elsewhere [36, 37], even though many studies report associations between sleep duration and CVD mortality independent of gender [4, 17, 38]. Gender differences have earlier been reported in Finland also in the association between sleep duration and type 2 diabetes [39] and between leisure time PA, commuting PA, and CRP levels [40]. Thus, it seems that even if the general risk of CVD is higher in men than in women, the variance in metabolic CVD risk factors is not explained by combinations of PA and sleep in Finnish men.
In both genders, the total CVD risk, assessed by the Framingham 10-year CVD risk score, was high in LC-4 but somewhat unexpectedly it was also higher in LC-2 than in LC-3. Short and insufficient sleep [6] and low leisure time PA [1] increase CVD risk, and thus, we had assumed that the LC-3 and LC-4 would associate with a higher CVD risk among the LCs. The common characteristics of the class profiles 2 and 4 were not working and likelihood of high screen time. Screen time was used here as a measure of sedentary leisure time that is suggested to increase CVD morbidity risk independently of PA levels [41]. In a large US cohort, higher CVD mortality was observed in short sleepers with less than 1 h/week intense PA or more than 3 h/day television viewing [16]. We speculate that a lower CVD risk in LC-3 than in LC-2 and LC-4 is partly due to the lower probability of high screen time but also the probability of high occupational and thus total PA in this LC. Benefits of occupational or commuting PA for CVD risk are not as evident as those of leisure time PA [1], but their role in total level of PA are important. Based upon our findings, being active at work and not spending too much time in screen-based entertainments may bear beneficial effects upon heart health on a population level.
Most of our non-working individuals were retired and consequently of older age. Age increases the likelihood of membership in LC-2 and LC-4, likely explaining some of the findings of total CVD risk between the LCs. The Framingham risk score itself increases with higher age. For example, being a 40-year-old woman results in 4 points on the scale which equals having a non-treated systolic blood pressure level of 150–159 mmHg. Being a 40-year-old man results in 5 points, which is more than is given for any other risk factor except a treated systolic blood pressure of over 160 mmHg [32]. Age also moderates PA and sleep behaviors. With increasing age, average sleep duration may decrease or increase [42], the weekend-weekday discrepancy in sleep duration may diminish [43], and sleep complaints increase [44]. Higher age also relate to less conditioning PA [45] and more television viewing time [46]. The age structure of the population in Finland is getting older, and therefore, it is important to acknowledge risky health behaviors also in older persons.
Household activities that are often reported as leisure time PA do not relate with metabolic CVD risk factors [47], suggesting that PA intensity matter when aiming to reduce CVD risk. An intervention study in elderly participants showed that aerobic exercise three times per week improved both sleep quality and metabolic functioning in the participants [48]. Buman et al. [3] studied how reallocation of time between sleep, sedentary behaviors, light PA, and moderate-to-high intensity PA influences different cardiovascular biomarkers. They found that the most beneficial effects upon waist circumference, HDL-cholesterol, triglycerides, and insulin sensitivity were achieved when increasing time in moderate-to-vigorous intensity PA, with additional benefit from light-intensity PA and sleep duration when reallocated from sedentary time. Thus, there is reason to argue that maybe the PA intensity for members in LC-2 is insufficient to gain stronger health benefits of PA.
Socioeconomic and sociodemographic factors affect patterns of adherence and non-adherence to health behaviors [34, 49, 50]. In the LC profiles, being not employed occurred together with probability of high leisure screen time and short sleep that furthermore was related to higher CVD risk, particularly in LC-4. It is noteworthy, that being not employed refers to all not-working persons irrespective the reasons. The estimated prevalence of retired was highest in LC-2s and of unemployed for other reasons in LC-4s, particularly in men (results not shown). The reason for being not employed can be one moderator of the results in this study, but we cannot conclude on causality. Unemployment shows, e.g., a U-shaped association with sleep duration [51, 52] while also retirement, disability retirement, and unemployment for other reasons, all have a positive relationship with long sleep duration [52] that as such can be a sign of chronic comorbidity particularly of non-cardiovascular causes [15]. While the probability of being a long sleeper (>9 h) in our LCs was, in absolute figures, so low (0.002–0.077 across LCs) that it was not a distinguishing characteristic of any of the class profiles, it should be noted that in class profile of LC-2, the likelihood of long sleep was 20-fold higher in men and 7.9-fold higher in women than in class profile of LC-3, and in women, the highest likelihood of long sleep (0.077) was found in LC-4 [21]. Consequently, although long sleep did not distinguish the class profiles from each other, it was most likely for members of LC-4. It has been suggested that PA behavior may be modifying the associations of self-reported short or long sleep duration and CVD risk [14, 17, 53, 54]. Our findings seem to support this idea and suggest that socioeconomic status, here employment, is an important feature for the clustering of health risk.
The women in LC-4 represent a high-risk group as regards both behavioral and metabolic perspective. Others have reported that short sleep and sleep insufficiency are related to increased risk of diabetes [5, 55, 56], risk of high BMI, obesity [57], and higher abdominal obesity, independently of PA [58]. In addition, low leisure time PA has been related to impaired glucose metabolism [59] and increased insulin resistance across different sleep durations [11]. In postmenopausal women, high leisure time PA despite poor sleep was associated with lower BMI, waist circumference, trunk fat, total body fat, insulin levels, and higher glucose levels compared to less active women with good sleep quality [60]. The role of chronotype for CVD risk is not fully established, but in a recent Finnish study [61], it was observed that evening types compared to morning types have higher odds for type 2 diabetes, low total cholesterol and LDL-cholesterol, and systolic blood pressure. Evening chronotype in combination with short sleep and physical inactivity is maybe a factor that further can explain some of the more pronounced associations found in LC-4 in women than in men, lending support to the idea that unfavorable health outcomes such as obesity, diabetes, and hypertension depend on the dysregulation of our circadian and metabolic systems resulting from an imbalance between our lifestyle and inherent behaviors [62].
Strengths and Limitations
Information about PA and sleep, as well as covariates, was self-reported, thus making the data vulnerable to reporting bias. Because of the cross-sectional setting, conclusions about causality cannot be drawn. However, the participants were free of an earlier CVD history, diminishing the possibility of reverse causation. Due to missing data, 17.8 % of the possible participants without prevalent CVD were excluded, which may further have affected the statistical power of the analyses but also weaken the generalizability of the results to CVD healthy adult population. The men’s LC-4 had less than a hundred subjects, which may explain the lack of statistically significant associations. We compared the final sample to the excluded, initially CVD-free participants and found that there were more women (56.4 vs. 50.0 %), older (mean age 51.1 vs. 47.7 years), more physically active (32.3 vs. 27.4 % medium to high active), and more 7–7.9 h sleepers (38.0 vs. 34.9 %) than in the excluded. However, if our sample was somewhat healthier than the excluded, this would only mean that our results would have been enforced by having a larger sample. We decided to include medication use in our outcome variables in logistic models. However, we also ran models for continuous risk factors, adjusting the analyses for medication use and observed that both analytical approaches yielded similar interpretation: LCs were associated with most CVD risk factors among women, but very little evidence was found among men. The few discrepancies between logistic and ANCOVA models were probably due to the use of the medication variable, but different results can also be due to the fact that ANCOVA tests the differences between all groups while logistic regression model uses one reference group. Acetylsalicylic acid was not controlled for as a medication because the effects of acetylsalicylic acid in CVD prevention are debated [31] and we assumed it to be used for other purposes than CVD among our CVD-free participants. BMI was controlled for in the Framingham risk score models but not in regression models because BMI was one outcome here. We reasoned not to include BMI as a covariate in our logistic models because we cannot conclude on which comes first, obesity or physical inactivity and poor sleep. Looking at the total CVD risk, taken together with information on several biomarkers, BMI is an important confounder since it is a part of the total risk of the person and not included in the Framingham risk score automatically.
Conclusions
Membership in PA and sleep profiles, reflecting real-life combinations of PA and sleep behaviors, is associated with CVD risk factors more conclusively in women than in men, even if the effect size is small, indicating little new information in addition to more traditional risk factors such as age, alcohol, and smoking. However, small statistically independent associations between real-life combinations of PA and sleep factors with CVD risk factors among CVD healthy population are worth considering for. Based on our findings, among CVD healthy adult population, about 11 % of women and 5 % of men belong to the group characterized by physical inactivity and poor sleep that especially in women also show a slightly higher independent risk for future CVD than the physically active and good sleeping.
References
Li J, Siegrist J. Physical activity and risk of cardiovascular disease—a meta-analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9(2):391–407. doi:10.3390/ijerph9020391.
Glazer NL, Lyass A, Esliger DW, Blease SJ, Freedson PS, Massaro JM, et al. Sustained and shorter bouts of physical activity are related to cardiovascular health. Med Sci Sports Exerc. 2012. doi:10.1249/MSS.0b013e31826beae5.
Buman MP, Winkler EA, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179(3):323–34. doi:10.1093/aje/kwt292.
Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–92. doi:10.1093/eurheartj/ehr007.
Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24(5):731–43. doi:10.1016/j.beem.2010.07.001.
Luyster FS, Strollo Jr PJ, Zee PC, Walsh JK. Boards of directors of the American academy of sleep medicine and the sleep research society. Sleep: a health imperative. Sleep. 2012;35(6):727–34. doi:10.5665/sleep.1846.
Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41(5):1338–53. doi:10.1093/ije/dys078.
Chomistek AK, Manson JE, Stefanick ML, Lu B, Sands-Lincoln M, Going SB, et al. Clinical research: relationship of sedentary behavior and physical activity to incident cardiovascular disease. Results from the women's health initiative. J Am Coll Cardiol. 2013;61:2346–54. doi:10.1016/j.jacc.2013.03.031.
Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35(6):725–40. doi:10.1139/H10-079.
Ding D, Rogers K, Macniven R, Kamalesh V, Kritharides L, Chalmers J, et al. Revisiting lifestyle risk index assessment in a large Australian sample: should sedentary behavior and sleep be included as additional risk factors? Prev Med. 2014;60:102–6. doi:10.1016/j.ypmed.2013.12.021.
Zuo H, Shi Z, Yuan B, Dai Y, Hu G, Wu G, et al. Interaction between physical activity and sleep duration in relation to insulin resistance among non-diabetic Chinese adults. BMC Public Health. 2012;12:247. doi:10.1186/1471-2458-12-247.
Countryman A, Saab P, Llabre M, Penedo F, McCalla J, Schneiderman N. Cardiometabolic risk in adolescents: associations with physical activity, fitness, and sleep. Ann Behav Med. 2013;45(1):121–31. doi:10.1007/s12160-012-9428-8.
Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6(1):23–7. doi:10.1016/j.sleep.2004.06.003.
Knutson KL, Turek FW. The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep. 2006;29(7):878–9.
Stranges S, Dorn JM, Shipley MJ, Kandala NB, Trevisan M, Miller MA, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168(12):1353–64. doi:10.1093/aje/kwn337.
Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. 2014;180(10):997–1006. doi:10.1093/aje/kwu222.
Bellavia A, Akerstedt T, Bottai M, Wolk A, Orsini N. Sleep duration and survival percentiles across categories of physical activity. Am J Epidemiol. 2014;179(4):484–91. doi:10.1093/aje/kwt280.
Bogat GA, Levendosky AA, von Eye A. The future of research on intimate partner violence: person-oriented and variable-oriented perspectives. Am J Community Psychol. 2005;36(1–2):49–70. doi:10.1007/s10464-005-6232-7.
Collins LM, Lanza ST. Latent class and latent transition analysis. With applications in the social, behavioral, and health sciences. Hoboken: Wiley Series in Probability and Statistics; 2010.
McAloney K, Graham H, Law C, Platt L. A scoping review of statistical approaches to the analysis of multiple health-related behaviours. Prev Med. 2013;56(6):365–71. doi:10.1016/j.ypmed.2013.03.002.
Wennman H, Kronholm E, Partonen T, Tolvanen A, Peltonen M, Vasankari T, et al. Physical activity and sleep profiles in Finnish men and women. BMC Public Health. 2014;14:82. doi:10.1186/1471-2458-14-82.
Peltonen M, Laatikainen T, Borodulin K, Wikström K, Jousilahti P, Jula A, et al. Prevalence of ideal cardiovascular health in an adult Finnish population: the national FINRISK 2007 study. Int Heart Vasc Dis J. 2014;2(3):3.
Borodulin K, Vartiainen E, Peltonen M, Juolevi A, Laatikainen T, Männistö S, et al. 40-year trends in cardiovascular risk factors in Finland. Eur J Public Health. 2014. doi:10.1093/eurpub/cku174.
World Health Organization. The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41(2):105–14.
Tolonen H, Kuulasmaa K, Laatikainen T, Wolf H, EHRM. European Health Risk Monitoring Project. Recommendation for indicators, international collaboration, protocol and manual of operations for chronic disease risk factor surveys. 2002; Helsinki, Finland.
Bachorik PS, Ross JW. National Cholesterol Education Program recommendations for measurement of low-density lipoprotein cholesterol: executive summary. The National Cholesterol Education Program Working Group on Lipoprotein Measurement. Clin Chem. 1995;41(10):1414–20.
Working group set up by the Finnish Medical Society Duodecim and the Finnish Respiratory Society. Diabetes. Current Care guideline (online). 2007; www.kaypahoito.fi. Accessed 28 Dec 2013.
Working group set up by the Finnish Medical Society Duodecim and the Finnish Respiratory Society. Dyslipidaemias. Current Care guideline (online). 2004; www.kaypahoito.fi. Accessed 28 Dec 2013.
Working group set up by the Finnish Medical Society Duodecim and the Finnish Respiratory Society. Obesity (adult). Current Care Guideline (online). 2002; www.kaypahoito.fi. Accessed 28 Dec 2013.
Working group set up by the Finnish Medical Society Duodecim and the Finnish Respiratory Society. Hypertension. Current Care Guideline (online). 2001; www.kaypahoito.fi. Accessed 28 Dec 2013.
World Health Organization. Prevention of cardiovascular disease: guidelines for assessment and management of total cardiovascular risk. 2007; Geneva, Switzerland.
D'Agostino RBS, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–53. doi:10.1161/CIRCULATIONAHA.107.699579.
Poortinga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Prev Med. 2007;44(2):124–8.
Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Prev Med. 2003;36(5):615–23. doi:10.1016/S0091-7435(02)00067-1.
Kronholm E, Laatikainen T, Peltonen M, Sippola R, Partonen T. Self-reported sleep duration, all-cause mortality, cardiovascular mortality and morbidity in Finland. Sleep Med. 2011;12(3):215–21. doi:10.1016/j.sleep.2010.07.021.
Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30(9):1121–7.
Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y, et al. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14(4):124–8.
Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33(8):1037–42.
Tuomilehto H, Peltonen M, Partinen M, Lavigne G, Eriksson JG, Herder C, et al. Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: the Finnish Diabetes Prevention Study. Diabetes Care. 2009;32(11):1965–71. doi:10.2337/dc08-1980.
Borodulin K, Laatikainen T, Salomaa V, Jousilahti P. Associations of leisure time physical activity, self-rated physical fitness, and estimated aerobic fitness with serum C-reactive protein among 3,803 adults. Atherosclerosis. 2006;185(2):381–7. doi:10.1016/j.atherosclerosis.2005.06.015.
Grøntved A, Ried-Larsen M, Møller NC, Kristensen PL, Wedderkopp N, Froberg K, et al. Youth screen-time behaviour is associated with cardiovascular risk in young adulthood: the European Youth Heart Study. Eur J Prev Cardiol. 2014;21(1):49–56. doi:10.1177/2047487312454760.
Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–66.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–43. doi:10.1016/j.cub.2012.03.038.
Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic-study of 3 communities. Sleep. 1995;18(6):425–32.
Borodulin K, Laatikainen T, Lahti-Koski M, Jousilahti P, Lakka TA. Association of age and education with different types of leisure-time physical activity among 4437 Finnish adults. J Phys Act Health. 2008;5(2):242–51.
Rhodes RE, Mark RS, Temmel CP. Review and special article: adult sedentary behavior: a systematic review. Am J Prev Med. 2012;42:3–e28. doi:10.1016/j.amepre.2011.10.020.
Stamatakis E, Hillsdon M, Primatesta P. Domestic physical activity in relationship to multiple CVD risk factors. Am J Prev Med. 2007;32(4):320–7. doi:10.1016/j.amepre.2006.12.020.
Lira F, Pimentel GD, Santos RV, Oyama LM, Damaso AR, Oller do Nascimento CM, et al. Exercise training improves sleep pattern and metabolic profile in elderly people in a time-dependent manner. Lipids Health Dis. 2011;10:1–6. doi:10.1186/1476-511X-10-113.
Griffin B, Sherman KA, Jones M, Bayl-Smith P. The clustering of health behaviours in older australians and its association with physical and psychological status, and sociodemographic indicators. Ann Behav Med. 2014. doi:10.1007/s12160-014-9589-8.
Borodulin K, Zimmer C, Sippola R, Makinen TE, Laatikainen T, Prattala R. Health behaviours as mediating pathways between socioeconomic position and body mass index. Int J Behav Med. 2012;19(1):14–22. doi:10.1007/s12529-010-9138-1.
Park S, Cho MJ, Chang SM, Bae JN, Jeon HJ, Cho S, et al. Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. J Sleep Res. 2010;19(4):567–77. doi:10.1111/j.1365-2869.2010.00841.x.
Lallukka T, Sares-Jaske L, Kronholm E, Saaksjarvi K, Lundqvist A, Partonen T, et al. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health. 2012;12:565. doi:10.1186/1471-2458-12-565.
Basner M, Fomberstein KM, Razavi FM, Banks S, William JH, Rosa RR, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–95.
Stamatakis KA, Punjabi NM. Long sleep duration: a risk to health or a marker of risk? Sleep Med Rev. 2007;11(5):337–9.
Shankar A, Syamala S, Kalidindi S. Insufficient rest or sleep and its relation to cardiovascular disease, diabetes and obesity in a national, multiethnic sample. PLoS One. 2010;5(11):e14189. doi:10.1371/journal.pone.0014189.
Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi:10.1196/annals.1417.033.
Altman NG, Izci-Balserak B, Schopfer E, Jackson N, Rattanaumpawan P, Gehrman PR, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13(10):1261–70. doi:10.1016/j.sleep.2012.08.005.
Fogelholm M, Kronholm E, Kukkonen-Harjula K, Partonen T, Partinen M, Härmä M. Sleep-related disturbances and physical inactivity are independently associated with obesity in adults. Int J Obes (Lond). 2007;31(11):1713–21.
Borodulin K, Tuomilehto J, Peltonen M, Lakka TA, Sundvall J, Jousilahti P. Association of leisure time physical activity and abdominal obesity with fasting serum insulin and 2-h postchallenge plasma glucose levels. Diabetic Med. 2006;23(9):1025–8. doi:10.1111/j.1464-5491.2006.01897.x.
Casas RS, Pettee Gabriel KK, Kriska AM, Kuller LH, Conroy MB. Association of leisure physical activity and sleep with cardiovascular risk factors in postmenopausal women. Menopause. 2012;19(4):413–9. doi:10.1097/gme.0b013e318230f531.
Merikanto I, Lahti T, Puolijoki H, Vanhala M, Peltonen M, Laatikainen T, et al. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol Int. 2013;30(4):470–7. doi:10.3109/07420528.2012.741171.
Gangwisch JE. Epidemiological evidence for the links between sleep, circadian rhythms and metabolism. Obes Rev. 2009;10 Suppl 2:37–45. doi:10.1111/j.1467-789X.2009.00663.x.
Acknowledgments
Funding for this study was obtained from the Ministry of Education and Culture and the Juho Vainio Foundation, Finland.
Conflict of Interest
Heini Wennman, Erkki Kronholm, Timo Partonen, Asko Tolvanen, Markku Peltonen, Tommi Vasankari, and Katja Borodulin declare that they have no conflict of interest.
Ethical Standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table
(DOC 66 kb)
Rights and permissions
About this article
Cite this article
Wennman, H., Kronholm, E., Partonen, T. et al. Interrelationships of Physical Activity and Sleep with Cardiovascular Risk Factors: a Person-Oriented Approach. Int.J. Behav. Med. 22, 735–747 (2015). https://doi.org/10.1007/s12529-015-9470-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-015-9470-6