Abstract
Background
This study aims to determine whether the suppression of myocardial FDG uptake and detection of infectious endocarditis (IE) may be enhanced when FDG-PET is repeated on the next day while maintaining patients on a ketogenic diet in the interim.
Methods
Seventeen patients with definite IE underwent FDG-PET investigations both after a conventional metabolic preparation (> 12-hour fast after a low-carbohydrate evening meal) and a subsequent 12-hour extension of the low-carbohydrate diet followed by an additional > 12-hour fast.
Results
Plasma biomarkers showed increased ketogenic metabolism between the two FDG-PET scans. A myocardial FDG uptake persisted on the 1st PET in 9 patients (53%) for whom myocardial FDG uptake decreased significantly on the 2nd PET (SUVmax: 6.05 ± 3.25 vs 4.32 ± 3.47, P = 0.021), resulting in an enhancement in the diagnostic confidence of IE in 6 cases. These enhancements were not documented in the 8 patients exhibiting a total suppression of myocardial FDG uptake on the 1st PET.
Conclusions
Better suppression of myocardial uptake and enhanced detection of IE may be achieved when an FDG-PET, showing an incomplete suppression of the myocardial FDG uptake, is repeated as soon as the next day, while maintaining patients on a ketogenic diet in the interim.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
18F-Fluorodeoxyglucose positron emission tomography (FDG-PET) is increasingly used to detect infective endocarditis (IE)1 and to identify additional infectious sites.2 A low-carbohydrate dinner, followed by a prolongation of the fast, is recommended to improve IE detection by 18F-Fluorodeoxyglucose positron emission tomography (FDG-PET).3,4,5 This metabolic preparation could be further enhanced by longer fasting periods (> 18 hours) or the consumption of at least two low‐carbohydrate meals the day before the study, as recommended by the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the American Society of Nuclear Cardiology (ASNC) for the FDG-PET imaging of cardiac sarcoidosis.6 But these protocols do not always suppress all myocardial FDG signals,7 and this may potentially affect the detection of IE.
Following a low-carbohydrate diet over several days prior to FDG-PET may also lower myocardial FDG uptake.8,9,10
Recently, the combination of a 72‐hour daytime ketogenic diet with a with 3 overnight fasts was found to provide a high suppression of the myocardial FDG signal.11 However, this method is difficult to adapt to IE patients in precarious medical condition, particularly considering that an accurate FDG-PET analysis of cardiac valve areas is achieved with a conventional regimen in the majority of cases. Nevertheless, no study has to date evaluated shorter periods of such low-carbohydrate diets when followed or preceded by fasting in the context of IE detection or IE management.
The current study aims (ii) to determine whether the suppression of myocardial FDG uptake and detection of IE may be enhanced when FDG-PET is repeated on the next day while maintaining patients on a ketogenic diet in the interim and (ii) to test that such a diet is tolerated by IE patients.
Materials and Methods
Study Population and Study Design
The study recruited consecutive patients hospitalized at the Nancy university hospital for a definite IE, which satisfied the Duke-Li criteria.1 None of the patients had taken antibiotics for more than 8 days prior to the first FDG-PET scan. None of the female patients were pregnant.
As detailed in Figure 1, enrolled patients underwent a first FDG-PET after a conventional metabolic preparation (≥ 12-hour fast after a low-carbohydrate evening meal) and a second FDG-PET the next day, after switching to a 12-hour high-lipid high-protein diet comprising ≤ 3 g carbohydrates followed by another ≥ 12 hours of fasting.
Approval for this study was obtained from the institutional Ethics Committee (Comité de Protection des Personnes OUEST 3). All patients enrolled in the study signed written informed consent. The study protocol is released on the ClinicalTrials.gov site under the identifier: NCT03465098
FDG-PET Recording and Analysis
PET images were obtained on a Vereos digital-PET/CT system (Philips, Cleveland, Ohio) in full 3D with 1.5 min recordings per bed position, 1 hour after an intravenous injection of 3 MBq·kg 18F-FDG.
Complete blood sampling for measuring plasma biomarker concentrations listed in Table 1, was attempted before each PET/CT investigation but was not obtained for all IE patients examined (depending on veinous conditions).
PET images were reconstructed using an OSEM method12 with and without a CT-based attenuation and analyzed by two independent observers on a MIM workstation (MIM Software Inc., Cleveland, Ohio) to visually detect IE and determine FDG activities from endocarditis, myocardial and blood areas.
IE foci should be detected on both corrected and non-corrected PET images, and with the criterion of a heterogeneous uptake pattern for IE on prosthetic valves.3 This visual analysis was conducted to reflect the two-step protocol of the study, i.e., an initial analysis of only the 1st PET followed by the analysis of both PET scans to assess the added value of the 2nd PET. The suppression of myocardial FDG uptake was graded as either complete or incomplete on the 1st PET. Incomplete uptake was defined by the visualization of myocardial areas exhibiting a higher activity than the LV blood cavity.
Spherical regions-of-interest (VOIs) were used to determine: (1) the SUV max from IE foci detected visually, (2) the SUV max from the myocardium with careful exclusion of extracardiac and valve areas, and (3) a mean blood SUV within the mid-portion of the descending aorta and with a 20 mm diameter VOI.
A myocardial SUV mean value was additionally determined within 3D regions-of-interest (VOIs) and positioned on a midventricular short-axis CT slice. This ring-shaped VOI of one cm width encompassed the lateral half of the left ventricle. Quantitative variables were averaged between the two observers. Results from the visual analyses were obtained by an additional consensual analysis between the observers for any of the discordant cases.
Statistical Analyses
Continuous variables were expressed as mean ± SD and categorical variables, as percentages. Quantitative variables were compared with the Wilcoxon test for paired comparisons and the Mann-Whitney test for unpaired comparisons. P values < .05 were considered significant.
Results
A total of 25 patients with definite IE were initially included in the study, 8 patients were subsequently excluded (1 died before the 1st PET, 2 withdrew their consent before the 2nd PET, 4 could not comply with the low-carbohydrate diet, as reported by the medical staff or the patients themselves, and PET images could not be analyzed for one of the patients), leaving 17 patients in the final analysis. As detailed in Table 1, the mean age was 73 ± 16 years, 3 patients were women, and 12 patients had one or two cardiac prothesis implants.
As detailed in Table 2, there was evidence of a significant increase in ketogenic metabolism, reflected by an increase in plasma beta-hydroxybutyrate between the 1st and 2nd PET (P = 0.022), associated with decreased insulinemia (P = 0.043).
IE foci were detected by FDG-PET in a total of 15 patients, and in 2 cases (patients # 1 and 2 in Figure 2) in only the 2nd PET. None of the IE foci were only detected in the 1st PET. The 15 detected EI were located on the aortic valve in 8 cases, mitral valve in 4, tricuspid valve in 2, and both mitral and aortic valves in 1 patient.
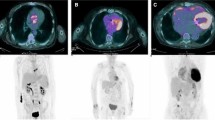
Representative median short-axis (SA) and long-axis (LA) FDG-PET slices through the IE area (red arrows) for patients in whom diagnostic confidence was enhanced by the 2nd PET. First and 2nd PET exams are displayed in grey scales, together with fused FDG-PET/CT LA slices (color/gray scales), in the 6 patients for whom IE detection was considered enhanced (i.e., leading to increased diagnostic confidence between the 1st and 2nd PET). Image scaling is given on the right side of the figure
Myocardial suppression of FDG uptake was deemed incomplete on the 1st PET in 9 patients (MS− group) and complete in 8 (MS+ group). MS+ patients only exhibited an increase in mean blood SUV between the 1st and 2nd PET (Table 3). In contrast, MS− patients presented a decrease between the 1st and 2nd PET in myocardial SUV max (6.05 ± 3.25 vs 4.32 ± 3.47, P = .021) and in myocardial SUV mean (3.10 ± 1.95 vs 2.42 ± 2.19, P = 0.038), associated with a trend of an increased EI/myocardium SUV max ratio (Table 3).
Finally, the observers considered that: (1) the myocardial FDG uptake was complete or almost complete in 4 MS− patients (patients # 1, 2, 3 and 6 in Figure 2) and (2) IE detection was enhanced between the 1st and 2nd PET (i.e., confirming a potential or probably visual IE focus as a definitive IE focus) in 6 MS− (67%) and in none of the MS+ patients. Representative PET/CT images of these 6 MS− patients are displayed in Figure 2, including the 2 cases where IE could only be visualized on the 2nd PET (patients # 1 and 2). Diagnostic confidence was not enhanced by the 2nd PET of 3 MS− patients: 2 with unchanged suppression of the myocardial FDG uptake on the 2nd PET, and one with no detectable IE foci on both PET despite an enhanced suppression on the 2nd PET. PET/CT images of representative patients for whom the diagnostic confidence was not enhanced on the 2nd PET are shown in Figure 3.
Representative median short-axis (SA) and long-axis (LA) FDG-PET slices through the IE area (red arrows) for patients in whom diagnostic confidence was not enhanced by the 2nd PET, i.e., two patients (# 1 and # 2) where IE was detected on the 1st PET and two further patients (# 3 and # 4) where IE was not detected on either the 1st or 2nd PET, patient # 3 showed a decrease in myocardial uptake on the 2nd PET but patient # 4 did not
Discussion
The current study shows that the suppression of myocardial uptake and the detection of IE may be enhanced when FDG-PET is repeated on the next day while maintaining patients on a ketogenic diet.
This observation may be explained by an increase in ketogenic metabolism (an increase in plasma beta-hydroxybutyrate), at the expense of glycolytic metabolism (decreased insulinemia). This potentially lowers the membrane density of the insulin-sensitive GLUT4 membrane receptor, which transports glucose and FDG molecules into the myocytes.9,13
In contrast, no change in myocardial FDG uptake was observed on the 2nd PET of patients for whom myocardial uptake suppression was already complete on the conventional 1st PET. These latter patients only exhibited an increase in blood activity on the 2nd PET (Table 2), which may potentially be linked to further decreases in cells’ glycolytic metabolism and thus, in glucose extraction from blood.
This two-step protocol may thus only be clinically useful in a small proportion of patients having undergone a conventional fast-based FDG-PET for IE diagnosis, when myocardial uptake suppression is not only incomplete but also, when it does not allow adequate analysis of all cardiac or peri-prosthetic areas of interest. The 2nd PET was required to achieve an IE diagnosis and was therefore definitely useful in only 2 patients (patients # 1 and 2 Figure 2).
Our study patients, who had been referred for a whole-body FDG-PET infectious endocarditis workup, were rather old (73 years on average), severely ill and in precarious medical condition. They frequently suffered from anorexia and were all on intravenous antibiotic treatments. This may explain why the two-step FDG-PET protocol was not always well-tolerated, i.e., 4 patients decided to take sweet food or received sugar in their intravenous perfusion and were thus excluded before the 2nd PET. Two additional patients withdrew their consent just after the 1st PET, and one patient died before the 1st PET.
Future studies will be required to confirm the FDG-PET differences observed using our two-step protocol as opposed to the one-step protocol, with a single FDG-PET preceded by several days of a very low-carbohydrate diet. Although long metabolic preparations have been successfully tested in cardiac sarcoidosis patients,11 these protocols are not appropriate for IE patients in precarious medical condition and often anorexic. It is likely that this diet would be better supported in less severely ill patients showing a low to intermediate pre-test likelihood of IE, compared to our patients with definite IE and who had been referred for a whole-body FDG-PET infectious endocarditis workup (i.e., to detect additional infectious sites2).
When compared with previously published studies involving comparable diet preparations,14,15,16 the myocardial SUVmax of our population was generally rather high, even when only considering the MS+ group (see Table 2). This observation likely relates to the particular characteristics of our study patients, who were rather old (73 ± 16 years) and often had a history of cardiac interventions (71% had a valve prothesis), given the fact that SUVmax may be significantly increased in vascular atherosclerosis and peri-prosthetic areas.3,15 Myocardial SUVmean, which is much less affected by small abnormal areas than SUV max, was in contrast very low in the MS+ group (close to blood SUVmean, see Table 2). Myocardial SUVmean also exhibited a marked decrease on the 2nd PET of the MS− patients, thereby explaining the improvement in diagnostic confidence in this group.
This pilot study, therefore, shows that when a myocardial FDG uptake persists after a conventional fast-based metabolic preparation, IE detection may be enhanced on an FDG-PET repeated the next day while maintaining patients on a ketogenic diet between the two scans. This two-step PET protocol needs to be confirmed in a much larger scale and more specifically in patients with an ambiguous IE diagnosis after a conventional fast-based FDG-PET.
New Knowledge Gained
In patients for whom the FDG-PET detection of IE is difficult due to the persistence of myocardial FDG uptake, IE detection may be enhanced on a repeat FDG-PET the next day while maintaining patients on a ketogenic diet between the two PET scans.
Abbreviations
- CT:
-
Computed tomography
- FDG:
-
18F-Fluorodesoxyglucose
- IE:
-
Infective endocarditis
- LV:
-
Left ventricle
- MS:
-
Myocardial suppression
- OSEM:
-
Ordered subset expectation maximization
- PET:
-
Positron emission tomography
- SD:
-
Standard deviation
- SUV:
-
Standardized uptake value
- VOI:
-
Volume of interest
References
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015;36:3075‐128.
Duval X, Le Moing V, Tubiana S, Esposito-Farèse M, Ilic-Habensus E, Leclercq F, et al. Impact of systematic whole-body 18F-fluorodeoxyglucose PET/CT on the management of patients suspected of infective endocarditis: The prospective multicenter TEPvENDO Study. Clin Infect Dis 2021;73:393‐403.
Erba PA, Lancellotti P, Vilacosta I, Gaemperli O, Rouzet F, Hacker M, et al. Recommendations on nuclear and multimodality imaging in IE and CIED infections. Eur J Nucl Med Mol Imaging 2018;45:1795‐815.
Dorbala S, Di Carli MF, Delbeke D, Abbara S, DePuey EG, Dilsizian V, et al. SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 10. J Nucl Med 2013;54:1485‐507.
Boursier C, Duval X, Bourdon A, Imbert L, Mahida B, Chevalier E, et al. ECG-gated cardiac FDG PET acquisitions significantly improve detectability of infective endocarditis. JACC Cardiovasc Imaging 2020;13:2691‐3.
Chareonthaitawee P, Beanlands RS, Chen W, Dorbala S, Miller EJ, Murthy VL, et al. Joint SNMMI–ASNC expert consensus document on the role of 18 F-FDG PET/CT in cardiac sarcoid detection and therapy monitoring. J Nucl Med 2017;58:1341‐53.
Atterton-Evans V, Turner J, Vivanti A, Robertson T. Variances of dietary preparation for suppression of physiological 18F-FDG myocardial uptake in the presence of cardiac sarcoidosis: A systematic review. J Nucl Cardiol 2020;27:481‐9.
Lu Y, Grant C, Xie K, Sweiss NJ. Suppression of myocardial 18F-FDG uptake through prolonged high-fat, high-protein, and very-low-carbohydrate diet before FDG-PET/CT for evaluation of patients with suspected cardiac sarcoidosis. Clin Nucl Med 2017;42:88‐94.
Larson SR, Pieper JA, Hulten EA, Ficaro EP, Corbett JR, Murthy VL, et al. Characterization of a highly effective preparation for suppression of myocardial glucose utilization. J Nucl Cardiol 2020;27:849‐61.
Clément A, Boutley H, Poussier S, Pierson J, Lhuillier M, Kolodziej A, et al. A 1-week extension of a ketogenic diet provides a further decrease in myocardial 18F-FDG uptake and a high detectability of myocarditis with FDG-PET. J Nucl Cardiol 2020;27:612‐8.
Özütemiz C, Koksel Y, Froelich JW, Rubin N, Bhargava M, Roukoz H, et al. Comparison of the effect of three different dietary modifications on myocardial suppression in 18 F-FDG PET/CT evaluation of patients for suspected cardiac sarcoidosis. J Nucl Med 2021;62:1759‐67.
Salvadori J, Odille F, Verger A, Olivier P, Karcher G, Marie P-Y, et al. Head-to-head comparison between digital and analog PET of human and phantom images when optimized for maximizing the signal-to-noise ratio from small lesions. EJNMMI Phys 2020;7:11.
Kong E. F-18 fluorodeoxyglucose positron emission tomography/computed tomography in the infection of heart. Yeungnam Univ J Med 2021;38:95‐106.
Williams G, Kolodny GM. Suppression of myocardial 18 F-FDG uptake by preparing patients with a high-fat, low-carbohydrate diet. Am J Roentgenol 2008;190:W151‐6.
Harisankar CNB, Mittal BR, Agrawal KL, Abrar ML, Bhattacharya A. Utility of high fat and low carbohydrate diet in suppressing myocardial FDG uptake. J Nucl Cardiol 2011;18:926‐36.
Cheng VY, Slomka PJ, Ahlen M, Thomson LEJ, Waxman AD, Berman DS. Impact of carbohydrate restriction with and without fatty acid loading on myocardial 18F-FDG uptake during PET: A randomized controlled trial. J Nucl Cardiol 2010;17:286‐91.
Acknowledgements
The authors wish to thank Dr. Petra Neufing for critical review of the manuscript, as well as the University Hospital of Nancy and the Nancyclotep Imaging Platform for providing funding.
Disclosures
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Germaini, M., Boursier, C., Goehringer, F. et al. The detection of infectious endocarditis may be enhanced by a repeat FDG-PET while maintaining patients on a ketogenic diet. J. Nucl. Cardiol. 29, 3256–3262 (2022). https://doi.org/10.1007/s12350-022-02921-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-022-02921-w