Abstract
Cardiac scintigraphy has emerged as a key diagnostic test for transthyretin cardiac amyloidosis (ATTR-CA). However, there are potential limitations and pitfalls in the interpretation of cardiac scintigraphy for ATTR-CA that are worth noting. We present here a series of three cases which illustrate some of these important principles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Cardiac amyloidosis (CA) is a form of infiltrative cardiomyopathy associated with significant morbidity and mortality. Once thought to be a rare disease, CA is now known to be relatively common in high risk patient populations, such as older or hospitalized patients with heart failure with preserved ejection fraction or patients who have “low-flow” aortic stenosis.1,2,3,–4 The pathophysiology of CA involves extracellular myocardial deposition of misfolded proteins called amyloid fibrils, resulting in cardiac hypertrophy, restrictive diastolic physiology, and heart rhythm abnormalities. Two types of amyloid fibrils account for the majority of clinical CA—immunoglobulin light chain (AL) and transthyretin (ATTR). Treatment of AL amyloidosis involves antineoplastic therapies targeted against plasma cell proliferation. Treatment of ATTR-CA, in contrast, was previously limited only to supportive care or solid organ transplantation. Due to the absence of therapeutic options, interest in diagnostic modalities for ATTR-CA was lacking. However, the recent development of several targeted therapies aimed at eliminating or stabilizing amyloid fibrils and the publication of a landmark clinical trial showing a reduction in mortality for patients with ATTR-CA treated with an ATTR stabilizer (tafamidis)5 have renewed enthusiasm for the early and accurate diagnosis of ATTR-CA.
Previously, the “gold standard” for diagnosis of ATTR-CA was endomyocardial biopsy, an invasive procedure associated with a risk of life-threatening complications. However, advancements in multimodality imaging for CA have led to the development of diagnostic algorithms which in many cases obviate the need for a biopsy for definitive diagnosis.6,7 Echocardiography, cardiac magnetic resonance imaging, and nuclear imaging all have roles in the diagnosis of CA. Recently, radionuclide imaging has emerged as a key diagnostic test in the evaluation of a patient with suspected ATTR-CA.
Radionuclide imaging (cardiac scintigraphy) for ATTR-CA utilizes calcium avid radiotracers such as 99mTc-labeled pyrophosphate (99mTc-PYP), 3,3-diphosphono-1,2-propanodicarboxylic acid (99mTc-DPD), or hydroxymethylene diphosphonate (99mTc-HMDP), of which only 99mTc-PYP is available in the United States.8 There is preferential uptake of these bone-avid radiotracers in ATTR-CA versus AL-CA and the accuracy of cardiac scintigraphy for the diagnosis of ATTR-CA in published cohorts has been exceptional, with sensitivity and specificity approaching 95% and 99%, respectively.9,10,–11 However, the majority of the published literature comes from amyloid centers of excellence which have significant expertise in the interpretation of cardiac scintigraphy imaging for CA. Furthermore, the patient populations in these studies likely had a high pretest probability for CA which may have biased the results given the large proportion of positive studies. Nevertheless, per contemporary recommendations, a positive result on cardiac scintigraphy with bone-avid radiotracers (without evidence of monoclonal proliferation on laboratory analysis) is diagnostic of ATTR-CA without the need for a biopsy.6,7
Interpretation of Cardiac Scintigraphy Imaging for ATTR-CA
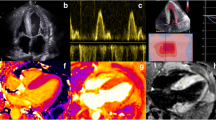
A multi-society consensus guideline for multimodality imaging of CA that includes recommendations for the acquisition and interpretation of cardiac scintigraphy for ATTR-CA was recently released.6,7 Though local protocols vary, planar and SPECT (or SPECT/CT) imaging is typically obtained at 1 hour and sometimes 3 hours after radiotracer injection. Delayed imaging allows for clearance of activity in the blood pool, which can take longer in those patients with renal dysfunction or dilated cardiomyopathy. Interpretation involves a stepwise approach. First, planar and SPECT images are evaluated to identify diffuse myocardial uptake and differentiate myocardial uptake from activity in the blood pool. If myocardial tracer uptake is detected, the interpreting clinician then proceeds to quantify uptake by utilizing the heart-to-contralateral lung ratio (H/CL) and/or by semi-quantitative comparison of the uptake in the myocardium to that of the ribs (Figure 1).
Interpretation of cardiac scintigraphy for ATTR-CA. A Quantitative H/CL analysis of cardiac scintigraphy for ATTR-CA. Similar regions of interest (ROIs) are drawn over the heart and contralateral lung. The ratio of mean counts per pixel of the heart/contralateral lung (H/CL) is calculated—a result of ≥ 1.5 at one hour after radiotracer injection is considered positive for ATTR-CA. B Semi-quantitative visual scoring of cardiac scintigraphy for ATTR-CA. Uptake within the myocardium is compared to that of the ribs via the following grading scale—Grade 0 = No uptake, Grade 1 = Uptake less than that of the ribs, Grade 2 = Uptake equal to that of the ribs, and Grade 3 = Uptake greater than that of the ribs. Grade 2 or 3 uptake is considered “strongly suggestive” of ATTR cardiac amyloidosis, while Grade 0 uptake is considered “not suggestive.” Grade 1 uptake is “equivocal” and could represent early ATTR-CA or AL amyloidosis
The H/CL ratio was previously validated in planar images acquired at one hour after injection and involves drawing a region of interest (ROI) over the myocardium (with care taken not to include the ipsilateral lung or the sternum) and a similar ROI over the contralateral lung (with care to avoid the cardiac silhouette) (Figure 1A).11 The H/CL is then calculated as the ratio of mean counts per pixel over the heart versus the contralateral lung. An H/CL ratio ≥ 1.5 at one hour was both sensitive and specific for the diagnosis of ATTR-CA. Some reports have suggested if this ratio is measured 3 hours post injection, an H/CL ratio of 1.3 is a more appropriate cutoff.9
Semi-quantitative analysis was previously validated at 3 hours and involves visual comparison of uptake within the myocardium to rib uptake and assigning a score from 0 to 3 (Figure 1B).10,12 A semi-quantitative visual score of 2 or 3 is considered “strongly suggestive” of ATTR-CA, while a score of 0 is “not suggestive.” A semi-quantitative score of 1 is an “equivocal” result and may indicate early ATTR-CA or AL amyloidosis.
Case Series
As the incidence of CA has grown with improved recognition and diagnostics, so too has the number of centers implementing cardiac scintigraphy for CA. Given more nuclear labs are incorporating cardiac scintigraphy for ATTR-CA into their workflow, it is prudent to highlight some potential pitfalls in the interpretation of these studies. We present a case series of three patients who underwent 99mTc-PYP imaging at our center for suspected ATTR-CA to illustrate important practical challenges in cardiac scintigraphy interpretation.
Case 1
Case presentation
A 70-year-old woman with a history of paroxysmal atrial fibrillation, hypertension, diabetes, and hyperlipidemia presented to an outside hospital with an acute anterior ST-elevation myocardial infarction (MI). She underwent percutaneous coronary intervention with a drug-eluting stent placed in her mid-left anterior descending (LAD) artery; however, she subsequently developed cardiogenic shock requiring multiple inotropes/vasopressors and intra-aortic balloon pump placement. Due to inability to wean hemodynamic support, she was transferred to our facility for further evaluation and management. Echocardiography revealed reduced left ventricular (LV) systolic function [ejection fraction (EF) 31%] with regional wall motion abnormalities in the LAD territory, normal left ventricular size and wall thickness, restrictive (grade III) diastolic dysfunction, severely elevated left atrial pressures with low mitral annular tissue doppler velocities (average e’ = ~ 5 cm/s), mildly dilated right ventricle with reduced systolic function, and a small pericardial effusion. Given the inability to wean the patient completely from hemodynamic support, as well as very low voltage on ECG, there was concern from the managing team for a possible concomitant infiltrative process. Laboratory analysis for AL amyloidosis was sent and she was referred for 99mTc-PYP imaging to evaluate for ATTR-CA.
The planar images from the patient’s study are shown in Figure 2. The calculated H/CL ratio was 1.6 and the semi-quantitative score was given a grade of 3 (Figure 2). The final interpretation of the study was that it was strongly suggestive of the diagnosis of ATTR-CM. Due to her unusual presentation, the patient subsequently underwent endomyocardial biopsy which was negative for cardiac amyloidosis. Review of SPECT and SPECT/CT sequences showed myocardial uptake was limited to the mid to apical anterior and anteroseptal walls, consistent with the territory involved with recent myocardial infarction (Figure 3).
Discussion
Although regional myocardial uptake on cardiac scintigraphy may be seen in early ATTR-CA, the disease is typically associated with diffuse uptake throughout the myocardium. In this case, SPECT imaging was necessary to localize the myocardial uptake to the LAD territory, as on planar imaging the uptake appeared to be more diffuse. Cardiac scintigraphy imaging with bone-avid radiotracers was originally used to detect areas of acute MI, as myocardial necrosis is associated with significant regional efflux of intracellular Ca2+.13 Cardiac scintigraphy can therefore produce false positive results in the setting of a recent myocardial infarction as demonstrated in this patient’s case. For this reason, many experts suggest waiting at least 4 weeks after acute MI prior to referring for cardiac scintigraphy imaging for ATTR-CA.14 The time from this patient’s MI to her 99mTc-PYP study was approximately 3.5 weeks, and her imaging still revealed intense regional myocardial uptake, suggesting that perhaps the waiting period should be longer.
This case highlights the need to determine appropriateness for cardiac scintigraphy imaging by screening for conditions that may influence the interpretation of the study, such as a recent MI. Other conditions can also produce regional areas of increased counts, including mitral annular calcification and aortic valve calcification. SPECT imaging can be helpful to localize areas of myocardial uptake which may aid in formulating a differential diagnosis.
Case 2
Case presentation
A 57-year-old woman with a history of left-sided breast cancer status post mastectomy, radiation therapy, and chemotherapy with an anthracycline containing regimen presented with 1 year of progressive dyspnea on exertion. Her ECG demonstrated low voltage in the limb leads and Q waves in leads V1-V2 (pseudo-infarct pattern). Her echocardiogram was significant for a LVEF of 71% with moderate concentric LV hypertrophy, grade II diastolic dysfunction with medial and lateral e’ < 5cm/s, biatrial enlargement, and reduced global longitudinal strain with relative sparing of the apex (“cherry on top” pattern). Overall, her presentation was thought to be strongly suggestive of CA and she was referred for serum/urine immunofixation electrophoresis and free light chain assay as well as 99mTc-PYP imaging. Her immunofixation electrophoresis was suspicious for a monoclonal free lambda light chain and her free kappa/lambda ratio was significantly reduced at 0.12, suggestive of lambda light chain AL amyloidosis. 99mTc-PYP imaging revealed intense myocardial uptake at 1 hour with less intense uptake (but still greater than or equal to that of rib uptake) with follow up imaging at 3 hours (Figures 4 and 5). The H/CL ratio was 1.83. The study was read as strongly suggestive of ATTR-CA. Due to these findings suggestive of both AL and ATTR-CA, the patient was referred for endomyocardial biopsy with tissue fiber typing. Biopsy revealed CA with amyloid fibrils of the AL type, confirming a diagnosis of AL amyloidosis.
Discussion
Although cardiac scintigraphy has high sensitivity and specificity for the diagnosis of ATTR-CA, patients with AL-CA often exhibit mild uptake (Grade 1). Moreover, prior reports have revealed that > 20% of individuals with AL-CA can display more intense (Grade 2 or 3) uptake,10 as was observed in this case. Therefore, it is critical that AL amyloidosis is ruled out with laboratory analysis for any patient in whom a diagnosis of ATTR-CA is considered. This point is emphasized in the recent multi-society consensus guidelines on multimodality imaging for CA.6,7 Serum and urine immunofixation electrophoresis and serum free kappa/lambda light chain assay are 99% sensitive for the presence AL amyloidosis and are therefore adequate screening studies to rule out this alternative diagnosis.15 The results of 99mTc-PYP imaging should always be considered in the context of the results of these laboratory studies and further workup should be pursued as indicated.
Case 3
Case presentation
An 89-year-old man with a history of aortic valve disease and coronary artery disease status post remote surgical bioprosthetic aortic valve replacement and two-vessel coronary artery bypass surgery, sick sinus syndrome with permanent implantable dual-chamber pacemaker, paroxysmal atrial fibrillation, and acute on chronic kidney disease presented as a referral from an outside hospital for evaluation by our valve team for progressive shortness of breath and recurrent admissions for heart failure. Electrocardiogram revealed atrial fibrillation with a ventricular paced rhythm. Echocardiography was significant for a mildly dilated LV with mildly reduced systolic function (EF 40%), mild concentric LV hypertrophy, moderate-severe biatrial dilation, and severe pulmonary hypertension (RV systolic pressure 65 mmHg). The aortic valve prosthesis appeared well seated with mild bioprosthetic aortic stenosis and mild-moderate aortic regurgitation; there was otherwise moderate mitral and tricuspid regurgitation. Notably, LV global longitudinal strain was abnormal at − 9.75% with relative sparing of the apex characteristic of CA. The patient was therefore referred for CA workup with AL labs (which were unrevealing) and 99mTc-PYP imaging.
Planar images from the patient’s 99mTc-PYP scan are shown in Figure 6. The H/CL ratio at one hour was 1.9. The study was given a semi-quantitative score of 1 at 3 hours and the overall interpretation was that the study was “equivocal” for the diagnosis of ATTR-CA, which could represent early ATTR-CA or AL amyloidosis. Notably, SPECT/CT imaging showed a large right-sided pleural effusion (Figures 6 and 7). The patient was subsequently referred for endomyocardial biopsy which was negative for CA.
Planar imaging and coronal SPECT/CT imaging at one hour after radiotracer injection for patient in case #3. Note the apparent myocardial uptake on planar imaging which was given a semi-quantitative score of 1. The H/CL ratio was calculated as 1.9 based on the ROIs drawn here. Note the decreased counts in the contralateral lung corresponding to a large pleural effusion on the contralateral side seen on the corresponding coronal SPECT/CT slice
Discussion
This case illustrates several key points. First, it is critical to ensure that ROIs are appropriately drawn and to understand limitations of the quantitative approach when interpreting the H/CL. Focal extracardiac uptake such as from metastatic (“hot”) lesions or focal rib uptake can lead to false positive or false negative results. Moreover, extracardiac sources of decreased counts, such as pleural or pericardial effusions, can also cause misleading results. If possible, the ROIs should be adjusted to avoid these sources of error. In this patient’s case, a very large pleural effusion (seen on SPECT/CT imaging, Figure 7) in the contralateral thorax caused a reduction of counts over the contralateral lung field and, consequently, a falsely elevated H/CL ratio. In this instance, regardless of how the contralateral ROI was adjusted, the H/CL ratio would still be inappropriately high.
Second, though there was apparent uptake in the myocardium on planar images at one hour, delayed imaging and SPECT imaging revealed all of this activity to be in the blood pool with no uptake in the myocardium itself (Figure 7). As discussed previously, in this patient with renal dysfunction, clearance of radiotracer from the blood pool was likely delayed. This highlights the importance of delayed imaging and SPECT sequences for distinguishing blood pool from true myocardial activity.8
Conclusion
Cardiac scintigraphy imaging with bone-avid radiotracers such as 99mTc-PYP has emerged as an essential tool in the diagnostic algorithm for ATTR-CA and will likely continue to see remarkable growth and adoption in the near future. However, there are potential pitfalls in the interpretation of these studies that are worth noting. Through a series of cases, we illustrated the following key principles:
-
(1)
Ensure appropriate patient selection and timing of imaging—Acute MI can cause focal uptake and therefore lead to false positives. Imaging should be delayed until at least 4 weeks (and possibly longer) after an acute MI.
-
(2)
Rule out AL amyloidosis—AL-CA can sometimes cause Grade 2 or 3 uptake on 99mTc-PYP imaging. Therefore, this diagnosis must be excluded with appropriate laboratory screening in every patient with suspected CA.
-
(3)
Understand potential sources of error in the quantitative analysis using H/CL ratio—False positives/negatives can be caused by focal extracardiac uptake (ribs, metastatic lesions), calcific valvular disease, and pleural/pericardial effusions. If possible, ROIs should be adjusted and/or interpreted accordingly.
-
(4)
Distinguish blood pool activity from true myocardial uptake—Renal dysfunction and dilated cardiomyopathy can lead to delayed clearance of activity from the blood pool. Delayed imaging and SPECT sequences can help differentiate blood pool from myocardial activity.
As newer positron emission tomography (PET) radiotracers come through the development pipeline and seek to make non-invasive type-specific molecular amyloid diagnosis a reality,16 some of the issues discussed here may become less relevant. In the interim, nuclear imaging laboratories seeking to implement cardiac scintigraphy imaging for ATTR-CA should be aware of the limitations of the technique and understand how to approach these common challenges.
References
Treibel TA, Fontana M, Gilbertson JA, Castelletti S, White SK, Scully PR, et al. Occult transthyretin cardiac amyloid in severe calcific aortic stenosis: Prevalence and prognosis in patients undergoing surgical aortic valve replacement. Circ Cardiovasc Imaging 2016;9:1-11. https://doi.org/10.1161/CIRCIMAGING.116.005066.
Longhi S, Lorenzini M, Gagliardi C, Milandri A, Marzocchi A, Marrozzini C, et al. Coexistence of degenerative aortic stenosis and wild-type transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging 2016;9:325-7. https://doi.org/10.1016/j.jcmg.2015.04.012.
Bennani Smires Y, Victor G, Ribes D, Berry M, Cognet T, Méjean S, et al. Pilot study for left ventricular imaging phenotype of patients over 65 years old with heart failure and preserved ejection fraction: the high prevalence of amyloid cardiomyopathy. Int J Cardiovasc Imaging 2016;32:1403-13. https://doi.org/10.1007/s10554-016-0915-z.
Koyama J. Prognostic significance of occult transthyretin cardiac amyloidosis in patients with severe aortic stenosis undergoing surgical aortic valve replacement. Circ Cardiovasc Imaging 2016. https://doi.org/10.1161/circimaging.116.005320.
Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med 2018;379:1007-16. https://doi.org/10.1056/NEJMoa1805689.
Dorbala S, Ando Y, Bokhari S, Dispenzieri A, Falk RH, Ferrari VA, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: part 1 of 2—evidence base and standardized methods of imaging. J Nucl Cardiol 2019;26:2065-123.
Dorbala S, Ando Y, Bokhari S, Dispenzieri A, Falk RH, Ferrari VA, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: part 2 of 2—diagnostic criteria and appropriate utilization. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01760-6.
Dorbala S, Bokhari S, Miller EJ, Bullock-Palmer R, Soman P, Thompson R. 99mTechnetium-pyrophosphate imaging for transthyretin cardiac amyloidosis ASNC cardiac amyloidosis practice points; 2019.
Castano A, Haq M, Narotsky DL, Goldsmith J, Weinberg RL, Morgenstern R, et al. Multicenter study of planar technetium 99m pyrophosphate cardiac imaging: Predicting survival for patients with ATTR cardiac amyloidosis. JAMA Cardiol 2016;1:880-9. https://doi.org/10.1001/jamacardio.2016.2839.
Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016;133:2404-12. https://doi.org/10.1161/CIRCULATIONAHA.116.021612.
Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99mTc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging 2013;6:195-201. https://doi.org/10.1161/CIRCIMAGING.112.000132.
Perugini E, Guidalotti PL, Salvi F, Cooke RMT, Pettinato C, Riva L, et al. Noninvasive etiologic diagnosis of cardiac amyloidosis using 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid scintigraphy. J Am Coll Cardiol 2005;46:1076-84. https://doi.org/10.1016/j.jacc.2005.05.073.
Billerica N. Acute myocardial infarct imaging with Tc-99m pyrophosphate. J Nucl Med Technol 1984;12:74-6.
Abou Ezzeddine O, Acharya G, Grogan M. TTR vs AL cardiac amyloidosis: don’t rely on imaging alone. Medscape. https://www.medscape.com/viewarticle/913672. Accessed 10 Feb 2020.
Witteles RM, Bokhari S, Damy T, Elliott PM, Falk RH, Fine NM, et al. Screening for transthyretin amyloid cardiomyopathy in everyday practice. JACC Heart Fail 2019;7:709-16. https://doi.org/10.1016/j.jchf.2019.04.010.
Kim YJ, Ha S, Kim Y. Cardiac amyloidosis imaging with amyloid positron emission tomography: A systematic review and meta-analysis. J Nucl Cardiol 2020;27:123-32. https://doi.org/10.1007/s12350-018-1365-x.
Disclosures
Ramsey M. Wehbe—No relevant conflicts of interest to disclose. Preeti Kansal—No relevant conflicts of interest to disclose. Thomas A. Holly—No relevant conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Funding This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Rights and permissions
About this article
Cite this article
Wehbe, R.M., Kansal, P. & Holly, T.A. Cases from a busy nuclear cardiology laboratory: Potential pitfalls in the interpretation of cardiac scintigraphy for ATTR cardiac amyloidosis. J. Nucl. Cardiol. 28, 653–660 (2021). https://doi.org/10.1007/s12350-020-02094-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02094-4