Abstract
Background
Previous studies investigated the association between gestational anemia and neonatal outcomes. However, few studies explored whether the effects of gestational anemia could be eliminated by subsequent correction of anemia in the later stages of pregnancy. This study aimed to investigate the relationship between anemia in different trimesters and neonatal outcomes.
Methods
The study was conducted in Shanghai, China, with a sample of 46,578 pregnant women who delivered between January 1, 2016 and July 1, 2019. A multivariable logistic regression model was adopted to analyse the associations between maternal anemia and neonatal outcomes.
Results
The incidence of gestational anemia was 30.2%, including 4.4% in the first trimester, 9.6% in the second trimester, and 16.2% in the third trimester. Only 24.5% (507/2066) of anemia that occurred in the first trimester and 29.6% (1320/4457) that occurred in the second trimester could be corrected in the later stages of pregnancy. Anemia occurring in the first trimester was associated with small for gestational age [odds ratio (OR) 1.46; 95% confidence interval (CI) 1.20–1.78] and with fetal distress (OR 1.23; 95% CI 1.08–1.40). Anemia corrected in the first trimester also was associated with a higher risk of small for gestational age.
Conclusions
Gestational anemia is a public health problem in China impacting neonatal health. Anemia in pregnancy could be corrected in only about a quarter of the women. Anemia in the first trimester, whether corrected or not, still led to lower birth weight; therefore, the prevention of anemia prior to pregnancy is important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pregnant women are more likely to suffer from anemia owing to increased blood volume during pregnancy [1] and to a greater demand for nutrients during fetal growth [2]. Generally, 500–800 mg of maternal iron are required for a normal singleton pregnancy [3]. Compared with non-pregnant women of childbearing age, the folate requirement increases from 400 to 600 μg/day [4]. A multicenter study reported that the incidence of gestational anemia ranged from 22 to 56% [5] and was about 23.5% in China, according to a global survey in 2011 [6]. Another study in China showed that the prevalence of gestational anemia and iron deficiency anemia was 19.8% and 13.9%, respectively [7]. Moreover, the incidence of thalassemia was high in certain provinces of China, such as Guangdong [8].
Some clinical studies showed that anemia during pregnancy was associated with stillbirth [9], preterm birth (PTB) [10], and low birth weight (LBW) [11]. Anemia during pregnancy also was reported to be associated with placental development [12,13,14]. The duration of pregnancy is divided into three trimesters: the first trimester (< 14 weeks), the second trimester (14–27+6 weeks), and the third trimester (≥ 28 weeks). Organogenesis takes place in the first trimester of pregnancy, during which the preliminary structure of most organs develop, such as the heart, lung, liver, and so forth. However, in later trimesters these organs need to experience further growth and maturation [15]. In the early stage of development, the embryo and the fetus are subjected to intensely epigenetic reprogramming [16,17,18]. Previous studies showed that epigenetic changes might play an important role in offspring diseases caused by gestational complications, intrauterine environment [19], and abnormal nutritional status [20]. These adverse outcomes can even be inherited across generations [21]. As one of the most common gestational complications, the environment of nutritional deficiency and hypoxia caused by anemia during pregnancy also may lead to the occurrence of various chronic diseases in adulthood [22].
Previous studies reported associations between gestational anemia and neonatal outcomes, most of which focused on only one trimester of pregnancy [10, 11, 23,24,25,26,27,28]. However, the findings are conflicting. The role of anemia in the three trimesters of pregnancy and its association with adverse neonatal outcomes remains unclear. Previous studies reported that anemia in the first trimester was more harmful [28]. This study aimed to establish whether anemia-induced adverse outcomes in the early stage of pregnancy could be avoided by correcting anemia during the later stages of pregnancy.
Methods
Study setting
This retrospective cohort study was conducted at the International Peace Maternal and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China.
Ethics
The ethical approval for this study was granted by the Ethics Committee of the International Peace Maternity and Child Health Hospital.
Inclusion criteria
Pregnant women who delivered between January 1, 2016 and July 1, 2019 with complete records of hemoglobin levels in each of the three trimesters and who underwent a single live birth no earlier than 28 weeks of gestation were included in this study.
Data collection
Data on maternal age, pre-pregnancy body mass index, education level, parity, residence, fetal sex, birth weight, and gestational age of the participants were extracted from the electronic medical information system. Data collection was conducted from December 15, 2019 to January 10, 2020.
Case definitions
Gestational anemia was defined as hemoglobin < 110 g/L in the first and third trimesters and < 105 g/L in the second trimester, according to the latest guideline of the World Health Organization (WHO) [29]. In the present study, recovered anemia was defined as anemic in the first trimester and non-anemic in the second and third trimesters. If anemia in the first trimester was combined with anemia in the second or third trimester, it was considered as persistent anemia. Gestational age was based on the last menstrual period and was confirmed with the first-trimester ultrasound examination. The residence of the participants was classified into Shanghai's local and migrant residence according to the maternal domicile. Maternal education was classified using the following two levels: college education or higher and high school education or lower. The Apgar score was evaluated one min after birth, based on the following five categories: breathing effort, heart rate, muscle tone, reflexes, and skin color. Fetal distress was diagnosed at the International Peace Maternity and Child Health Hospital based on the International Classification of Diseases, 10th Revision codes. Small for gestational age (SGA) was defined as birth weight below the tenth percentile for gestational age–specific birth weight distribution [30]. LBW was defined as birth weight < 2500 g, and macrosomia was defined as birth weight > 4000 g. PTB was defined as a gestational age between 28+0 and 36+6 weeks at delivery.
Statistical analysis
Statistical analyses were performed using SPSS version 25 software (IBM, SPSS Statistics, NY, USA). The categorical variables were presented as number and percentage, and continuous variables were reported as median and interquartile range. The associations between gestational anemia, SGA, LBW, Apgar score < 8, and PTB were analyzed using a multivariable logistic regression model. Statistical significance was set at P < 0.05. Potential confounding variables (P < 0.05) including maternal age at the register, pre-pregnancy body mass index, categories of education level, parity, residence, and neonatal sex were included in the regression model.
Results
The details of 56,729 women who delivered between January 1, 2016 and July 1, 2019 were recorded in the electronic system of the International Peace Maternal and Child Health Hospital (Fig. 1). Of these, 1,719 women with multiple births, 103 with stillbirth, 21 who delivered before 28 weeks of gestational age, and 8,308 with missing hemoglobin records were excluded. Of the 46,578 pregnant women included in our study, 69.8% (32,500/46,578) had a normal hemoglobin and 30.2% (14,078/46,578) had anemia during their pregnancy, including 4.4% (2066/46,578), 9.6% (4457/46,578), and 16.2% (7555/46,578) who suffered in the first, second, and third trimester, respectively. In the first trimester of pregnancy, 2066 (4.4%) women experienced anemia. Of these, anemia of 507 (24.5%) women was absolutely corrected in both the second and third trimesters; 15.9% (329/2066) of women were anemic in the first and third trimesters, 8.3% (171/2066) in the first and second trimesters, and 51.3% (1059/2066) in all three trimesters. Moreover, anemia of 29.6% (1320/4457) of women in the second trimester could be corrected in the third trimester. In the anemic groups, maternal age, proportion of parous women, and ferritin level < 30 μg/L were higher. Maternal pre-pregnancy body mass index, proportion of Shanghai locals, male newborns, and college education or higher were lower among women with anemia (Table 1).
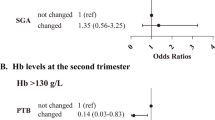
Gestational anemia in the first trimester was associated with higher risks of SGA and fetal distress (Table 2). Anemia in the second trimester was associated with lower risks of SGA, LBW, and PTB, and a higher risk of macrosomia. Anemia in the third trimester was associated with higher risks of Apgar score < 8 and macrosomia, and lower risks of SGA, LBW, and PTB.
Gestational anemia in the first trimester was associated with lower birth weight and with a higher risk of fetal distress (Table 2). Therefore, a further analysis was conducted to explore whether maternal anemia was also associated with lower birth weight and fetal distress and whether anemia in the first trimester could be corrected in both the second and third trimesters. A higher risk of SGA was associated with both corrected and persistent anemia, and a higher risk of fetal distress was associated with only persistent anemia but not corrected anemia. No significant association was found between persistent anemia, corrected anemia, and LBW (Table 3).
The normal, corrected anemia, and persistent anemia groups comprised 14.3%, 47.7%, and 30.3% of women, respectively, with a ferritin level of < 30 μg/L. Anemia in the first trimester with ferritin < 30 μg/L was associated with a higher risk of SGA, but not in subgroups of ferritin level ≥ 30 μg/L. Moreover, persistent anemia with a ferritin level < 30 μg/L was associated with a higher risk of LBW. Persistent anemia with both ferritin levels < 30 μg/L and ≥ 30 μg/L was associated with a higher risk of fetal distress (Table 4).
Discussion
The prevalence of gestational anemia was 30.2% in the present cohort, and the incidence was higher in the third trimester. Once anemia occurred in the first trimester, only 24.5% could be corrected. Gestational anemia in various trimesters was associated with different neonatal outcomes. Maternal anemia in the first trimester of pregnancy was associated with higher risks of SGA and fetal distress. Anemia in the second trimester was negatively associated with the risk of PTB, SGA, and LBW, but was positively associated with macrosomia. Anemia in the third trimester was associated with lower risks of SGA, PTB, and LBW, but also included a higher risk of Apgar score < 8 and macrosomia. Anemia in the first trimester played more important roles in a higher risk of SGA and fetal distress. Whether these impacts could be eliminated in the latter two trimesters needed to be determined. This study found that even if anemia in the first trimester of pregnancy was completely corrected, it still led to an increased risk of SGA. If not recovered, anemia in the first trimester further led to fetal distress in addition to SGA. With more detailed analysis by the level of maternal ferritin, we found that persistent anemia also was associated with a higher risk of LBW under the condition of ferritin < 30 μg/L, but not in the recovered group.
The incidence of anemia in the present cohort was comparable with results previously reported in China [6, 7]. In accordance with a previous investigation of PTB, our study found a negative association between anemia in the last two trimesters and PTB [10]. One study showed that anemia in the first, but not in the second or third trimesters, led to LBW [28]. Another study in India showed that the mean birth weight was lower in the group with anemia in the third trimester [31]. However, in both of these studies, the sample size was not large enough. In the present study, anemia in the second and third trimesters was found to be associated with a higher risk of macrosomia, and a similar result was reported in another study [32]. The author explained that maternal anemia might cause placental hyperplasia and better nutritional support. In this study, the higher speed of fetal development in the later stage of pregnancy also might be a risk factor for maternal anemia owing to the concurrence of a higher ratio of macrosomia. The persistent anemia group did not exhibit a much higher risk of SGA, and its pathogenesis was thought to be more complicated but not iron deficiency. The serum ferritin test was thought to be the most effective method to diagnose iron deficiency [33]. Iron deficiency is defined as serum ferritin level less than 10, 15, or 30 μg/L according to different guidelines; a threshold of 30 μg/L is 98% specific and 92% sensitive for the diagnosis of iron deficiency [34] according to the UK guideline [35]. Continued iron deficiency can lead to iron deficiency anemia. Folate deficiency is defined as serum folate level less than 6.8 nmol/L. However, a single test of serum folic acid can only stand for a transient status of folate concentration [36]. In our study few women with folate deficiency were found, which might also benefit from the policy of folic acid supplementation before pregnancy to prevent neural tube defects [37]. Hence, a more detailed analysis by stratification was conducted based on the ferritin level. The pregnant women with low ferritin levels accounted for most of the remediable group. However, the pathogenesis in the intractable group starting from the first trimester seemed to be more complicated, which might be due to an imbalanced nutritional intake because the level of folic acid was slightly lower, but iron deficiency was not obvious. If ferritin was less than 30 μg/L, a higher risk of SGA was found, and the persistent anemic group was associated with a higher risk of LBW. Iron deficiency anemia was associated with lower birth weight reported formerly [38].
This study was novel in exploring whether newborns of pregnant women who recovered from anemia were associated with adverse neonatal outcomes. Complete records on hemoglobin levels in all three pregnancy stages allowed us to conduct a more detailed analysis of the effect of exposure window of anemia. Also, the serum ferritin and folic acid levels were tested in most of the included cases. Anemic women with low ferritin levels had no folic acid deficiency. Based on the characteristics of the present cohort, the results of serum ferritin levels and trimesters in which anemia occurred were combined for further stratification. Our findings showed that even corrected anemia led to SGA, which is the core content of the developmental origins of health and disease [39] and is associated with a higher risk of mortality in newborns [40] and children [41]. These findings suggested that the prevention of anemia before pregnancy was important. In contrast to the suggestion of the WHO [29], the UK guideline [35] suggested that pregnant women took elemental iron only if the serum ferritin level was less than 30 μg/L. Moreover, based on the results of our study, it was presumed that ferritin detection in the last two trimesters, not only in the first trimester, should be emphasized.
However, the present study also had some limitations. First, as a single-center retrospective cohort, the biases caused by geography, medical processes, or the environment could not be completely excluded. Whether the patients took supplemental pills at home, as prescribed by the doctors, was not certain. Second, the nutritional condition in the other two trimesters of pregnancy is uncertain, and the influence of inflammation on serum ferritin cannot be excluded. Further studies are needed also to resolve the remaining shortcomings of the present study. In particular, multicenter surveys with pregnant women from other provinces and hospitals in China can help in knowing the global status of anemia control. In addition, prospective and randomized controlled trials should be conducted to know which guidelines and dosages of iron supplementation would provide greatest benefit to anemic pregnant women.
In conclusion, the incidence of gestational anemia is high. Maternal anemia is associated with an increased risk of SGA, LBW, fetal distress, and lower Apgar score. It is difficult to recover from anemia occurring in the first trimester of gestation. Even if corrected, it can still lead to a higher risk of SGA. The results of the present study indicated that more attention should be paid to the prevention of anemia before pregnancy; otherwise, it may result in irreversible adverse pregnancy outcomes.
References
Churchill D, Nair M, Stanworth SJ, Knight M. The change in haemoglobin concentration between the first and third trimesters of pregnancy: a population study. BMC Pregnancy Childbirth. 2019;19:359–64.
Fisher AL, Nemeth E. Iron homeostasis during pregnancy. Am J Clin Nutr. 2017;106:1567–74.
Milman N, Bergholt T, Byg KE, Eriksen L, Graudal N. Iron status and iron balance during pregnancy. A critical reappraisal of iron supplementation. Acta Obstet Gynecol Scand. 1999;78:749–57.
Marangoni F, Cetin I, Verduci E, Canzone G, Giovannini M, Scollo P, et al. Maternal diet and nutrient requirements in pregnancy and breastfeeding. An Italian consensus document. Nutrients. 2016;8:629–45.
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16-25.
Lin L, Wei Y, Zhu W, Wang C, Su R, Feng H, et al. Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: a multicentre retrospective study. BMC Pregnancy Childbirth. 2018;18:111–8.
Tan J, He G, Qi Y, Yang H, Xiong Y, Liu C, et al. Prevalence of anemia and iron deficiency anemia in Chinese pregnant women (IRON WOMEN): a national cross-sectional survey. BMC Pregnancy Childbirth. 2020;20:670–81.
Yin A, Li B, Luo M, Xu L, Wu L, Zhang L, et al. The prevalence and molecular spectrum of alpha- and beta-globin gene mutations in 14,332 families of Guangdong Province, China. PLoS ONE. 2014;9:e89855.
Sun CC, Chou HH, Chuang LL. Trends and risk factors of stillbirth in Taiwan 2006–2013: a population-based study. Arch Gynecol Obstet. 2019;299:961–7.
Zhang Q, Ananth CV, Li Z, Smulian JC. Maternal anaemia and preterm birth: a prospective cohort study. Int J Epidemiol. 2009;38:1380–9.
Figueiredo ACMG, Gomes-Filho IS, Silva RB, Pereira PPS, Mata FAFD, Lyrio AO, et al. Maternal anemia and low birth weight: a systematic review and meta-analysis. Nutrients. 2018;10:601–17.
Lelic M, Bogdanovic G, Ramic S, Brkicevic E. Influence of maternal during pregnancy on placenta and newborns. Med Arch. 2014;68:184–7.
Stangret A, Skoda M, Wnuk A, Pyzlak M, Szukiewicz D. Mild anemia during pregnancy upregulates placental vascularity development. Med Hypotheses. 2017;102:37–40.
Larsen S, Bjelland EK, Haavaldsen C, Eskild A. Placental weight in pregnancies with high or low hemoglobin concentrations. Eur J Obstet Gynecol Reprod Biol. 2016;206:48–52.
Embryogenesis and fetal morphological development. In: Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, et al., editors. Williams obstetrics. 24th ed. McGraw-Hill; 2014. p. 127–53.
Liu X, Wang C, Liu W, Li J, Li C, Kou X, et al. Distinct features of H3K4me3 and H3K27me3 chromatin domains in pre-implantation embryos. Nature. 2016;537:558–62.
Wang C, Liu X, Gao Y, Yang L, Li C, Liu W, et al. Reprogramming of H3K9me3-dependent heterochromatin during mammalian embryo development. Nat Cell Biol. 2018;20:620–31.
Li L, Guo F, Gao Y, Ren Y, Yuan P, Yan L, et al. Single-cell multi-omics sequencing of human early embryos. Nat Cell Biol. 2018;20:847–58.
Tian S, Lin XH, Xiong YM, Liu ME, Yu TT, Lv M, et al. Prevalence of prediabetes risk in offspring born to mothers with hyperandrogenism. Ebiomedicine. 2017;16:275–83.
Rooij SR, Painter RC, Roseboom TJ, Phillips DI, Osmond C, Barker DJ, et al. Glucose tolerance at age 58 and the decline of glucose tolerance in comparison with age 50 in people prenatally exposed to the Dutch famine. Diabetologia. 2006;49:637–43.
Li J, Liu S, Li S, Feng R, Na L, Chu X, et al. Prenatal exposure to famine and the development of hyperglycemia and type 2 diabetes in adulthood across consecutive generations: a population-based cohort study of families in Suihua, China. Am J Clin Nutr. 2017;105:221–7.
Barker DJ, Osmond C. Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. Lancet. 1986;1:1077–81.
Fowkes FJI, Moore KA, Opi DH, Simpson JA, Langham F, Stanisic DI, et al. Iron deficiency during pregnancy is associated with a reduced risk of adverse birth outcomes in a malaria-endemic area in a longitudinal cohort study. BMC Med. 2018;16:156–65.
Symington EA, Baumgartner J, Malan L, Wise AJ, Ricci C, Zandberg L, et al. Maternal iron-deficiency is associated with premature birth and higher birth weight despite routine antenatal iron supplementation in an urban South African setting: the NuPED prospective study. PLoS ONE. 2019;14:e221299.
Smith C, Teng F, Branch E, Chu S, Joseph KS. Maternal and perinatal morbidity and mortality associated with anemia in pregnancy. Obstet Gynecol. 2019;134:1234–44.
Oaks BM, Jorgensen JM, Baldiviez LM, Adu-Afarwuah S, Maleta K, Okronipa H, et al. Prenatal iron deficiency and replete iron status are associated with adverse birth outcomes, but associations differ in Ghana and Malawi. J Nutr. 2019;149:513–21.
Haider BA, Olofin I, Wang M, Spiegelman D, Ezzati M, Fawzi WW. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2013;346:f3443.
Hamalainen H, Hakkarainen K, Heinonen S. Anaemia in the first but not in the second or third trimester is a risk factor for low birth weight. Clin Nutr. 2003;22:271–5.
WHO. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016.
Zhu L, Zhang R, Zhang S, Shi W, Yan W, Wang X, et al. Chinese neonatal birth weight curve for different gestational age. Zhonghua Er Ke Za Zhi. 2015;53:97–103.
Kumar KJ, Asha N, Murthy DS, Sujatha M, Manjunath V. Maternal anemia in various trimesters and its effect on newborn weight and maturity: an observational study. Int J Prev Med. 2013;4:193–9.
Gabriela B, Christian B. Mild anemia and pregnancy outcome in a Swiss collective. J Pregnancy. 2014;2014:307535.
Byg KE, Milman N, Hansen S, Agger AO. Serum ferritin is a reliable, non-invasive test for iron status in pregnancy: comparison of ferritin with other iron status markers in a longitudinal study on healthy pregnant women. Hematology. 2000;5:319–25.
Means RT. Iron deficiency and iron deficiency anemia: implications and impact in pregnancy, fetal development, and early childhood parameters. Nutrients. 2020;12:447–61.
Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2012;156:588–600.
WHO. Serum and red blood cell folate concentrations for assessing folate status in populations. Geneva: World Health Organization; 2012.
WHO. Optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects. Geneva: World Health Organization, 2015.
Julia LF, Anura VK, Beena B, Tinku T, Krishnamachari S, Christopher D. Anaemia and iron deficiency in pregnancy and adverse perinatal outcomes in Southern India. Eur J Clin Nutr. 2018;74:112–25.
Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311:171–4.
Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–25.
Ludvigsson JF, Lu D, Hammarstrom L, Cnattingius S, Fang F. Small for gestational age and risk of childhood mortality: a Swedish population study. PLoS Med. 2018;15:e1002717.
Acknowledgements
The authors would like to thank Lei Chen and Ping Wang in International Peace Maternity and Child Health Hospital for their efforts in data collection.
Funding
This work was supported by the Special Fund for the National Key Research and Development Plan Grant (2017YFC1001300), the International Cooperation Project of China and Canada NSFC (81661128010), the Major Program of National Natural Science Foundation of China (81490742), the Natural Science Foundation of China (31571556), Innovative research team of high-level local universities in Shanghai, and Shanghai Municipal Key Clinical Speciality, Shanghai, China.
Author information
Authors and Affiliations
Contributions
HFH, GLD, CFS, XML, and ZYZ participated in the conceptualization of the study. HHF had full access to all data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. CFS wrote the original draft. CFS and HL conducted the formal analysis. GLD, HFH, and JZS reviewed and edited the manuscript. YHH, KXZ, and HTH provided supports on methodology. All authors commented on the drafts and approved the final draft.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the International Peace Maternity and Child Health Hospital (GKLW) 2017–81.
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, CF., Liu, H., Hao, YH. et al. Association between gestational anemia in different trimesters and neonatal outcomes: a retrospective longitudinal cohort study. World J Pediatr 17, 197–204 (2021). https://doi.org/10.1007/s12519-021-00411-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00411-6