Abstract
Background
Vascular risk factors such as hypertension and obesity have been associated with physical limitations among older adults.
Purpose
The purpose of this study is to examine whether individual and aggregated vascular risk factors (VRFs) are associated with functional dependence and to what extent carotid atherosclerosis (CAS) or peripheral artery disease (PAD) may mediate the possible associations of aggregated VRFs with functional dependence.
Method
This cross-sectional study included 1,451 community-living participants aged ≥60 years in the Confucius Hometown Aging Project of China. Data on demographic features, hypertension, high total cholesterol, obesity, smoking, physical inactivity, diabetes, CAS, PAD, and cardiovascular diseases (CVDs) were collected through an interview, a clinical examination, and laboratory tests. Functional dependence was defined as being dependent in at least one activity in the personal or instrumental activities of daily living. Data were analyzed using multiple logistic models controlling for potential confounders. We used the mediation model to explore the potential mediating effect of CAS and PAD on the associations of aggregated VRFs with functional dependence.
Results
Of the 1,451 participants, 222 (15.3 %) had functional dependence. The likelihood of functional dependence increased linearly with increasing number of VRFs (hypertension, high total cholesterol, abdominal obesity, and physical inactivity) (p for trend <0.002). Mediation analysis showed that controlling for demographics and CVDs up to 11 % of the total association of functional dependence with clustering VRFs was mediated by CAS and PAD.
Conclusion
Aggregation of multiple VRFs is associated with an increased likelihood of functional dependence among Chinese older adults; the association is partially mediated by carotid and peripheral artery atherosclerosis independently of CVDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maintenance of physical functional independence in late life is of the utmost importance for elderly individuals and their family, as well as for aging societies. Thus, understanding the influential factors and the pathway to the development of physical limitations and functional dependence has become a critical issue. Lifestyle- and metabolic-related vascular risk factors (VRFs), such as smoking, hypertension, hypercholesterolemia, diabetes mellitus, obesity, and physical inactivity are considered major risk factors for cardiovascular diseases (CVDs), including cerebrovascular disease [1–3]. In addition, several epidemiological studies have found VRFs to be independent predictors of physical limitations in older adults [4–8]. Most previous studies that have examined the association of VRFs with physical limitations have focused on individual factors [4–6, 8]. However, in a recent study of Swedish older people, we found that an increasing number of VRFs was linearly associated with an increased likelihood of mobility limitation [7]. This association persisted even after controlling for cardiovascular and cerebrovascular diseases, suggesting that the association of VRFs with physical limitation is independent of CVDs [7].
Carotid plaques and increased carotid intima-media thickness (cIMT), as markers of carotid atherosclerosis (CAS), have been associated with an increased risk of CVDs, mobility limitations, and functional dependence [9–11]. In addition, peripheral artery disease (PAD), as an atherosclerotic occlusive disease of the lower extremities, has been associated with CVDs, physical limitations, and functional dependence [12, 13]. CAS and PAD share common risk factors with CVDs [14, 15].
The association of VRFs with physical limitations may partly be explained by CVDs because VRFs cause CVDs, and physical limitations may be clinical manifestations of cardiovascular and cerebrovascular diseases [16, 17]. In addition, it has been suggested that VRFs may contribute to common geriatric syndromes, such as impaired cognitive and physical function, by causing cerebrovascular lesions through atherosclerosis [18].
On the basis of previous research, we hypothesize that VRFs play a role in the development of functional dependence partly through its impact on atherosclerosis and CVDs including cerebrovascular disease. In this population-based study of rural Chinese older adults, we seek to test this hypothesis by examining (1) whether individual and aggregated VRFs are associated with functional dependence and (2) to what extent CAS or PAD may mediate the possible associations of aggregated VRFs with functional dependence. To our knowledge, no studies have examined the association of VRF burden with functional dependence in Asian populations. Since most VRFs are amenable to intervention or management, an increased understanding of the vascular involvement in functional dependence may provide an opportunity for prevention of late-life functional dependence.
Methods
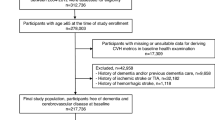
Study Participants
This is a population-based cross-sectional study. We used the data from the Confucius Hometown Aging Project (CHAP) [19]. The CHAP participants included all people who were aged ≥60 years and registered in the Xing Long Zhuang community in June 2010. The community is located approximately 20 km from Qufu (the hometown of Confucius) in Shandong, China. The primary aim of CHAP is to investigate health in aging by focusing on VRFs and atherosclerotic mechanisms in brain aging and dysfunction. The baseline data collection was conducted during June 2010–July 2011. Of all eligible subjects in the community (n = 1,743), 205 declined participation, lost contact, or died before the examination, and 1,539 (88.3 %) participated in the baseline examination. We excluded 88 persons with missing information on demographics, VRFs, functional status, CAS, and PAD, leaving 1,451 subjects for the current analyses. There were no significant differences in age (mean age ± SD, 68.6 ± 4.9 years vs. 68.7 ± 5.0, p = 0.412), gender (women: 59.0 % vs. 61.4 %, p = 0.661), or education (for people with no formal education: 32.2 % vs. 30.9 %, p = 0.808) between the analytical sample and the excluded subjects.
The CHAP study was approved by the Ethics Committee at Jining First People's Hospital of Jining Medical University, Shandong, China. Written informed consent was obtained directly from participants or, in case of cognitively impaired persons, from a proxy (usually the next of kin or guardian). Research within CHAP was conducted according to the principles expressed in the Declaration of Helsinki.
Data Collection and Definitions
In this cross-sectional study, data was collected through face-to-face interviews, clinical examinations, and laboratory tests by trained nurses, physicians, and technicians from the local Xing Long Zhuang Coal Mine Hospital that provides routine medical and health care services to residents of the local community. Before the baseline examination, the research staff of CHAP was trained by senior researchers and specialists from the Aging Research Center of Karolinska Institutet, Stockholm, Sweden. Epidemiological data was collected via a questionnaire that was developed by integrating the World Health Organization STEPwise approach to Surveillance (STEPS) and the Study on Global Ageing and Adult Health (SAGE) [19, 20]. We collected data on demographics (age, gender, and education), VRFs (e.g., smoking, hypertension, high total cholesterol, diabetes, obesity, and physical inactivity), CVDs (e.g., stroke and coronary heart disease), and use of medications (e.g., antihypertensive and blood glucose-lowering agents). Education was measured as the highest level of formal education and was categorized as no formal school, primary school, middle school, and high school or above.
Functional Dependence
Functional status was evaluated using personal and instrumental activities of daily living (P-ADL and I-ADL). Functional dependence was defined as being dependent in one or more of the following P-ADLs or I-ADLs: bathing, dressing, toileting, transferring/moving, feeding/eating, shopping, cooking, housework, washing clothes, and transportation [21, 22].
Assessments of Vascular Risk Factors and Cardiovascular Disease
Arterial blood pressure (systolic Korotkoff phase I and diastolic phase V) was measured twice on the right arm using a sphygmomanometer in the sitting position after at least a 5-min rest. The mean of the two readings was used in defining hypertension status, which was categorized as normotension (<120/80 mmHg, reference), prehypertension (120–139/80–89 mmHg), stage 1 hypertension (140–159/90–99 mmHg), and stage 2 hypertension (≥160/100 mmHg or current use of antihypertensive agents) [23].
High cholesterol was defined as a total serum cholesterol level ≥6.22 mmol/L [24].
Smoking status was categorized into never, former, or current smoking.
Abdominal obesity was defined as waist-to-height ratio (a ratio of waist circumference to body height in centimeters) ≥0.61, which was equivalent to the 75th percentile of the total sample [25]. Abdominal obesity was used in this study because a high waist-to-height ratio has been suggested to be superior to waist circumference and body mass index in defining cardiometabolic risk in both men and women of various ethnicities including Chinese adults [25, 26].
Leisure time physical exercise was assessed by two questions: (1) “How often do you currently exercise with moderate intensity (e.g. brisk walking, bike rides, volleyball games)?” and (2) “How often do you currently exercise more intensively?” Physical inactivity was defined as less than weekly participation in moderate or intensive physical exercise [27].
Diabetes was ascertained based on current use of oral glucose-lowering agents, insulin injection, or having a fasting blood glucose level ≥7.0 mmol/L or a non-fasting glucose level ≥11.0 mmol/L [28].
Coronary heart disease was ascertained based on self-reported history of the disease or abnormal electrocardiogram. Stroke was defined based on self-reported history of stroke.
Assessments of Atherosclerosis
CAS
The carotid arteries were examined with a color Doppler ultrasonography (Vivid 7 ultrasound system and a 7- to 10-MHz transducer) following a standardized protocol [29]. All participants were examined by one clinical sonographer alone. The cIMT was measured on the internal carotid arteries of each side and recorded to the nearest 0.1 mm. The average of three measurements for each side was used in the analysis, and the higher cIMT of the two sides was reported and used in the analysis. Carotid plaque was defined as focal encroachment of the common carotid artery walls in either side of the carotid artery. CAS was defined as the presence of a carotid arterial plaque or cIMT ≥1.81 mm in either side [9].
PAD
Systolic pressures at ankle and brachial arteries were measured using a Doppler ultrasonic device (8 MHz, Model L500VA, Vista AVSTM, USA) following a standardized protocol [30]. The ankle brachial index (ABI) for each side was calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure in the arm. The lower ABI of the two sides was reported. PAD was defined as ABI ≤0.90 in either side [30].
Data Analysis
Descriptive analysis was performed to show the distribution of demographic and clinical characteristics of the study participants by functional status. Statistical differences were examined using chi-square test or t test. Logistic regression analyses were conducted to estimate the odds ratio (OR) and 95 % confidence interval (CI) of functional dependence associated with individual and clustering of VRFs. We reported the results for individual VRFs and CVDs from two models: In model 1, individual VRFs and CVDs were analyzed separately, adjusting for demographics (age, gender, and education). In model 2, all VRFs and CVDs were included in the same model, along with demographic variables. The burden of VRFs was assessed by counting the number of those individual VRFs that were potentially associated with an increased OR of functional dependence in any model (p value ≤0.20); we hypothesized that the combination of these factors would increase the likelihood of functional dependence [7].
Results for the associations of functional dependence with aggregated VRFs were reported from four models: Model 1 was adjusted for demographics, model 2 included demographics and CVDs, in model 3, an additional adjustment was made for CAS, and in model 4, an additional adjustment was made for PAD. We used the mediation modeling analysis to explore the potential mediating effect of CAS and PAD on the associations of aggregated VRFs with functional dependence [31]. The mediation modeling provides estimates of the total effect, average mediation effect, direct effect, and the percentage of the total effect that is mediated by simulating predicted values of the mediator/outcome variable. The percentage of the total effect that is mediated may slightly differ from the result of dividing the average mediation effect by the total effect because simulations are used in the calculations [31]. Statistical interactions were tested by including the independent variables and their cross-product variables in the same model simultaneously. The p value <0.05 was considered as statistically significant. The STATA 12 software (StataCorp, 2011. College Station, TX: StataCorp LP) was used for all analyses.
Results
Of the 1,451 participants, 222 (15.3 %) had functional dependence. Among those with functional dependence, 101 (45.5 %) were dependent in 1 P-ADL or I-ADL activity, 64 (28.8 %) in 2 P-ADL or I-ADL activities, and 57 (25.7 %) were dependent in 3 or more P-ADL or I-ADL activities. The proportions of subjects who were dependent in each specific activity were 12.2 % for bathing, 4.5 % for dressing, 2.7 % for toileting, 1.8 % for transferring/moving, 0.9 % for feeding/eating, 73.9 % for shopping, 54.5 % for cooking, 9.0 % for housework, 17.6 % for washing clothes, and 28.8 % for transportation. Subjects with functional dependence were older, more often women, less educated, more likely to have CAS, stage 2 hypertension, high total cholesterol, abdominal obesity, stroke, and to be physically inactive (Table 1).
Table 2 shows the associations of individual VRFs and CVDs with functional dependence. Controlling for demographics (model 1), abdominal obesity, physical inactivity, stroke, and CAS were each significantly associated with an increased odds ratio of functional dependence. In model 2, when controlling for all VRFs, along with demographic and CVD variables, the associations of abdominal obesity and CAS with functional dependence were attenuated and no longer statistically significant. In model 1, four of those VRFs were either significantly (abdominal obesity, physical inactivity; p < 0.05) or potentially (stage 2 hypertension, high cholesterol; p < 0.20) associated with an increased likelihood of functional dependence. Therefore, in subsequent analyses, these four factors were aggregated to assess the burden of VRFs.
Controlling for demographics, the likelihood of functional dependence was linearly associated with an increasing number of VRFs (Table 3). The association of aggregated VRFs with functional dependence was attenuated but remained statistically significant when CVDs, CAS, and PAD, respectively, were further included in the model (Table 3, models 2, 3, and 4).
Table 4 shows the association of CAS and PAD with the burden of VRFs: controlling for demographics and CVDs, the likelihood of CAS and PAD was increased linearly with an increasing number of VRFs (p for linear trend <0.01). Because there was only one subject with PAD in the reference group of people with no VRF, in the additional analysis, we combined people with no VRF and those with one VRF as reference category. Compared with this reference category, the likelihood of PAD was 1.44 (95 % CI 0.97–2.13) when having two VRFs and 2.25 (95 % CI 1.46–3.45) when having three or more VRFs (p for linear trend = 0.02).
The mediation modeling analysis showed that CAS had a statistically significant (p < 0.05) or marginal effect (0.05 < p < 0.10) in mediating the association of functional dependence with burden of VRFs, whereas the average mediation effect of PAD was statistically non-significant (p > 0.05) (Table 5). The proportion of average mediation effect over the total effect on the association of functional dependence with burden of VRFs was approximately 6–11 % for CAS and 9–11 % for PAD (p < 0.05 or p < 0.10). In addition, the direct association of aggregated VRFs with functional dependence remains statistically marginal when the mediation effects of PAD and CAS were taken into account (Table 5).
We found no statistical interaction of aggregated VRFs with age or gender on functional dependence.
Discussion
In this population-based cross-sectional study of rural Chinese older adults, we found that an increasing number of VRFs (stage 2 hypertension, high total cholesterol, abdominal obesity, and physical inactivity) was linearly associated with an increased likelihood of functional dependence and that the association was partially mediated by CAS and PAD independently of CVDs. These results support the hypothesis that vascular pathways may be involved in late-life functional dependence.
For individual VRFs, we found that abdominal obesity was associated with functional dependence when adjusting for demographics. This is consistent with a previous study that found a high waist-to-height ratio at baseline to be associated with functional dependence 9 years later among middle-aged and older persons [8]. Obesity may lead to osteoarthritis due to joint wear, reduced exercise capacity, high levels of inflammation, and CVDs, which may partly explain its association with functional dependence. In addition, abdominal obesity has been a correlate of CAS [32]. We found that physical inactivity was associated with functional dependence, but this has to be interpreted with caution because of the potential reverse causality of physical inactivity with functional dependence in the cross-sectional design, i.e., although physical inactivity may contribute to functional dependence, people with functional dependence are also more likely to be physically inactive. Physical inactivity, as an important VRF, has been associated with an increased risk of CAS [33, 34].
For the aggregated VRFs, we found that the likelihood of functional dependence was increased linearly with increasing number of VRFs. This is in line with our previous study of Swedish elderly people, in which an aggregation of multiple VRFs was associated with an increased likelihood of mobility limitation defined as slow walking speed [7]. These studies indicate that an increased burden of VRFs may contribute both to the initial physical limitation defined as mobility limitation and to the progression from physical limitation to dependence in daily activities. Furthermore, the finding that an increasing number of VRFs is linearly associated with an increased likelihood of CAS and PAD is consistent with existing literature [14, 15].
Our results extend previous finding of the association of increased vascular risk burden with functional dependence among elderly persons by demonstrating that CAS and PAD play partial mediation effects on this association. The size of the mediating effects (up to 11 %) may be considered as a medium effect [35], but the effects are present independent of CVDs. One explanation for this finding may be that persons with more severe atherosclerosis are likely to have more microvascular injuries in the brain [36]. Previous studies have demonstrated that microvascular brain injuries are associated with physical limitations [37] and that the association of certain VRFs (e.g., hypertension) with physical limitation is mediated by the brain injuries [38]. Finally, PAD may also contribute to functional dependence through disabling leg pain, impaired muscle strength, and balance dependence [13].
A major strength of this study is that the study population consisted of older people living in a geographically defined rural area in China, largely representing the general older population in this region. Moreover, the participation rate was high, and those excluded subjects did not differ significantly from the participants in terms of age, gender, or education, and thus minimizes the selection bias. Finally, a broad range of VRFs were assessed using a standard and comprehensive approach such as face-to-face interviews, clinical examinations, and laboratory tests. Limitations of the study include the cross-sectional design, which restricts us from determining the direction of the observed associations. Moreover, possible selective survival bias due to the cross-sectional design may have led to underestimations of the association of VRFs with functional dependence. The study cohort is currently being followed, and the follow-up data may help to further clarify the associations of VRFs with late-life functional dependence.
In conclusion, this study provides evidence that the aggregation of multiple VRFs is associated with an increased likelihood of functional dependence in old age; both CAS and PAD may have partial mediating effects independent of CVDs. These results support the hypothesis that vascular pathways may be involved in late-life functional dependence. Although the study participants were from a rural area of China, the results are generally consistent with our previous study on Swedish elderly people living in central Stockholm. Given that China has the largest aging population in the world, identifying potentially manageable behavioral and metabolic factors that are associated with late-life functional dependence may have significant implications for public health as well as for sustainable development of China's economy and society.
References
Daviglus ML, Stamler J, Pirzada A, Yan LJL, Garside DB, Liu K, et al. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292:1588–92.
Ford ES, Li CY, Zhao GX, Pearson WS, Capewell S. Trends in the prevalence of low risk factor burden for cardiovascular disease among United States adults. Circulation. 2009;120:1181–8.
Sattelmair J, Pertman J, Ding EL, Kohl HW, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124:789–95.
Atkinson HH, Cesari M, Kritchevsky SB, Penninx BW, Fried LP, Guralnik J, et al. Predictors of combined cognitive and physical decline. J Am Geriatr Soc. 2005;53:1197–202.
Dumurgier J, Elbaz A, Dufouil C, Tavernier B, Tzourio C. Hypertension and lower walking speed in the elderly: the Three-City study. J Hypertens. 2010;28:1506–14.
Volpato S, Blaum C, Resnick H, Ferrucci L, Fried LP, Guralnik. Comorbidities and impairments explaining the association between diabetes and lower extremity disability: The Women's Health and Aging Study. Diabetes Care. 2002;25:678–83.
Welmer A, Angleman S, Rydwik E, Fratiglioni L, Qiu C. Association of cardiovascular burden with mobility limitation among elderly people: a population-based study. PLoS One. 2013;31:e65815.
Houston DK, Stevens J, Cai J. Abdominal fat distribution and functional limitations and disability in a biracial cohort: the Atherosclerosis Risk in Communities Study. Int J Obes. 2005;29:1457–63.
O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SKJ. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22.
Elbaz A, Ripert M, Tavernier B, Fevrier B, Zureik M, Gariepy J, et al. Common carotid artery intima-media thickness, carotid plaques, and walking speed. Stroke. 2005;36:2198–202.
den Ouden MEM, Schuurmans MJ, Mueller-Schotte S, Brand JS, van der Schouw YT. Domains contributing to disability in activities of daily living. J Am Med Dir Ass. 2013;14:18–24.
Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilson PWF. The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham study. Arch Intern Med. 2003;163:1939–42.
Kuo HK, Yu YH. The relation of peripheral arterial disease to leg force, gait speed, and functional dependence among older adults. J Gerontol A Bio Sci Med Sci. 2008;63:384–90.
Ostchega Y, Paulose-Ram R, Dillon CF, Gu QP, Hughes JP. Prevalence of peripheral arterial disease and risk factors in persons aged 60 and older: data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc. 2007;55:583–9.
Stensland-Bugge E, Bonaa KH, Joakimsen O. Age and sex differences in the relationship between inherited and lifestyle risk factors and subclinical carotid atherosclerosis: the Tromso study. Atherosclerosis. 2001;154:437–48.
Phan HM, Alpert JS, Fain M. Frailty, inflammation, and cardiovascular disease: evidence of a connection. Am J Geriatr Cardiol. 2008;17:101–7.
Kattainen A, Koskinen S, Reunanen A, Martelin T, Knekt P, Aromaa A. Impact of cardiovascular diseases on activity limitations and need for help among older persons. J Clin Epidemiol. 2004;57:82–8.
Pugh KG, Lipsitz LA. The microvascular frontal-subcortical syndrome of aging. Neurobiol Aging. 2002;23:421–31.
Song A, Liang Y, Yan Z, Sun B, Cai C, Jiang H, et al. Highly prevalent and poorly controlled cardiovascular risk factors among Chinese elderly people living in the rural community. Eur J Prev Cardiol. 2013. doi:10.1177/2047487313487621.
Kowal PCS, Naidoo N, Biritwum R, Fan W, Lopez Ridaura R, Maximova T, et al. Data resource profile: The World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidemiol. 2012;41:1639–49.
Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J Gerontol B Psychol Sci Soc Sci. 1998;53:S46–57.
LaPlante MP. The classic measure of disability in activities of daily living is biased by age but an expanded IADL/ADL measure is not. J Gerontol B Psychol Sci Soc Sci. 2010;65:720–32.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Third Report of the National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–4321.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Dong X, Liu Y, Yang J, Sun Y, Chen L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a Chinese population. Postgrad Med J. 2011;87:251–6.
Rydwik E, Welmer AK, Kåreholt I, Angleman S, Fratiglioni L, Wang HX. Adherence to physical exercise recommendations in people over 65—the SNAC-Kungsholmen study. Eur J Public Health. 2013. doi:10.1093/eurpub/cks150.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–8.
O'Leary DH, Polak JF, Wolfson SKJ, Bond MG, Bommer W, Sheth S, et al. Use of sonography to evaluate carotid atherosclerosis in the elderly: the Cardiovascular Health Study. Stroke. 1991;22:1155–63.
Grenon SM, Gagnon J, Hsiang Y. Video in clinical medicine. Ankle-brachial index for assessment of peripheral arterial disease. N Engl J Med. 2009;36(361):e340.
Hicks R, Tingley D. Causal mediation analysis. Stata J. 2011;11:605–19.
Maher V, O'Dowd M, Carey M, Markham C, Byrne A, Hand E, et al. Association of central obesity with early Carotid intima-media thickening is independent of that from other risk factors. Int J Obes. 2009;33:136–43.
Sacco RL. Achieving ideal cardiovascular and brain health: opportunity amid crisis. Presidential Address at the American Heart Association 2010 Scientific Sessions. Circulation. 2011;123:2653–7.
Thijssen DHJ, Cable NT, Green DJ. Impact of exercise training on arterial wall thickness in humans. Clin Sci (Lond). 2012;122:311–22.
Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16:93–115.
Bots ML, Vanswieten JC, Breteler MMB, Dejong P, Vangijn J, Hofman A, et al. Cerebral white matter lesions and atherosclerosis in the Rotterdam study. Lancet. 1993;341:1232–7.
Zheng JJ, Delbaere K, Close JC, Sachdev PS, Lord SR. Impact of white matter lesions on physical functioning and fall risk in older people: a systematic review. Stroke. 2011;42:2086–90.
Hajjar I, Quach L, Yang F, Chaves PH, Newman AB, Mukamal K, et al. Hypertension, white matter hyperintensities, and concurrent impairments in mobility, cognition, and mood: the Cardiovascular Health Study. Circulation. 2011;123:858–65.
Acknowledgments
The Confucius Hometown Aging Project (CHAP) was supported in part by grants from the Department of Science and Technology (2008GG00221) and the Department of Health (2009-067) in Shandong, China and by the Young Scholar Grant for Strategic Research in Epidemiology at Karolinska Institutet, Stockholm, Sweden. We thank all CHAP participants for their contribution to the project and the CHAP Study Group for their collaboration in data collection and management. Dr. Welmer was supported in part by grants from the Stockholm County Council, and Dr. Qiu was supported by grants from Swedish Research Council and Karolinska Institutet, Stockholm, Sweden.
Conflict of Interest
The authors declare no conflicts of interest. The funding sources had no role in the study design, data collection, analysis, or interpretation of the results.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Welmer, AK., Liang, Y., Angleman, S. et al. Vascular Risk Factor Burden, Atherosclerosis, and Functional Dependence in Old Age: A Population-Based Study. Int.J. Behav. Med. 21, 597–604 (2014). https://doi.org/10.1007/s12529-013-9352-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-013-9352-8