Abstract
Background
The aim of this study was to investigate the correlation of coronary flow reserve (CFR) assessed by rest/stress myocardial perfusion imaging with dynamic single-photon emission computed tomography (SPECT) with intracoronary pressure-derived fractional flow reserve (FFR) in patients with single-vessel coronary artery disease (CAD).
Methods
Patients with suspected or known stable CAD who were referred for invasive coronary angiography were prospectively enrolled. Both invasive FFR and SPECT were performed in subjects with single-vessel intermediate coronary stenosis. A cutoff value of < 0.8 was used to define abnormal FFR.
Results
A total of 34 patients were enrolled. The mean age of the subjects was 62.1 ± 6.7 years, and 79.4% were male. SPECT-derived CFR showed a significantly moderate correlation with FFR (r = 0.505, P = .003). The diagnostic performance for the identification of abnormal FFR in terms of sensitivity, specificity, and accuracy was 88.9%, 83.3%, and 87.9%, respectively, for CFR, with an optimized cutoff value of 1.73.
Conclusion
In patients with single-vessel CAD, SPECT CFR was useful for the detection of functionally significant stenosis. Our data support the use of this technique as an optional method for hemodynamic assessment, especially when FFR results are in normal range.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The hemodynamic assessment of coronary lesions, especially intermediate coronary artery stenosis, has become increasingly important in patients with stable coronary artery disease (CAD). There is accumulating evidence that the functional significance of coronary stenosis determines the potential benefit of the revascularization procedure.1 Fractional flow reserve (FFR), which is the distal-to-proximal pressure ratio across a coronary stenosis, typically measured by a pressure guidewire during invasive coronary angiography (CAG), is considered the gold-standard method for defining hemodynamically significant coronary stenosis.2 Although FFR-guided revascularization is associated with improved clinical outcomes and is strongly recommended by the established guidelines,3 FFR remains substantially underused for a variety of practical reasons, such as its invasive nature and high costs.
To overcome these limitations, the quantification of coronary flow reserve (CFR) using noninvasive imaging techniques has emerged as an attractive tool in assessing assessment of the functional significance of angiographic coronary stenosis when evaluating the efficacy of therapeutic intervention.4,5 Single-photon emission computed tomography (SPECT) myocardial perfusion imaging with technetium-99m-labeled (99mTc)-perfusion agents is a well-established modality for the screening and characterization of myocardial ischemia.6 However, SPECT perfusion quantitation was extremely challenging because of the difficulty in achieving dynamic acquisitions with classic Anger cameras. With the advent of cardiac cameras equipped with cadmium-zinc-telluride (CZT) detectors, allowing list-mode recording and multiframe dynamic reconstructions with high sensitivity and resolution, the measurement of CFR with SPECT has been made feasible.7 Although CFR derived from dynamic SPECT was recently compared to invasive angiographic findings in patients with multivessel coronary disease, showing that global and regional CFR was strongly correlated with the anatomic extent and severity of CAD and the FFR measurements,8,9 the agreement between SPECT-based CFR and invasive FFR in the evaluation of intermediate coronary artery stenosis in patients with single-vessel CAD is still unknown. The DEFER study has shown that patients with single-vessel stenosis with an FFR > 0.75 who did not undergo percutaneous coronary intervention (PCI) had excellent outcomes.10 In these patients, the possibility that chest pain/discomfort may be more related to microvascular dysfunction rather than macrovascular disease and cardiac SPECT is of special interest as it permits simultaneous assessment of microvascular status.
In the present study, we sought to investigate the relation between CFR quantification by dynamic 99mTc-perfusion SPECT and invasive FFR and the additional diagnostic insights provided by dynamic SPECT to the visual evaluation in the assessment of the severity of intermediate single-vessel disease.
Materials and Methods
Patient Population
A total of 236 patients with suspected or known stable CAD who were referred for invasive CAG were prospectively enrolled between June 2018 and April 2019 at Zhongshan Hospital, Fudan University. All patients received invasive CAG. Seventy-eight patients underwent FFR evaluation for lesions thought to be of intermediate severity at the time of invasive CAG. One hundred and twenty-one patients underwent a 99mTc-sestamibi (MIBI) SPECT imaging within 3 days before or after invasive CAG. No revascularization was performed between SPECT imaging and CAG. Among these patients, patients with intermediate single-vessel lesions who underwent both FFR and SPECT were enrolled for further analysis. The exclusion criteria were as follows1: ≥ 50% stenosis of ≥ 2 coronary arteries at invasive CAG,2 stenosis of the left main coronary artery,3 revascularization in the time between FFR and SPECT,4 previous myocardial infarction,5 nonischemic cardiomyopathy,6 previous PCI or coronary artery bypass grafting (CABG), and7 left ventricular ejection fraction < 35%. The study protocol was approved by the local ethics committee, and informed consent was obtained from all patients.
Dynamic Perfusion SPECT Imaging and Analysis
SPECT imaging was performed using a single-day rest/stress imaging protocol as previously published,11 and image acquisition was achieved with a D-SPECT cardiac scanner (Spectrum Dynamics, Caesarea, Israel) equipped with nine individual CZT detector columns. During the dynamic scanning process, the detectors performed a continuous step and shoot scanning pattern consisting of multiple sweeps forwards and backwards. Each sweep comprised ten positions over approximately 3 seconds.
For rest imaging, prescanning was performed after the administration of an initial dose of approximately 1 mCi MIBI to enable positioning of the heart in the center of the field of view and establishment of the scanning region of interest (ROI). Full scanning was started immediately after the injection of the remaining dose of approximately 15 mCi MIBI, and dynamic images were acquired in list mode for over 6 minutes. Following the rest dynamic scanning, rest perfusion scanning was performed. For stress imaging, pharmacological stress was induced with an intravenous infusion of adenosine triphosphate (ATP) disodium at a rate of 140 μg·kg−1·min−1 for 5 minutes, and 25 mCi MIBI was injected 3 minutes later from the start of ATP injection, followed by dynamic image acquisition for over 6 minutes. After that, stress perfusion scanning was acquired. The workflow for dynamic perfusion SPECT imaging is illustrated in Fig. 1.
For the dynamic perfusion analysis, rest and stress dynamic images were reformatted and reconstructed into 32 time frames (21 × 3, 1 × 9, 1 × 15, 1 × 21, 1 × 27, and 7 × 30 seconds). The reconstruction was based on an ordered subset expectation maximization algorithm with four iterations and 32 subsets. All analyses of dynamic images and corresponding perfusion values were performed using Corridor 4DM software (INVIA, Ann Arbor, MI, USA). Residual activity from the rest injection was corrected using the early images (30-second frames) prior to the first pass of the tracer bolus. Residual correction was achieved by calculating the mean pre-injection activity in each sampled region and subtracting it from that region’s time activity curve. The left ventricular (LV) endocardial and epicardial surfaces were algorithmically estimated from summed myocardial images beyond the 2-minute mark. Manual motion correction was applied on the dynamic sequences as necessary. A midwall surface, determined equally distant between the endocardial and epicardial surfaces, was sampled at the center of each polarmap sector across all time frames to produce global and regional LV myocardial tissue time activity curves (TAC). A box-shaped ROI sampled LV blood pool centered at the basal valve plane across all time frames to produce the LV blood TAC. Myocardial blood flow (MBF) was extrapolated from uptake rate K1 using the previously established Renkin–Crone equation for MIBI.12 CFR was then calculated as the ratio of the stress MBF to the rest MBF. The global myocardial ROI was divided into 3 regional ROIs corresponding to coronary territories (left anterior descending coronary artery, right coronary artery, and left circumflex coronary artery), and each regional CFR was also calculated. Images were analyzed by two experienced nuclear physicians who were blinded to the CAG and FFR results.
Invasive Coronary Angiography with Fractional Flow Reserve
Invasive CAG was performed according to standard clinical protocols. Intermediate stenosis was defined as 40%-70% diameter stenosis by visual assessment. Before invasive FFR measurements, all patients received 5000 IU of intravenous heparin and intracoronary nitroglycerin. A 0.014-inch coronary pressure wire (Pressure Wire X; Abbott Vascular, Santa Clara, CA) was calibrated outside the body and then equalized to the guiding catheter pressure with the sensor positioned just outside the ostium of the guiding catheter. The wire was then advanced to the distal portion of the study lesion. Distal coronary pressure (Pd) and aortic pressure (Pa) were recorded at baseline and at maximal hyperemia. Maximal hyperemia was induced through intravenous administration of ATP using the same protocol as applied during SPECT imaging. FFR was calculated as the mean Pd divided by the mean Pa during maximal hyperemia. After all recordings, a subsequent measure of the FFR value at the aorta site was conducted to routinely check that drift did not occur. If the value was beyond the range of 0.97-1.03, the FFR measurement was repeated. FFR values < 0.8 were considered positive for ischemia.
Statistical Analysis
The qualitative data were described as numbers and percentages. The quantitative data are reported as the mean ± standard deviation and were tested by Student’s t test. All tests were two-tailed, and a P value < .05 was considered to be statistically significant. Linear regression analysis was used to clarify the relationship between CFR and FFR. A receiver operating characteristic (ROC) curve analysis was performed by using easyROC version 1.3 to evaluate the accuracy of MPR in the detection of functionally significant stenosis defined by FFR. Statistical analyses were performed with SAS software (SAS Institute Inc., Cary, NC), version 9.3.
Results
Patient Characteristics
The baseline clinical data of the patients are summarized in Table 1. A total of 34 patients with intermediate single-vessel CAD were included. One case was excluded from further analysis because of poor image quality. The mean age of the patients was 62.1 ± 6.7 years, 27 (79.4%) were male, and the mean body mass index was 24.6 ± 2.5 kg·m−2. Only 4 patients (11.8%) had typical effort angina. With regard to coronary risk factors, 19 patients (55.9%) had hypertension, 7 (20.6%) had dyslipidemia, 6 (17.6%) had diabetes mellitus, 11 (32.4%) were current smokers, and 2 (5.9%) had a familial history of premature CAD.
SPECT, CAG, and FFR Data
The hemodynamic parameters during the rest and stress SPECT procedure and the global and regional MBF and CFR estimates resulting from the processing of the dynamic SPECT images are detailed in Table 2. The baseline heart rate and blood pressure were significantly increased and decreased, respectively, during ATP administration. ATP infusion was well tolerated in all patients, and no complications during the procedure were reported. Pharmacological stress significantly increased global MBF and regional MBF of both stenotic and nonstenotic arteries. As expected, the regional CFR of the stenotic vessels was lower than that of the nonstenotic vessels, although the difference was not statistically significant (2.12 ± 0.53 vs 2.19 ± 0.68, P = .535). However, an interesting finding was that there was a trend towards higher MBF in coronary arteries with stenosis than in vessels without stenosis at both rest and stress. The reasons may be related to the fact that the coronary artery with the most stenosis was the left anterior descending artery (LAD), which supplies the largest territory of epicardial coronary arteries.
Table 3 shows the quantitative coronary angiographic and FFR findings. The LAD was the most commonly affected vessel (75.8%), followed by the right coronary artery (RCA), 15.1%, and 3 patients (9.1%) had circumflex artery involvement. The mean stenosis by quantitative coronary arteriography of all patients was 55.8 ± 7.3%, and the mean FFR was 0.85 ± 0.08. There were no cardiac events between the time of dynamic SPECT imaging and the date of CAG.
Correlation of CFR with FFR in Single-Vessel CAD
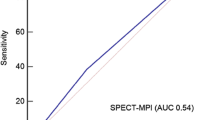
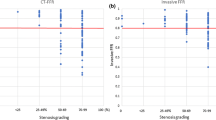
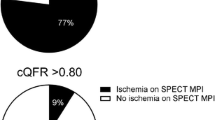
As depicted in Fig. 2, regional CFR was significantly positively correlated with FFR value (r = 0.505, P = .003). Patients with FFR < 0.8 (n = 6) had significantly lower corresponding regional CFR (1.62 ± 0.32 vs 2.22 ± 0.49, P = .008), when compared with those with FFR ≥ 0.8. The area under the ROC curve of CFR for the diagnosis of abnormal FFR was 0.864 (P < .001), which was larger than that for stress MBF (0.673, P = .034) and diameter stenosis (0.432, P = .431). The diagnostic performance in terms of sensitivity, specificity, and accuracy was, respectively, 88.9%, 83.3%, and 87.9% for SPECT-derived CFR with a ROC-optimized cutoff value of 1.73. Discrepancies between FFR and SPECT-derived regional CFR were found in 4 patients. All of these patients have normal FFR but low regional CFR value corresponded to the coronary territories.
Discussion
In the present study, we performed a prospective trial to examine the diagnostic performance of dynamic cardiac SPECT for functional significance in patients with single-vessel CAD and intermediate stenosis severity using invasive FFR as the reference standard. The main findings of our study are as follows1: regional SPECT-derived CFR was moderately correlated with FFR, which reflects the functional significance of coronary stenosis; and2 CFR exhibited much better diagnostic value than stress MBF in defining significant hemodynamic coronary stenosis.
Noninvasive CFR equals the ratio of absolute coronary flow or myocardial perfusion between hyperemia and rest and can be accomplished using a range of technologies.13,14,–15 Previous studies exploring the quantification of CFR with conventional SPECT systems documented the limitations of gamma cameras for the dynamic collection of data.16 With dedicated cardiac CZT cameras, dynamic SPECT offers great promise for MBF and CFR quantification, although 99mTc-labeled tracers are not ideal flow agents, and their myocardial uptake is low at high flow rates.17 The feasibility of CFR quantitation using CZT-SPECT has been validated by a variety of studies, although the absence of attenuation correction in CZT-SPECT could results in overestimation of MBF compared to positron emission tomography (PET),14 which is considered the gold standard for noninvasive assessment of MBF. In our study, the difference in the AUC of CFR and stress MBF values could be partially attributed to missing attenuation correction. Developed as a relative CFR, invasive FFR practically equals the ratio of distal coronary to aortic pressure during hyperemia and is documented to be the gold standard for relative CFR measurement. FFR-guided revascularization, which has been demonstrated to be associated with a better outcome compared with revascularization based on angiographic stenosis severity alone, is given the highest recommendation in the guidelines. In patients with multivessel coronary disease, global SPECT CFR has been shown to significantly negatively correlate with the severity of coronary lesions assessed by the Gensini score on invasive angiographic findings,18 and the diagnostic accuracy of regional SPECT CFR for the detection of functionally significant stenosis confirmed by FFR was 85%.8 In our study, we focused on patients with single-vessel CAD. Compared with multivessel CAD, there would be more variability in the correlation between FFR and CFR in patients with single-vessel CAD. The major factor that may contribute to the variability in the correlation may be the presence of visible or invisible coronary collateral circulation. The presence of coronary collateral circulation can cause the overestimation of CFR, especially in patients with single-vessel CAD.19 There is evidence that collateral blood flow is much more augmented in response to stress in patients with nonstenotic donor coronary arteries than in patients with stenosed donor coronary arteries.20 This may partially explain why the correlation between FFR and CFR was weaker in our study than that reported in studies of multivessel CAD patients.
In patients with intermediate coronary stenosis, the CFR may be more considerably affected by the state of microcirculation than by the collateral circulation.21 CFR is an assessment of coronary vasomotor dysfunction determined as a result of the complex interaction of epicardial stenosis and microvascular resistance on myocardial tissue perfusion at hyperemia. In contrast to hemodynamically significant stenosis of the epicardial coronary artery, which results in a decrease in both FFR and CFR, the impairment of microcirculation, which leads to increased microvascular resistance, diminishes CFR but does not affect (or even increase) FFR.22 Therefore, based on the range of microvascular function, discordance between FFR and CFR can be expected in intermediate coronary lesions.23,24 In the present study, discordance between FFR and CFR was observed in 12% of patients. All of these patients displayed preserved FFR but considerable impairments in both global and regional CFR. It has been suggested that preserved FFR and low CFR are associated with microvascular disorders and increased microvascular resistance.25 Different from focal epicardial stenosis in patients with single-vessel CAD, microvascular dysfunction is predominantly diffused through the myocardial tissue and causes decreased CFR of all coronary territories. Here, we found that although there was a trend toward lower CFR value of stenotic coronary arteries than that of nonstenotic vessels, the difference was not significant between the two groups, which could be partially attributed to the possible presence of microvascular dysfunction. Furthermore, CFR is thought to have a significant advantage over FFR in the prediction of prognosis in some studies. It has been shown that similar to patients with diminished FFR, those with preserved FFR but impaired CFR also have a higher incidence of adverse cardiac outcomes compared with those with preserved FFR and CFR.26,27 Therefore, in patients with intermediate coronary lesions, an additional SPECT CFR measurement should be helpful in making clinical decisions, especially when the FFR result is in the normal range.
Limitations
There are several limitations that need to be considered when interpreting our results. First, this study is based on a relatively small number of patients, although a significant correlation was found between invasive FFR and SPECT-derived CFR. With our sample size, it was not possible to perform subanalyses in specific patients, such as those with normal FFR but abnormal CFR. Second, the study patients were dominantly male and had relatively low body mass index. Heterogeneous attenuation effects in large individuals may complicate evaluation. Third, stenosis of the LAD accounted for over 70% of the intermediate coronary artery stenosis in the trial and resting MBF was not adjusted to compensate for physiological variance, both of which may cause potential bias. Fourth, myocardial perfusion PET, which is considered to be the gold standard of noninvasive CFR, was not performed to validate the method of dynamic SPECT, even though good correlation has been verified between PET and SPECT CFR measurements. Finally, the prognostic value of SPECT-derived CFR was not investigated, particularly in patients with discrepant SPECT and FFR findings. Further studies with larger samples and long-term follow-up are needed.
Conclusion
In summary, the high diagnostic accuracy of SPECT CFR for the detection of functionally significant stenosis supports the use of this technique as an optional method for hemodynamic assessment in patients with single-vessel CAD. In patients with discrepancies between FFR and CFR, an abnormal CFR may indicate microvascular dysfunction, which calls for further investigations.
New Knowledge Gained
In patients with single-vessel CAD and intermediate stenosis severity, SPECT-derived CFR showed a significantly correlation with FFR and was a reliable noninvasive method for hemodynamic assessment.
Abbreviations
- CFR:
-
Coronary flow reserve
- FFR:
-
Fractional flow reserve
- CAD:
-
Coronary artery disease
- PCI:
-
Percutaneous coronary intervention
- MBF:
-
Myocardial blood flow
- CAG:
-
Coronary angiography
- CZT:
-
Cadmium-zinc-telluride
- ROI:
-
Region of interest
- ATP:
-
Adenosine triphosphate
- ROC:
-
Receiver operating characteristic
References
van Nunen LX, Zimmermann FM, Tonino PA, Barbato E, Baumbach A, Engstrom T, et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet 2015;386:1853–60.
Pijls NH, Sels JW. Functional measurement of coronary stenosis. J Am Coll Cardiol 2012;59:1045–57.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:44–122.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015;131:19–27.
Murthy VL, Lee BC, Sitek A, Naya M, Moody J, Polavarapu V, et al. Comparison and prognostic validation of multiple methods of quantification of myocardial blood flow with 82Rb PET. J Nucl Med 2014;55:1952–8.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11:171–85.
Ben-Haim S, Murthy VL, Breault C, Allie R, Sitek A, Roth N, et al. Quantification of myocardial perfusion reserve using dynamic SPECT imaging in humans: A feasibility study. J Nucl Med 2013;54:873–9.
Ben Bouallegue F, Roubille F, Lattuca B, Cung TT, Macia JC, Gervasoni R, et al. SPECT Myocardial perfusion reserve in patients with multivessel coronary disease: Correlation with angiographic findings and invasive fractional flow reserve measurements. J Nucl Med 2015;56:1712–7.
Miyagawa M, Nishiyama Y, Uetani T, Ogimoto A, Ikeda S, Ishimura H, et al. Estimation of myocardial flow reserve utilizing an ultrafast cardiac SPECT: Comparison with coronary angiography, fractional flow reserve, and the SYNTAX score. Int J Cardiol 2017;244:347–53.
Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van’t Veer M, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105–11.
Hesse B, Tagil K, Cuocolo A, Anagnostopoulos C, Bardies M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855–97.
Leppo JA, Meerdink DJ. Comparison of the myocardial uptake of a technetium-labeled isonitrile analogue and thallium. Circ Res 1989;65:632–9.
Han S, Kim YH, Ahn JM, Kang SJ, Oh JS, Shin E, et al. Feasibility of dynamic stress (201)Tl/rest (99m)Tc-tetrofosmin single photon emission computed tomography for quantification of myocardial perfusion reserve in patients with stable coronary artery disease. Eur J Nucl Med Mol Imaging 2018;45:2173–80.
Agostini D, Roule V, Nganoa C, Roth N, Baavour R, Parienti JJ, et al. First validation of myocardial flow reserve assessed by dynamic (99m)Tc-sestamibi CZT-SPECT camera: Head to head comparison with (15)O-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging 2018;45:1079–90.
Petretta M, Storto G, Pellegrino T, Bonaduce D, Cuocolo A. Quantitative assessment of myocardial blood flow with SPECT. Prog Cardiovasc Dis 2015;57:607–14.
Marini C, Giusti M, Armonino R, Ghigliotti G, Bezante G, Vera L, et al. Reduced coronary flow reserve in patients with primary hyperparathyroidism: A study by G-SPECT myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 2010;37:2256–63.
Acampa W, Assante R, Mannarino T, Zampella E, D’Antonio A, Buongiorno P, et al. Low-dose dynamic myocardial perfusion imaging by CZT-SPECT in the identification of obstructive coronary artery disease. Eur J Nucl Med Mol Imaging 2019;47:1705–12.
Iguchi N, Utanohara Y, Suzuki Y, Suzuki M, Hagiya K, Higuchi R, et al. Myocardial flow reserve derived by dynamic perfusion single-photon emission computed tomography reflects the severity of coronary atherosclerosis. Int J Cardiovasc Imaging 2018;34:1493–501.
van de Hoef TP, Nolte F, Rolandi MC, Piek JJ, van den Wijngaard JP, Spaan JA, et al. Coronary pressure-flow relations as basis for the understanding of coronary physiology. J Mol Cell Cardiol 2012;52:786–93.
Zbinden R, Zbinden S, Meier P, Hutter D, Billinger M, Wahl A, et al. Coronary collateral flow in response to endurance exercise training. Eur J Cardiovasc Prev Rehabil 2007;14:250–7.
Yong AS, Ho M, Shah MG, Ng MK, Fearon WF. Coronary microcirculatory resistance is independent of epicardial stenosis. Circ Cardiovasc Interv 2012;5(103-8):S1–2.
Taqueti VR, Di Carli MF. Clinical significance of noninvasive coronary flow reserve assessment in patients with ischemic heart disease. Curr Opin Cardiol 2016;31:662–9.
Meuwissen M, Chamuleau SA, Siebes M, Schotborgh CE, Koch KT, de Winter RJ, et al. Role of variability in microvascular resistance on fractional flow reserve and coronary blood flow velocity reserve in intermediate coronary lesions. Circulation 2001;103:184–7.
van de Hoef TP, Nolte F, EchavarrIa-Pinto M, van Lavieren MA, Damman P, Chamuleau SA, et al. Impact of hyperaemic microvascular resistance on fractional flow reserve measurements in patients with stable coronary artery disease: Insights from combined stenosis and microvascular resistance assessment. Heart 2014;100:951–9.
Ahn SG, Suh J, Hung OY, Lee HS, Bouchi YH, Zeng W, et al. Discordance between fractional flow reserve and coronary flow reserve: Insights from intracoronary imaging and physiological assessment. JACC Cardiovasc Interv 2017;10:999–1007.
Meuwissen M, Chamuleau SA, Siebes M, de Winter RJ, Koch KT, Dijksman LM, et al. The prognostic value of combined intracoronary pressure and blood flow velocity measurements after deferral of percutaneous coronary intervention. Catheter Cardiovasc Interv 2008;71:291–7.
van de Hoef TP, van Lavieren MA, Damman P, Delewi R, Piek MA, Chamuleau SA, et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv 2014;7:301–11.
Acknowledgement
This work was supported by grant from the National Natural Science Foundation of China (Nos. 81770429 and 81700312).
Disclosure
Chenguang Li, Rende Xu, Kang Yao, Jie Zhang, Shuguang Chen, Lifang Pang, Hao Lu, Yuxiang Dai, Juying Qian, Hongcheng Shi, and Junbo Ge have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, C., Xu, R., Yao, K. et al. Functional significance of intermediate coronary stenosis in patients with single-vessel coronary artery disease: A comparison of dynamic SPECT coronary flow reserve with intracoronary pressure-derived fractional flow reserve (FFR). J. Nucl. Cardiol. 29, 622–629 (2022). https://doi.org/10.1007/s12350-020-02293-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02293-z