Abstract
Background
Regadenoson is a selective adenosine receptor agonist. It is currently unclear if the level of hyperemia differs between stress agents. We compared Myocardial Blood Flow (MBF) and Myocardial Flow Reserve (MFR) response on CZT-SPECT Myocardial Perfusion Imaging (MPI) to evaluate if dipyridamole and regadenoson could induce the same level of hyperemia.
Methods
228 patients with dynamic CZT-SPECT MPI were retrospectively analyzed (66 patients stressed with regadenoson and 162 with dipyridamole) in terms of MBF and MFR. To rule out confounding factors, two groups of 41 patients were matched for clinical characteristics in a sub-analysis, excluding high cardiovascular risk patients.
Results
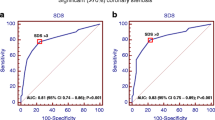
Overall stress MBF was higher in regadenoson patients (1.71 ± 0.73 vs. 1.44 ± 0.55 mL·min−1·g−1 for regadenoson and dipyridamole, respectively, p < .05). However, when confounding factors were ruled out, stress MBF (1.57 ± 0.56 vs. 1.61 ± 0.62 mL·min−1·g−1 for dipyridamole and regadenoson, respectively, p = .88) and MFR (2.62 ± 0.77 vs. 2.46 ± 0.76 for dipyridamole and regadenoson, respectively, p = .40) were not different between regadenoson and dipyridamole.
Conclusions
Our results suggest that dipyridamole and regadenoson induce equivalent hyperemia in dynamic SPECT with similar stress MBF and MFR in comparable patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
During Myocardial Perfusion Imaging (MPI), pharmacologically induced or exercise-induced stress normally increases blood flow to the myocardium while stress imaging is performed. The most common medications used in pharmacologically induced stress testing are vasodilators, which increase blood flow in the myocardium by stimulating adenosine receptors 1: adenosine, dipyridamole, and regadenoson. Because adenosine receptors are not specific of the myocardial tissue, non-cardiac adverse events may be observed. Up to 80% of patients will experience at least one adverse event or discomfort regardless of the vasodilator used.1,2,3 Depending on severity, this may require reversal by aminophylline injection.4
Regadenoson is a selective agonist of adenosine A2A receptors approved for clinical use by the FDA in 2008 and by the European Medicines Agency in 2010. Besides its simplicity of use with a single bolus injection needed to obtain the maximum of efficacy (conversely to dipyridamole and adenosine which require infusion of a weight adapted dose), the ADVANCE MPI 1 and 2 trials proved that regadenoson was equally effective regarding diagnostic and prognostic information and better tolerated in head to head comparisons in the general population.5,6,7,8,9
Regarding safety and tolerability, regadenoson has been tested in a several populations with favorable results because of its adenosine receptor subtype selectivity.10,11,12,13
Hence, regadenoson has now become the most commonly used vasodilator in the USA—where, based on 2013 data, It holds an 84% of the vasodilator market share 14—while its use is continuously expanding in Europe. For example, in Germany in 2018, a pharmacological stress test was performed in 49 % of SPECT MPI: 23 % used adenosine, 26 % used regadenoson, and less than 1% used dipyridamole or dobutamine.15 However, regadenoson is approximately 10 to 30 times more expensive than dipyridamole or adenosine.
Assessment of Myocardial Blood Flow (MBF) and Myocardial Flow Reserve (MFR) are used to explore coronary microcirculation function and provide additional information over qualitative parameters from conventional MPI for diagnosis and prognosis of Coronary Artery Disease (CAD).16 Quantification of MBF and MFR values is now technically feasible using dynamic CZT-SPECT MPI with 99mTc-tetrofosmin, with similar MFR compared to Positron Emission Tomography (PET).17,18,19,20 Stress MBF can quantify the level of hyperemia induced by pharmacological stress agents. Goudarzi et al showed no difference between regadenoson and dipyridamole in terms of stress MBF and MFR on a retrospective PET study including 104 subjects.21 Regarding tolerance, patients in the regadenoson group reported less severe symptoms and required less aminophylline. Bravo et al also found comparable results of stress MBF and MFR between regadenoson and dipyridamole in patients with hypertrophic cardiomyopathy.22 Johnson et al ,however, found that regadenoson (with the standard timing protocol) only achieved 80% of dipyridamole hyperemia (and 90% if delaying radiotracer injection) when performing 2 pharmacological stress on the same subjects.23
Since there are conflicting results regarding the performance of both regadenoson and dipyridamole agents to induce myocardial hyperemia we proposed to compare their performance using CZT-SPECT MPI in a retrospective study of patients with and without CAD referred for MPI.
Materials and Methods
Study Groups
We performed a bi-centric retrospective case control study. 242 patients were enrolled between June 2018 and February 2020. 14 were excluded for technical issues or missing data. Among the 228 remaining patients, hyperemia was achieved with regadenoson in 66 and with dipyridamole in 162 (Figure 1). Part of them were enrolled in the CFR-OR trial (clinicaltrials.gov unique identifier NCT03586492). Every patient received information and gave informed consent (written consent for the CFR-OR trial participants). The study protocol was approved by the Local and Regional Ethics Committees (CPP Ouest III) and the procedures were in accordance with the declaration of Helsinki. Inclusion criteria were as follow: patients at least 18 years or older, referred for MPI, with or without history of stable CAD, acute coronary syndrome, cardiomyopathy or other heart disease. Exclusion criteria included absolute common contraindication to vasodilators (severe hypotension, atrioventricular block 2nd or 3rd grade and recent infarction), pregnancy or active breastfeeding. Patients with specific dipyridamole contraindication (asthma, chronic obstructive pulmonary disease (COPD) or pulmonary arterial hypertension) were tested using regadenoson. Patients with a 50% stenosis or greater on at least one major coronary vessel (assessed by coronary angiography or coronary computed tomography angiography), elevated calcium score (> 400) or history of coronary stenting were considered CAD patients.
To avoid interfering effects of flow-limiting coronary artery stenosis, we performed a subgroup analysis including only low risk patients with no prior history of CAD, normal regional myocardial perfusion, left ventricular ejection fraction (LVEF) > 45% on MPI, known coronary calcium score < 400, absence of diabetes on insulin therapy, absence of severe renal disease (estimated glomerular filtration rate < 60 mL·min−1), and absence of any other significant systemic disease. Because of regadenoson cost, more procedures using dipyridamole are performed in our centers. The dipyridamole subgroup was selected to match the regadenoson subgroup for clinical variables including age, sex distribution, body mass index (BMI), cardiovascular risk factors including hypertension, active smoking, hyperlipidemia, and obesity.
The matching process was performed on an individual basis. Each subject who had received regadenoson was matched as closely as possible with a subject from the large available group of dipyridamole patients.
Tables 1 and 2 summarize the characteristics of both final patient’s groups.
SPECT Images Acquisition
All patients underwent a 1-day stress/rest protocol. They were asked to refrain from caffeine and methylxanthine-containing substances/drugs for at least 12 h and from beta blockers 48 h before their scans if asked by the cardiologist in accordance with European recommendations.24 SPECT data were acquired in list mode using the same Discovery NM530c cardiac CZT camera (General Electric Healthcare, Haifa, Israel) in both centers. For stress imaging, an initial dose of approximately 37 MBq of 99mTc-tetrofosmin was used to position the patient’s heart within the field of view. A pharmacological stress was then performed with an injection of regadenoson (400 μg) or with a dipyridamole perfusion (0.56 mg·kg−1),25 followed by the injection of 250 MBq of 99mTc-tetrofosmin, delivered by a rapid hand injection at hyperemia peak and flushed by 50 mL of saline to ensure consistent delivery of a tight bolus. 99mTc-tetrofosmin injection was performed 10-20 s after the bolus of regadenoson as mentioned in the package insert 26 or 4 min after the beginning of the dipyridamole perfusion. Three hours later, for rest imaging, a bolus of 500 MBq of 99mTc-tetrofosmin was injected using the same technique. Our procedure is summarized in Figure 2.
SPECT Images Analysis
All images were reconstructed using the following parameters: OSEM 2 iterations and 10 subsets, Butterworth filtering order 5, cutoff 0.5 cm−1. We did not apply attenuation correction and scatter correction.
MPI were visually assessed using a 17-segment model on a Xeleris workstation (General Electric Healthcare, Haifa, Israel). MPI was considered abnormal in case of reversible or irreversible defect extending on at least 1 segment out of 17, akinesia or transient left ventricular dilation.
Dynamic imaging data were analyzed using Corridor 4DM software (INVIA, Ann Arbor, MI, USA). SPECT data were re-binned into 20 frames consisting of 12 × 10-s and 8 × 30-s frames. Left ventricle (LV) endocardial and epicardial surfaces were algorithmically estimated from summed myocardial images beyond the 2-min mark. A midwall surface was divided into 460 polarmap sectors, where LV myocardial tissue Time Activity Curves (TACs) were nearest neighbor sampled at the center of each sector across all time frames. Global and regional TACs (Left Anterior Descending artery (LAD), Left Circumflex (LCx), Right Coronary Artery (RCA)) were averaged from the polarmap sector TACs. MFR analysis used blood sampling by averaging a 3D box-shaped Region Of Interest (ROI) within the LV/Left Atrium (LA) blood pool, localized in the LA in the short axis and centered at the basal valve plane along the long axis, across all time frames. The size of the ROI was two pixels wide in the short axis and 30 mm long in the long axis to sample both the LV and LA cavities.27 A net retention model proposed by Jeffrey Leppo 28 and Yoshida 29 was used to calculate the retention rate R according to the following equation:
In this equation, MBF is the myocardial blood flow, E is the extraction fraction, P(t) is the total myocardial tracer concentration or tissue TAC, Ca(t) is the arterial concentration of the tracer or blood TAC and PV is the partial volume value (set to 0.6). The Correction Factor (CF) for myocardial density was set to 1. Sm is the spillover from the blood pool activity to the myocardium estimated from compartmental analysis, and Sb is the spillover from the myocardium to the blood pool activity which can be set to 0 assuming the spillover is negligible. Integration limit t1 denotes the end of the blood pool phase, at 1 min, while t2 and t3 denote integration limits of the average tissue activity, typically from 1 min to 2 min. The integration limits are adjusted to the peak of the blood TAC. The extraction fraction from the retention equation (E) is based on the Renkin-Crone model used by Leppo,28 with parameters A = 0.874 and B = 0.443: \( E = \left( {1 - A \times e - \frac{B}{MBF}} \right) \)
Statistical Analysis
Continuous variables are presented as means ± standard deviation (SD). Gaussian distribution was assessed using D’Agostino-Pearson normality test. The Student’s t test for unpaired data was adopted for the global analysis and Mann-Whitney test was used when normality test wasn’t passed. Chi-square test was applied for categorical data. In the subgroup analysis continuous variables were compared with the paired student’s t test. Fischer test was used to compare nominal qualitative variables. Wilcoxon matched pairs signed rank test was used when normality test wasn’t passed. p < .05 was considered statistically significant. All analysis was performed using Prism 8.4.1.30
Results
Overall Analysis
228 patients were analyzed.162 patients underwent a dipyridamole stress test, and 66 patients a regadenoson stress test. These two groups were comparable regarding age, gender, BMI, cardiovascular risk factors except diabetes, and hemodynamic parameters (Table 1). There were significantly more diabetic patients in the dipyridamole group.
Global rest MBF was 0.63 ± 0.26 in the dipyridamole group and 0.70 ± 0.32 in the regadenoson group, with no statistical difference (p = .28). Stress MBF was lower with dipyridamole than with regadenoson, 1.44 ± 0.50 and 1.71 ± 0.73, respectively (p = .01). MFR was not significantly different between the dipyridamole and the regadenoson groups, 2.46 ± 0.87 and 2.64 ± 1.02 ,respectively (p = .36) (Table 1).
The two groups were comparable in terms of patients suffering from CAD. There was no significant difference in terms of stress MBF and MFR between dipyridamole and regadenoson in patients suffering from CAD (treated or not), but this result is subject to a small number of patients with CAD in the regadenoson group (n = 11). However, in patients with no evidence of CAD, there was still a higher stress MBF value in the regadenoson group (1.71 ± 0.66) than in the dipyridamole group (1.48 ± 0.51) similar to what was observed in the overall population (p = .03).
There was no significant correlation between hemodynamic parameters and stress MBF in both groups. In the dipyridamole group, stress MBF was not correlated either with RPP (r = .13; p = .69) or heart rate at peak (r = .49; p = .11). In the regadenoson group stress MBF was neither significantly correlated with RPP (r = .07; p = .82) nor with heart rate at peak (r = − .05; p = .89).
There was a little more pathological MPI in the dipyridamole group (2 out of 66 in the regadenoson group (3%) and 17 out of 162 in the dipyridamole group (10%)), but this difference wasn’t statistically significant (p = .11).
Matched patients without history of CAD
41 patients without prior history of CAD or high risk of CAD were analyzed. These two groups excluded diabetic patients and were comparable in terms of age, gender, BMI, cardiovascular risk factors and cardiovascular treatments at the time of evaluation.
There was no significant difference in terms of stress MBF (1.57 ± 0.56 for dipyridamole vs. 1.61 ± 0.62 for regadenoson; p = .88), rest MBF (0.65 ± 0.32 for dipyridamole vs. 0.71 ± 0.35 for regadenoson; p = .41) and MFR (2.62 ± 0.77 for dipyridamole vs 2.46 ± 0.76 for regadenoson; p = .40) (Table 2).
Discussion
Regadenoson is often used for its simple administration 31,32 and its high tolerability profile 33,34,35, while dipyridamole is favored for its better cost-effectiveness ratio, with comparable results for qualitative SPECT MPI.36,37,38,39
In our study, regadenoson stress test seemed to result in higher stress MBF values in our global population. However, there was no difference of quantitative MPI parameters such as stress MBF and MFR between dipyridamole and regadenoson in a subgroup of patients without prior history or high risk of CAD.
Quantitative effects of regadenoson have already been explored with different modalities. In a dog model, intravenous bolus injection of regadenoson caused a dose-dependent increase in MBF comparable to that produced by adenosine infusion.31 Another dog study showed similar data; regadenoson and adenosine caused a dose-dependent increase in MBF, with non-statistically different maximal values between the 2 drugs although regadenoson was 100 × more potent than adenosine.33 A Cardiovascular Magnetic Resonance (CMR) study conducted by Vasu et al on a small number of healthy patients with a crossover design found equivalent effects of regadenoson and adenosine on MBF and MFR both being superior to dipyridamole.40 DiBella et al showed in another crossover study with 30 patients using CMR, that regadenoson and adenosine produced the same vasodilation.41 In several coronary angiography flow measurements studies using invasive catheter-based fractional flow reserve, it has been shown that regadenoson could provoke an equivalent hyperemia compared to usual vasodilators.42,43,44 Goudarzi et al in a retrospective 82Rb-PET study, showed on 104 patients that MFR and stress MBF were equivalent when using dipyridamole or regadenoson.21 A crossover PET study with the same imaging modality showed that regadenoson achieved only 80% of dipyridamole hyperemia following the recommended timing sequence 26 maximized to 90% when delaying radiotracer injection.23
Altogether, these results are consistent with our findings. In our overall analysis stress MBF is higher when regadenoson is used. This difference could be explained by the higher number of diabetic patients in the dipyridamole group (p = .005). Many studies showed a higher prevalence of impaired MFR in patients with diabetes compared with those without diabetes.45,46 This might be explained because diabetic patients have more CAD but also more coronary microvascular dysfunction. In our study, patients suffering from CAD stressed with regadenoson tend to have similar stress MBF and MFR values than patients without CAD and have considerable variability. This might be due to a very small number of patients with previous CAD history stressed using regadenoson (n = 11), including both patients with revascularization procedures and optimal therapies and also patients with authentic ischemia, limiting its interpretation and explaining the higher variability compared to other results. However, patients with CAD stressed with dipyridamole (n = 27) seemed to have lower stress MBF and MFR results, when compared to patients without evidence of CAD. We reported a little more pathological MPI in the dipyridamole group, but this might be explained by the higher number of diabetic patients and of patients with previous history of CAD.
When adjusting on confounding factors, in the sub-analysis of patients with a low probability of CAD, we did not find any significant difference between stress MBF induced by regadenoson and dipyridamole. In this sub-population and because of their higher probability of reduced MFR as mentioned before, diabetic patients were excluded. Thus, our data suggest that regadenoson has similar performances to dipyridamole to achieve maximum coronary vasodilation. To our knowledge, the present study is the first to investigate the quantitative flow response to regadenoson in SPECT.
Our MFR values are in the same range as previous SPECT studies, with mean global MFR values of 2.18 ± 0.83, 2.44 ± 0.7 and 2.84 ± 0.81, respectively, for Giubbini et al19, Acampa et al20, and Agostini et al18. Our stress MBF values are consistent with those reported by Fang et al with mean stress MBF of 1.77 ± 0.4647, while results from previous works are quite heterogeneous. Some reported lower values, with stress MBF of 1.11 [Interquartile range (IQR), 1.00-1.26] for Nkoulou et al17 0.67 [IQR, 0.55-0.81] for Zavadovsky et al48 Other authors reported higher values, with stress MBF of 3.18 ± 0.95, 2.40 ± 0.7 and 2.3 ± 0.97 for Agostini et al18 Acampa et al20 and Giubbini et al19 These differences could be explained by a lack of standardization of flow measurement techniques leading to great a variability of stress MBF results. The variability being less significant for MFR results, as described with 82Rb-PET.49 Agostini et al for example used the same software but performed their acquisitions on a D-SPECT camera (Spectrum Dynamics Medical, Caesarea, Israel); Giubbini et al used the same camera and the same software, but applied motion correction that requires a manual contouring. In our study we chose not to apply motion correction as this is not an automatic tool and could be considered as an additional bias. Instead, we placed the vascular ROI box closer to the septum, to minimize the lateral wall motion effect.
Our protocol uses a dose of tracer of 250 MBq and 500 MBq for stress and rest acquisition, respectively, which is quite consistent with the previous dynamic SPECT studies: Giubbini et al injected 185 MBq and 370 MBq, respectively, at stress and rest 19; Acampa et al reported 155 MBq and 370 MBq, respectively, at stress and rest 20; however, Agostini et al injected 3 MBq·kg−1 at rest and 9 MBq·kg−1 at stress, like Nkoulou et al (330 MBq and 990 MBq for their injections), resulting in higher doses.17,18
We also chose not to apply attenuation correction (AC) because most of CZT-SPECT cameras are not equipped with computed tomography scanner, so it may not be routinely applicable. Furthermore, in our experience stress MBF values are lower with AC than without AC but MFR remains equivalent.50 Giubbini et al also reached the same conclusion in their study.19 Wells et al51, however, did not find significant differences between MBF and MFR with or without AC.
However, our study has some limitations that need to be acknowledged. First this was an observational and retrospective study. Second, the subgroup analysis was performed on patients referred for CAD screening, most of them having mild CAD risk and at least one cardiovascular risk factor which may have interfered with stress MBF. Third, side effects were not recorded in this study because of the large amount of previously published studies showing the great tolerability profile of regadenoson; although a recent study suggesting more frequent but less severe side effects induced by regadenoson challenged this general agreement.52 We just did not notice any major adverse event. Fourth, the small number of patients in each group strongly limits the conclusion of our study.
In addition, due to dipyridamole contraindications we might have more COPD patients in the regadenoson group. A meta-analysis showed that COPD patients have a 2-3 fold increased risk of cardiovascular disease compared to age-matched controls when adjusted for cigarette smoking,53 but as those potential COPD patients are in the regadenoson group, this might not interfere as we reported higher values of stress MBF in the regadenoson group. Moreover, we did not perform any correction of hemodynamic parameters as they were not significantly different between the two groups. Finally, though it could be considered as the gold standard, we did not compare our results to PET because PET MFR remains of high cost and difficult access in our country.
New knowledge gained
MPI quantitative parameters (stress MBF and MFR) are comparable whether pharmacological stress is performed using regadenoson or dipyridamole in low risk patients.
Conclusion
In this retrospective study, regadenoson stress test seemed to result in higher stress MBF values in our general population of patients referred for MPI. However, dipyridamole and regadenoson induced equivalent hyperemia with similar stress MBF and MFR in a subgroup of low CAD risk patients. Confirming these results in a larger prospective and randomized trial is warranted.
Abbreviations
- CAD:
-
Coronary artery disease
- LAD:
-
Left anterior descending artery
- LA:
-
Left atrium
- LCx:
-
Left circumflex
- LVEF:
-
Left ventricular ejection fraction
- MBF:
-
Myocardial blood flow
- MFR:
-
Myocardial flow reserve
- MPI:
-
Myocardial perfusion imaging
- RCA:
-
Right coronary artery
- ROI:
-
Region of interest
References
Johnson SG, Peters S. Advances in pharmacologic stress agents: Focus on regadenoson. J Nucl Med Technol 2010;38:163-71.
Leaker BR, O’Connor B, Hansel TT, Barnes PJ, Meng L, Mathur VS, et al. Safety of regadenoson, an adenosine A2A receptor agonist for myocardial perfusion imaging, in mild asthma and moderate asthma patients: A randomized, double-blind, placebo-controlled trial. J Nucl Cardiol 2008;15:329-36.
Page RL, Spurck P, Bainbridge JL, Michalek J, Quaife RA. Seizures associated with regadenoson: A case series. J Nucl Cardiol 2012;19:389-91.
Druz RS. Current advances in vasodilator pharmacological stress perfusion imaging. Semin Nucl Med 2009;39:204-9.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 2007;14:645-58.
Mahmarian JJ, Cerqueira MD, Iskandrian AE, Bateman TM, Thomas GS, Hendel RC, et al. Regadenoson induces comparable left ventricular perfusion defects as adenosine: A quantitative analysis from the ADVANCE MPI 2 trial. JACC Cardiovasc Imaging 2009;2:959-68.
Mahmarian JJ, Peterson LE, Xu J, Cerqueira MD, Iskandrian AE, Bateman TM, et al. Regadenoson provides perfusion results comparable to adenosine in heterogeneous patient populations: A quantitative analysis from the ADVANCE MPI trials. J Nucl Cardiol 2015;22:248-61.
Cerqueira MD, Nguyen P, Staehr P, Underwood SR, Iskandrian AE, ADVANCE-MPI Trial Investigators. Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging 2008;1:307-16.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, Raslan S, Heo J, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014-21.
Golzar Y, Doukky R. Regadenoson use in patients with chronic obstructive pulmonary disease: The state of current knowledge. Int J Chron Obstruct Pulmon Dis 2014;9:129-37.
Hussain N, Chaudhry W, Ahlberg AW, Amara RS, Elfar A, Parker MW, et al. An assessment of the safety, hemodynamic response, and diagnostic accuracy of commonly used vasodilator stressors in patients with severe aortic stenosis. J Nucl Cardiol 2017;24:1200-13.
Rai M, Ahlberg AW, Marwell J, Chaudhary W, Savino JA, Alter EL, et al. Safety of vasodilator stress myocardial perfusion imaging in patients with elevated cardiac biomarkers. J Nucl Cardiol 2017;24:724-34.
Gupta A, Bajaj NS. Regadenoson use for stress myocardial perfusion imaging in advance chronic kidney disease and dialysis: Safe, effective, and efficient. J Nucl Cardiol 2018;25:150-2.
American Society of Nuclear Cardiology. MedAxiom Nuclear Survey. J Nucl Cardiol 2014;21:5-88.
Lindner O, Burchert W, Buechel R, Schäfer WM, Im Namen der Arbeitsgemeinschaft „Kardiovaskuläre Nuklearmedizin“ der Deutschen Gesellschaft für Nuklearmedizin under AG20 „Nuklearkardiologische Diagnostik“ der Deutschen Gesellschaft für Kardiologie. Myocardial Perfusion SPECT 2018 in Germany: Results of the 8th Survey. Nukl Nucl Med 2019;58(6):425-33.
Camici PG, Rimoldi OE. The clinical value of myocardial blood flow measurement. J Nucl Med 2009;50:1076.
Nkoulou R, Fuchs TA, Pazhenkottil AP, Kuest SM, Ghadri JR, Stehli J, et al. Absolute myocardial blood flow and flow reserve assessed by gated SPECT with cadmium-zinc-telluride detectors using 99mTc-tetrofosmin: head-to-head comparison with 13 N-ammonia PET. J Nucl Med 2016;57:1887-92.
Agostini D, Roule V, Nganoa C, Roth N, Baavour R, Parienti J-J, et al. First validation of myocardial flow reserve assessed by dynamic 99mTc-sestamibi CZT-SPECT camera: Head to head comparison with 15O-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging 2018;45:1079-90.
Giubbini R, Bertoli M, Durmo R, Bonacina M, Peli A, Faggiano I, et al. Comparison between N13NH3-PET and 99mTc-Tetrofosmin-CZT SPECT in the evaluation of absolute myocardial blood flow and flow reserve. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01939-x.
Acampa W, Zampella E, Assante R, Genova A, De Simini G, Mannarino T, et al. Quantification of myocardial perfusion reserve by CZT-SPECT: A head to head comparison with 82Rubidium PET imaging. J Nucl Cardiol 2020. https://doi.org/10.1007/s12350-020-02129-w.
Goudarzi B, Fukushima K, Bravo P, Merrill J, Bengel FM. Comparison of the myocardial blood flow response to regadenoson and dipyridamole: A quantitative analysis in patients referred for clinical 82Rb myocardial perfusion PET. Eur J Nucl Med Mol Imaging 2011;38:1908-16.
Bravo PE, Pozios I, Pinheiro A, Merrill J, Tsui BMW, Wahl RL, et al. Comparison and effectiveness of regadenoson versus dipyridamole on stress electrocardiographic changes during positron emission tomography evaluation of patients with hypertrophic cardiomyopathy. Am J Cardiol 2012;110:1033-9.
Johnson NP, Gould KL. Regadenoson versus dipyridamole hyperemia for cardiac PET imaging. JACC Cardiovasc Imaging 2015;8:438-47.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging 2015;42:1929-40.
Iskandrian AS, Heo J, Askenase A, Segal BL, Auerbach N. Dipyridamole cardiac imaging. Am Heart J 1988;115:432-43.
lexiscan.pdf. [cited 2019 28]. https://www.astellas.us/docs/lexiscan.pdf.
Lortie M, Beanlands RSB, Yoshinaga K, Klein R, Dasilva JN, DeKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging 2007;34:1765-74.
Leppo JA, Meerdink DJ. Comparison of the myocardial uptake of a technetium-labeled isonitrile analogue and thallium. Circ Res 1989;65:632-9.
Yoshida K, Mullani N, Gould KL. Coronary flow and flow reserve by PET simplified for clinical applications using rubidium-82 or nitrogen-13-ammonia. J Nucl Med 1996;37:1701-12.
GraphPad Software, La Jolla California USA, www.graphpad.com.
Trochu J-N, Zhao G, Post H, Xu X, Belardinelli L, Belloni FL, et al. Selective A2A adenosine receptor agonist as a coronary vasodilator in conscious dogs: potential for use in myocardial perfusion imaging. J Cardiovasc Pharmacol 2003;41:132-9.
Hudgens S, Breeze J, Spalding J. Patient- and clinician-reported satisfaction with pharmacological stress agents for single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI). J Med Econ 2013;16:828-34.
Zhao G, Linke A, Xu X, Ochoa M, Belloni F, Belardinelli L, et al. Comparative profile of vasodilation by CVT-3146, ael A2A receptor agonist, and adenosine in conscious dogs. J Pharmacol Exp Ther 2003;307:182-9.
Buhr C, Gössl M, Erbel R, Eggebrecht H. Regadenoson in the detection of coronary artery disease. Vasc Health Risk Manag 2008;4:337-40.
Husain Z, Palani G, Cabrera R, Karthikeyan AS, Dhanalakota S, Pathmanathan S, et al. Hemodynamic response, arrhythmic risk, and overall safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic obstructive pulmonary disease and bronchial asthma patients. Int J Cardiovasc Imaging 2012;28:1841-9.
Bouallçgue FB, Nganoa C, Vigne J, Agostini D, Manrique A. Comparative performances of dipyridamole and regadenoson to detect myocardial ischemia using cardiac cadmium-zinc-telluride single-photon emission computerized tomography. J Clin Imaging Sci 2018;8:51.
Assaad M, Berry A, Palanisamy J, Fenner J, Zughaib M. Differential effect of regadenoson versus dipyridamole on heart rate in patients with left bundle branch block: How does it affect the results of pharmacological nuclear stress testing? JRSM Cardiovasc Dis 2019;8:2048004019828257.
Hendel RC, Bateman TM, Cerqueira MD, Iskandrian AE, Leppo JA, Blackburn B, et al. Initial clinical experience with regadenoson, ael selective A2A agonist for pharmacologic stress single-photon emission computed tomography myocardial perfusion imaging. J Am Coll Cardiol 2005;46:2069-75.
Cullom SJ, Case JA, Courter SA, McGhie AI, Bateman TM. Regadenoson pharmacologic rubidium-82 PET: A comparison of quantitative perfusion and function to dipyridamole. J Nucl Cardiol 2013;20:76-83.
Vasu S, Bandettini WP, Hsu L-Y, Kellman P, Leung S, Mancini C, et al. Regadenoson and adenosine are equivalent vasodilators and are superior than dipyridamole: A study of first pass quantitative perfusion cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2013;24:85.
DiBella EVR, Fluckiger JU, Chen L, Kim TH, Pack NA, Matthews B, et al. The effect of obesity on regadenoson-induced myocardial hyperemia: A quantitative magnetic resonance imaging study. Int J Cardiovasc Imaging 2012;28:1435-44.
Stolker JM, Lim MJ, Shavelle DM, Morris DL, Angiolillo DJ, Guzman LA, et al. Pooled comparison of regadenoson versus adenosine for measuring fractional flow reserve and coronary flow in the catheterization laboratory. Cardiovasc Revascularization Med Mol Interv 2015;16:266-71.
Lieu HD, Shryock JC, von Mering GO, Gordi T, Blackburn B, Olmsted AW, et al. Regadenoson, a selective A2A adenosine receptor agonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol 2007;14:514-20.
van Nunen LX, Lenders GD, Schampaert S, van’t Veer M, Wijnbergen I, Brueren GRG, et al. Single bolus intravenous regadenoson injection versus central venous infusion of adenosine for maximum coronary hyperaemia in fractional flow reserve measurement. EuroInterv J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol 2015;11:905-13.
Potier L, Chequer R, Roussel R, Mohammedi K, Sismail S, Hartemann A, et al. Relationship between cardiac microvascular dysfunction measured with 82Rubidium-PET and albuminuria in patients with diabetes mellitus. Cardiovasc Diabetol 2018;17:11.
Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol 2003;41:1387-93.
Fang Y-HD, Liu Y-C, Ho K-C, Kuo F-C, Yang C-F, Yen T-C, et al. Single-scan rest/stress imaging with 99mTc-Sestamibi and cadmium zinc telluride-based SPECT for hyperemic flow quantification: A feasibility study evaluated with cardiac magnetic resonance imaging. PLoS ONE 2017;12:e0183402.
Zavadovsky KV, Mochula AV, Boshchenko AA, Vrublevsky AV, Baev AE, Krylov AL, et al. Absolute myocardial blood flows derived by dynamic CZT scan vs invasive fractional flow reserve: Correlation and accuracy. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01678-z.
Murthy VL, Lee BC, Sitek A, Naya M, Moody J, Polavarapu V, et al. Comparison and prognostic validation of multiple methods of quantification of myocardial blood flow with 82Rb PET. J Nucl Med 2014;55:1952-8.
Bailly M, Thibault F, Courtehoux M, Metrard G, Ribeiro MJ. Impact of attenuation correction for CZT-SPECT measurement of myocardial blood flow. J Nucl Cardiol 2020. https://doi.org/10.1007/s12350-020-02075-7.
Wells RG, Marvin B, Poirier M, Renaud J, deKemp RA, Ruddy TD. Optimization of SPECT measurement of myocardial blood flow with corrections for attenuation, motion, and blood binding compared with PET. J Nucl Med 2017;58:2013-9.
Amer KA, Hurren JR, Edwin SB, Cohen G. Regadenoson versus dipyridamole: A comparison of the frequency of adverse events in patients undergoing myocardial perfusion imaging. Pharmacotherapy 2017;37:657-61.
Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Lancet Respir Med 2015;3:631-9.
Acknowledgments
We express our deepest gratitude to the cardiologists, the technical and radiopharmaceutical staff from CHR of Orleans and CHRU of Tours. This study is part of the French network of University Hospitals HUGO (‘Hôpitaux Universitaires du Grand Ouest’).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Quentin Brana, Frédérique Thibault, Maxime Courtehoux, and Maria Joao Ribeiro have nothing to disclose. Gilles Metrard received honoraria and travel grants from General Electric Healthcare (from previous and other works). Denis Angoulvant received honoraria and travel grants from Astra Zeneca, MSD, Amgen, Servier, Sanofi, Bayer, BMS, Pfizer, Boehringer, artis, ando Nordisk (from previous and other works). Matthieu Bailly received honoraria and travel grants from General Electric Healthcare (from previous and other works).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Rights and permissions
About this article
Cite this article
Brana, Q., Thibault, F., Courtehoux, M. et al. Regadenoson versus dipyridamole: Evaluation of stress myocardial blood flow response on a CZT-SPECT camera. J. Nucl. Cardiol. 29, 113–122 (2022). https://doi.org/10.1007/s12350-020-02271-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02271-5