Abstract
Background
Coping flexibility refers to one’s ability or skill to effectively modify one’s coping strategy according to the nature of each stressful situation one encounters; the coping flexibility hypothesis (CFH) predicts that more flexible coping will produce more adaptive outcomes.
Purpose
Qur purpose was to test the validity of the CFH in chronic headaches.
Method
The validity of the CFH in chronic pain was tested in female college students who suffered from chronic daily headaches in Japan. Over a period of approximately 3 months, primary participants with chronic headaches (n = 73) and participants with low frequency headaches (n = 123) completed questionnaires related to flexibility in coping and coping with headaches, as well as depressive symptoms later.
Results
A hierarchical multiple regression analysis revealed that flexibility in coping with chronic headaches was significantly associated with reduced depressive symptoms later, even after controlling for the effects of coping strategies with chronic headaches; the CFH for chronic pain was supported by data from chronic headache sufferers. Similar results were also obtained for participants with low frequency headaches. Catastrophizing, a strategy for coping with chronic headaches, was negatively and significantly associated with depressive symptoms later.
Conclusion
The CFH was supported in cases of chronic headache. Our findings indicate the importance of the effects of flexibility in coping with primary headaches on distress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many people are known to suffer from chronic headaches. According to Smitherman et al.’s meta-analysis [1], the prevalence of severe headaches in a 3-month period in four US public health surveillance studies ranged from 16.6 % (according to the National Health Interview Survey) to 22.7 % (based on the National Health and Nutrition Examination Survey). Among 4029 people aged 15 or older in Japan, where our survey was administered, the prevalence of primary headaches categorized as migraines or tension-type headaches in the last year was 30.8 % [2].
Research on chronic pain has emphasized the role of primary headaches as a potential stressor that negatively induces psychological/physical distress [3–5]. Indeed, previous studies have found an association between depressive symptoms and primary headaches, in particular [6, 7]. These studies also revealed that stress responses to primary headaches differ between individuals.
Among the various factors associated with individual differences, coping flexibility has received much attention in pain research [8–17]. Coping flexibility, in general, refers to one’s ability or skill to effectively modify one’s coping strategies according to the nature of each stressful situation one encounters [18]. The transactional theory [19, 20] states that more flexible coping will produce more adaptive outcomes; this supposition is generally referred to as the coping flexibility hypothesis (CFH) [18]. Several frameworks supporting the CFH have also been proposed in chronic disease research [14, 17], and prior investigations on chronic pain [11, 15], rheumatoid arthritis [8, 16], multiple sclerosis [12], breast cancer [13], functional dyspepsia [10], and gastrointestinal cancer [9] have provided support for the CFH. To our knowledge, no study has yet examined the effects of flexibility in coping with primary headaches on psychological/physical distress. However, several studies on coping with headaches [17, 21, 22] have suggested that a number of coping strategies for headaches are associated with distress (including depressive symptoms). Additionally, as mentioned earlier, research on chronic pain has provided frameworks for the CFH and evidence of the hypothesis in incidences of chronic pain. Thus, the CFH may also apply to chronic headaches. In the present study, we tested the validity of the CFH in chronic headaches.
Method
Participants and Procedures
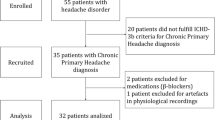
Potential participants described the pain they most frequently suffered during the past year using an open-ended questionnaire. In the questionnaire, pain was defined as pain that occurred at least once or more in a month. Potential participants were recruited from psychology classes across four women’s colleges in Japan and comprised 790 Japanese students in total (mean age 19.3; SD = 1.5). Of the 790 students, 196 (24.8 %; mean age 20.5 years; SD = 1.6; range 18–24) reported headaches as being the most frequent pain they suffered during the last year. There did not include secondary headaches (e.g., headaches arising from menstruation, alcohol/drug consumption, head injuries, or toothaches). These 196 students were participants of the present study. Other types of pain mentioned were menstruation pain (32.2 %), gastralgia (20.0 %), pain from poor circulation or cold fingers and toes (7.1 %), low back pain (6.1 %), and neck and shoulder stiffness (4.7 %).
After providing their informed consent, the 196 participants enrolled in the present study completed questionnaires related to the symptoms and pain frequency of headaches and their coping behaviors. Approximately 3 months after the survey, participants completed a questionnaire related to depressive symptoms. Of the participants we surveyed, 6.1 % noted having received outpatient treatment for headaches, while another 17 % had received outpatient as well as inpatient treatment for headaches. All participants received a pen valued at 100 yen (approximately US $1.25) in exchange for completing each survey.
The participants were subsequently categorized into two groups based on the frequency of their headaches: the chronic daily headache (CH) group and non-chronic headache (NCH) group. To assess headache frequency, participants were asked to rate how frequently they had experienced headaches on a 5-point Likert scale, with 0 = a few times a year, 1 = once a month, 2 = a few times a month, 3 = a few times a week, and 4 = nearly every day. The CH group (N = 73, mean age 20.6 years; SD = 1.7; range 18–24), constituted the primary participants in the present study, were those suffering from chronic daily headaches and who scored a “4” on this question. The NCH group (N = 123, mean age 20.5 years; SD = 1.6; range 18–23) consisted of sufferers of low frequency headaches (not occurring daily), who scored “1” to “3” on this question. None of the participants selected “a few times a year” because chronic pain was defined as occurring at least once a month in this questionnaire.
Measures
All measures, originally written in English, were independently translated into Japanese by three native Japanese psychologists. They were then back-translated into English by a native English psychologist. After the back translation, the original and back-translated questionnaires were compared for discrepancies. Modifications were made to the translated questionnaires after a discussion between the translators. The alpha coefficients of all measures used in this study are given in Table 1.
Coping with Headache
Coping with headache was measured using the Coping Strategies Questionnaire-Revised (CSQ-R) [23], which consists of 27 of the original items from the CSQ [24]. The CSQ was designed to measure coping strategies for chronic pain and is the most frequently used scale to measure stress caused by health-related issues [25]. The CSQ-R consists of six subscales: distraction (five items), catastrophizing (six items), ignoring of pain (five items), distancing from pain (four items), coping self-statements (four items), and praying (three items). Many studies have demonstrated that the CSQ-R has adequate reliability and validity [23, 26, 27]. Each item was rated according to how frequently the strategy is used to cope with headache on a 5-point Likert-type scale, ranging from 0 (never do that) to 4 (always do that), instead of a 7-point Likert scale. This change was made in line with the previous modification [28] because participants were confused by the Likert scale during the pilot testing of the instrument.
Flexibility in Coping with Headache
The Coping Flexibility Scale (CFS) [18], which contains ten items (e.g., I am aware of how successful or unsuccessful my attempts to cope with stress have been. If I have failed to cope with stress, I think of other ways to cope.), was used to measure coping flexibility in chronic headache sufferers. The CFS was designed to measure coping flexibility, which was defined as “the ability to discontinue an ineffective coping strategy and produce and implement an alternative coping strategy” (p. 263) [18]. In a study conducted on Japanese participants [18], the CFS score was positively correlated with all scores on other scales measuring theoretically related constructs and on indicators of improved psychological functioning, such as reduced anxiety, depression, and distress. For Japanese participants, the alpha coefficients of the CFS ranged from 0.83 to 0.90 (M = 0.87); test-retest reliability coefficients over a 6-week period ranged from 0.71 to 0.73 [18]. In this study, the CFS items were slightly modified for measuring flexibility in coping with chronic pain (e.g., stress was replaced with pain). Participants rated the extent to which each item was applicable to them on a 5-point scale ranging from 0 (not applicable) to 4 (highly applicable).
Depressive Symptoms
Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D) [29]. The CES-D is a 20-item self-report scale. The Japanese version of the CES-D has shown adequate reliability and validity in prior research involving a Japanese sample [30]. Each item was rated based on the participants’ experiences within the past week on a 4-point Likert scale, ranging from 0 (not at all) to 3 (very much so). In a study conducted by Wong et al. [31], the mean CES-D score was 29.35 (SD = 15.76) in a sample of 181 Chinese patients with chronic pain. In another study of 32 female US patients with fibromyalgia [32], the mean CES-D score was 26.4 (SD = 11.4). We compared the mean of the CH group in the current study with the means of these two samples of chronic pain sufferers and found no significant differences t(252) = 0.26, p = 0.21, d = 0.175 for Chinese patients and t(103) = 0.07, p = 0.95, d = 0.014 for US patients.
Data Analysis
In order to test the validity of the CFH in chronic headache, a hierarchical multiple regression analysis was conducted for the CH group, with depressive symptom score as the criterion variable. The CSQ-R subscale and CFS scores were entered in steps 1 and 2, respectively. The same analysis was conducted for the NCH group to provide informative data.
Results
The means and standard deviations of all variables for each group are given in Table 1; the zero-order correlations between the variables are shown in the Appendix. To test the CFH, a hierarchical multiple regression analysis was conducted with the depressive symptom score measured for the CH group (see Table 2). The change in R 2 at step 2 indicated that coping flexibility accounted for a significant proportion of the variance in depressive symptoms: ΔR 2 = 0.11, F(1, 65) = 14.69, p < 0.001; effect size, Cohen’s f 2 = 0.12. The result suggests that, beyond coping strategies for chronic headaches, flexibility in coping with chronic headaches incrementally contributes to decreased severity in depressive symptoms later. With regard to each coping strategy, catastrophizing significantly predicted depressive symptoms (β = 0.59, p < 0.001).
A hierarchical multiple regression analysis for the NCH group revealed that the change in R 2 at step 2 was significant: ΔR 2 = 0.06, F(1, 115) = 8.49, p < 0.01; effect size, Cohen’s f 2 = 0.06. Furthermore, catastrophizing was found to significantly predict depressive symptoms (β = 0.23, p < 0.05).
Discussion
Research on chronic pain has emphasized the effects of coping flexibility on the manifestation of psychological symptoms with pain [8–17], and recent studies have reported the effects of training on coping flexibility among chronic disease patients [10, 33]. However, no study has yet examined the effects of flexibility in coping with headaches on psychological/physical distress. Therefore, in the present study, the CFH, which predicts that coping flexibility attenuates the negative impact of headaches on depressive symptoms, was tested in primary headache sufferers. The hierarchical multiple regression analysis revealed that flexibility in coping with chronic headaches was significantly associated with reduced depressive symptoms over a period of approximately 3 months, even after controlling for the effects of coping strategies with chronic headaches. That is, coping flexibility attenuated the negative impact of chronic headaches on depressive symptoms. Thus, the CFH was supported by data from chronic headache sufferers in Japan, although the effect size (Cohen’s f 2) was small. Similar results were also observed in non-chronic headache sufferers (Table 2).
Our findings could contribute to the development of stress management strategies for headaches. Headache research has only recently reported stress management for headache sufferers [34, 35]. Global prevention-oriented stress management programs are designed to aid the acquisition of a repertoire of coping strategies, teach when and where strategies will be effective, and facilitate the selection of an appropriate strategy for a particular situation [36]. In addition, the transactional theory states that the inability to successfully cope with stressors or recognize that a coping strategy is ineffective contributes to long-term dysfunction among those who continue to struggle with chronic stress [19]. Therefore, in stress management for chronic pain, it may be important for sufferers to acquire flexible coping rather than specific coping strategies targeting pain-related distress.
Moreover, a recent study [3] suggests the importance of acceptance and commitment therapy (ACT) [37] for headaches, on the basis of evidence that ACT reduces pain intensity, pain-related anxiety, and depressive symptoms for sufferers with chronic pain. ACT aids in the acquisition of psychological flexibility, which refers to one’s ability to change or persist with a given behavior in the pursuit of one’s goals [37]. According to Kato [18], psychological flexibility is associated with the concept of coping flexibility measured in the present study. To our knowledge, no studies have yet examined the effects of psychological flexibility on pain-related distress among sufferers of chronic headaches. Therefore, a task for future research is to develop appropriate treatments for chronic headaches.
With regard to each coping strategy we surveyed, catastrophizing―which is a lack of confidence and control and an expectation of negative outcomes―was significantly associated with depressive symptoms later. Previous studies have found that catastrophizing may be the quintessential maladaptive coping strategy for chronic pain [38]. Several studies on coping with primary headaches have reported that catastrophizing is associated with a higher level of depressive symptoms [22]. Our finding is therefore consistent with previous research on chronic pain including headaches. Future investigations might explore whether interventions that decrease catastrophizing help reduce pain-related distress in chronic headache sufferers.
Limitations
Several limitations to the present study need to be mentioned, however. While the study sample included college students who reported having chronic daily headaches, it did not include clinical patients diagnosed with chronic headaches. In order to test the CFH in a diverse sample of chronic headache sufferers, we have planned to first recruit study participants from among college students, then from the general population, and finally from a clinical population. Thus, caution should be applied when generalizing our findings to general or clinical populations with chronic headaches.
Moreover, several methodological issues must also be addressed. All data were obtained from headache sufferers through self-reported measures. In our study, “chronic headache” was not defined according to specific clinical criteria, such as those of the International Classification of Headache Disorders, third edition. Therefore, ascertaining headache diagnoses is recommended for future studies. In addition, the present study did not assess variables related to headache intensity, which could potentially influence depressive symptoms later. Data related to headache intensity may help with ascertaining the effects of coping flexibility on depressive symptoms. A modified version of the CFS was used in the present study, and the alphas for the CFS scores were 0.71 for the CH group and 0.75 for the NCH group. These were lower estimates than those ranging from 0.83 to 0.90 for the original CFS [18]. In addition, only female participants were included in the present study, so it was not possible to address any questions related to gender differences. Finally, assessments of depressive symptoms with the CES-D were conducted 3 months later than the other assessments, in light of the potential influence of temporal relationships of flexibility in coping with chronic headaches on depressive symptoms. Thus, the influence of these different points of measurement should be taken into consideration when interpreting our findings.
In conclusion, data from Japanese females provided support for the CFH in incidences of chronic headache; coping flexibility attenuated the negative impact of chronic daily headaches on depressive symptoms. Our findings contribute to the development of future research on chronic headaches and highlight the need for researchers or practitioners to develop stress management programs that help sufferers acquire flexibility in coping with chronic headache.
References
Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from National Surveillance Studies. Headache. 2013;53:427–36.
Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. 1997;17:15–22.
Lake AE. Headache as a stressor: dysfunctional versus adaptive coping styles. Headache. 2009;49:1369–77.
Nash JM, Thebarge RW. Understanding psychological stress, its biological processes and impact on primary headache. Headache. 2006;46:1377–86.
Sauro KM, Becker WJ. The stress and migraine interaction. Headache. 2009;49:1378–86.
Antonaci F, Nappi G, Galli F, Manzoni GC, Calabresi P, Costa A. Migraine and psychiatric comorbidity: a review of clinical findings. J Headache Pain. 2011;12:115–25.
Heckman BD, Holroyd KA. Tension-type headache and psychiatric comorbidity. Curr Pain Headache Rep. 2006;10:439–47.
Blalock SJ, DeVellis BM, Holt K, Hahn PM. Coping with rheumatoid arthritis: is one problem the same as another? Health Educ Q. 1993;20:119–32.
Cheng C, Chan N, Chio JH, Chan P, Chan AO, Hui W. Being active or flexible? Role of control coping on quality of life among patients with gastrointestinal cancer. Psychooncology. 2012;21:211–8.
Cheng C, Yang F, Jun S, Hutton JM. Flexible coping psychotherapy for functional dyspeptic patients: a randomized, controlled trial. Psychosom Med. 2007;69:81–8.
Haythornthwaite JA, Menefee LA, Heinberg LJ, Clark MR. Pain coping strategies predict perceived control over pain. Pain. 1998;77:33–9.
Pakenham KI. Adjustment to multiple sclerosis: application of a stress and coping model. Health Psychol. 1999;18:383–92.
Roussi P, Krikeli V, Hatzidimitriou C, Koutri I. Patterns of coping, flexibility in coping and psychological distress in women diagnosed with breast cancer. Cogn Ther Res. 2007;31:97–109.
Rozanski A, Kubzansky LD. Psychological functioning and physical health: a paradigm of flexibility. Psychosom Med. 2005;67:S47–53.
Schmitz U, Saile H, Nilges P. Coping with chronic pain: flexible goal adjustment as an interactive buffer against pain-related distress. Pain. 1996;67:41–51.
Vriezekolk JE, van Lankveld WG, Eijsbouts AM, van Helmond T, Geenen R, van den Ende CH. The coping flexibility questionnaire: development and initial validation in patients with chronic rheumatic diseases. Rheumatol Int. 2012;32:2383–91.
Wieser T, Walliser U, Womastek I, Kress HG. Dysfunctional coping in headache: avoidance and endurance is not associated with chronic forms of headache. Eur J Pain. 2011;16:268–77.
Kato T. Development of the Coping Flexibility Scale: evidence for the coping flexibility hypothesis. J Couns Psychol. 2012;59:262–73.
Lazarus RS. Stress and emotion: a new synthesis. New York: Springer; 1999.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
Chiros C, O’Brien WH. Acceptance, appraisals, and coping in relation to migraine headache: an evaluation of interrelationships using daily diary methods. J Behav Med. 2011;34:307–20.
Materazzo F, Cathcart S, Pritchard D. Anger, depression, and coping interactions in headache activity and adjustment: a controlled study. J Psychosom Res. 2000;49:69–75.
Riley JL, Robinson ME. CSQ: five factors or fiction? Clin J Pain. 1997;13:156–62.
Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44.
Kato T. Frequently used coping scales: a meta-analysis. Stress Health. First published online, Dec 12, 2014. doi: 10.1002/smi.2557
Riley JL, Robinson ME, Geisser ME. Empirical subgroups of the Coping Strategies Questionnaire-Revised: a multi sample study. Clin J Pain. 1999;15:111–6.
Robinson ME, Riley JL, Myers CD, Sadler IJ, Kvaal SA, Geisser ME, et al. The Coping Strategies Questionnaire: a large sample, item level factor analysis. Clin J Pain. 1997;13:43–9.
Ulmer JF. An exploratory study of pain, coping, and depressed mood following burn injury. J Pain Symptom Manag. 1977;13:148–57.
Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Iwata N, Roberts CR, Kawakami N. Japan-U.S. comparison of responses to depression scale items among adult workers. Psychiatry Res. 1995;8:237–45.
Wong WS, Chen PP, Yap J, Mak KH, Tam BKH, Fielding R. Assessing depression in Chinese patients with chronic musculoskeletal pain: a comparison of three rating scales. J Affect Disord. 2011;133:179–87.
Hooten WM, Townsend CO, Decker PA. Gender differences among patients with fibromyalgia undergoing multidisciplinary pain rehabilitation. Pain Med. 2007;8:624–32.
Vriezekolk JE, Geenen R, van den Ende CHM, Slot H, van Lankveld WGJM, van Helmond T. Behavior change, acceptance, and coping flexibility in highly distressed patients with rheumatic diseases: feasibility of a cognitive-behavioral therapy in multimodal rehabilitation. Patient Educ Couns. 2012;87:171–7.
Becker WJ, Sauro KM. Recent studies on stress management-related treatments for migraine. Headache. 2009;49:1387–90.
Bromberg J, Wood ME, Black RA, Surette DA, Zacharoff KL, Chiauzzi EJ. A randomized trial of a web-based intervention to improve migraine self-management and coping. Headache. 2011;52:244–61.
Auerbach SM, Gramling SE. Stress management psychological foundations. Upper Saddle River: Prentice Hall; 1998.
Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press; 1999.
Edwards RR, Campbell C, Jamison RN, Wiech K. The neurobiological underpinnings of coping with pain. Curr Dir Psychol Sci. 2009;18:237–41.
Conflict of Interest
The author Kato declares that he has no conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the current study.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Kato, T. Effects of Flexibility in Coping with Chronic Headaches on Depressive Symptoms. Int.J. Behav. Med. 22, 506–511 (2015). https://doi.org/10.1007/s12529-014-9443-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-014-9443-1