Abstract
Background
The sympathetic nervous system provides an important trigger for major arrhythmic events through regional heterogeneity of sympathetic activity, which could be evaluated by SPECT imaging as the regional MIBG washout rate (WR). There is little information available on the prognostic value of regional WR in SPECT imaging for the prediction of sudden cardiac death (SCD) in patients with chronic heart failure (CHF).
Methods
We studied 73 CHF outpatients with LVEF < 40%. At study entry, the regional WR was measured in 17 segments on the polar map. We defined abnormal regional WR as both the regional WR range (maximum − minimum regional WR) and maximum regional WR > mean value + 2SD obtained in 15 normal controls.
Results
During a mean follow-up of 7.5 ± 4.1 years, 15 of 73 patients had SCD. The abnormal regional WR and abnormal global WR on planar images were significantly and independently associated with SCD. Patients with both the abnormal regional WR and global WR had a significantly higher risk of SCD than those with none of these criteria.
Conclusions
The analysis of regional MIBG WR on SPECT imaging provides additional prognostic value to global WR on planar images for SCD prediction in CHF patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The identification of patients with chronic heart failure (CHF) who are at risk for sudden cardiac death (SCD) remains an important goal.1 As CHF largely involves disruption of the neurohumoral state, neural innervation plays a key role in the pathophysiology of this condition.2 In patients with CHF, sympathetic overactivity produces deleterious neurohumoral and myocardial structural changes that worsen the patient’s condition and that increase the likelihood of arrhythmic SCD.3
Cardiac iodine-123 (I-123) meta-iodobenzylguanidine (MIBG) imaging is useful for the estimation of cardiac sympathetic nerve activity and can predict poor clinical outcomes, including life-threatening arrhythmia and sudden cardiac death, in patients with CHF.4,5,6,7,8,9,10,11,12,–13 Most cardiac MIBG studies are based on the measurements from anterior planar images of the chest, with cardiac uptake quantified in terms of the heart-to-mediastinum ratio (HMR) and washout rate (WR) between early and delayed images. Recently, it has become more common for MIBG single-photon emission computed tomography (SPECT) imaging to be used for clinical evaluation of patients.14,15,–16 The sympathetic nervous system provides an important trigger for major arrhythmic events through regional heterogeneity of sympathetic activity,17 which might be evaluated by SPECT imaging as the regional MIBG washout rate (WR).18,19,–20 However, no data on the prognostic significance of the regional WR in CHF patients are currently available. Therefore, the present study investigated whether the regional WR in SPECT imaging provides additional prognostic value to global WR on planar images for the prediction of SCD in CHF patients.
Methods
Study patients
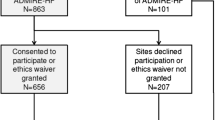
We studied 80 outpatients with stable CHF who had been diagnosed based on clinical signs and symptoms according to the Framingham criteria.21 The study patients were the participants of our prospective cohort study (unpublished) from 1995 October to 1999 October, where the efficacy of carvedilol or amlodipine was investigated. To be included in this study, all patients who had experienced at least one episode of decompensated heart failure were required to be stable for at least 3 months on conventional therapy with angiotensin-converting enzyme inhibitors, diuretics and digoxin, and left ventricular ejection fraction determined by radionuclide angiography remained <40% after the medical treatment. The exclusion criteria were sustained ventricular tachycardia, significant renal dysfunction, insulin-dependent diabetes mellitus, and autonomic neuropathy. None of the patients were receiving beta-blockers or had an implantable cardioverter defibrillator (ICD), biventricular pacemaker, or biventricular defibrillator at enrollment. At the time of entry into the study, all patients had been assessed by cardiac MIBG imaging, echocardiography, and Holter electrocardiography, and a venous blood sample was obtained from each patient. Osaka General Medical Center’s Review Committee approved the protocol of this study, and all patients provided written informed consent to participate.
Cardiac MIBG imaging
All patients were assessed while resting in the supine position by myocardial imaging with I-123 MIBG (FUJIFILM RI Pharma Co., Ltd, Tokyo, Japan) using a dual-head gamma camera (Prism 2000, Picker, Bedford, Ohio) equipped with a low-energy, high-resolution, parallel-hole collimator. The patients were injected intravenously with a 111-MBq dose of I-123 MIBG after an overnight fast and underwent anterior planar and SPECT imaging of the thorax beginning at 20 min (early) and 3 h 20 min (delayed) post injection. A 128 × 128 matrix was used for SPECT studies, and 20% energy peak was centered around the 159-keV energy peak of I-123 MIBG. All planar and SPECT images were reviewed by two independent observers who were blinded to clinical data.
As previously reported,22 HMRs on early and delayed images were determined from the counts/pixel in a visually drawn region of interest over the whole left ventricular myocardium divided by the counts/pixel in a 7 × 7 pixel region of interest placed in the upper mediastinum. The cardiac global WR of MIBG was calculated from the initial and delayed images with the correction for radioactive decay of I-123 and background subtraction. Based on findings from our previous study,22 an abnormal global WR was defined as >27%.
I-123 MIBG SPECT studies were processed with filtered back-projection and reconstructed into the standard long and short axis, and perpendicular to the heart axis 7 patients were excluded from this analysis because MIBG SPECT reconstruction was difficult because of too low MIBG uptake in 2 patients and overlying extracardiac (lung and liver) accumulation interfered the cardiac visibility in 5 patients. In the remaining 73 patients, we analyzed the SPECT images with cardioBull,23 fully automated software for the quantification of I-123 MIBG SPECT (FUJIFILM RI Pharma). We constructed a polar map of MIBG uptake, which was divided into 17 segments, and the regional MIBG washout rate in each segment was calculated by (regional counts in early image − regional counts in delayed image) × 100/(regional counts in early image) with correction for radioactive decay without background subtraction. The regional WR range was calculated by subtracting the minimum regional WR from the maximum regional WR among 17 segments. We defined the abnormal regional WR as both the regional WR range and maximum regional WR > mean value + 2SD obtained in 15 subjects (chest pain syndrome in 12 subjects, mild hypertension in 2 subjects, and suspected vasospastic angina in 1 subject) with normal cardiac function documented by echocardiography, 27.2% and 31.1%, respectively. Furthermore, the extent and severity maps were also generated automatically based on a control database acquired from the 15 control subjects. We obtained summed extent score (SES) as the sum total of the % area where I-123 MIBG uptake was less than mean-2SD of normal controls. SES could range from 0 to 1700 (17 × 100). A scoring algorithm for the evaluation of low uptake employs a 5-point scoring system as 0-4 for normal, mildly abnormal, moderately abnormal, severe abnormal, and perfusion defect, respectively. The summed severity (SSS) scores were obtained by summing the score for all segments. SSS could range from 0 to 68 (17 × 4). We compared SES and SSS to abnormal regional WR with regard to prediction of SCD.
Echocardiography and 24-hour Holter monitoring
The patients were assessed by two-dimensional echocardiography using an SSH-380A recorder equipped with a 2.5- or 3.75-MHz transducer (Toshiba, Tokyo, Japan). Left ventricular end-diastolic dimension and left atrial dimension were measured using standard techniques. The patients were also assessed by 24-hour electrocardiogram monitoring using an 8000 Holter system (Marquette Electronics, Milwaukee, WI, USA). Ventricular arrhythmias were classified according to Lown’s grade, and nonsustained ventricular tachycardia was defined as 5 or more consecutive premature ventricular beats lasting <30 s. We also performed serial Holter monitoring at 2, 6, 12, 18, 24, 30, and 36 months after the enrollment, and every one year thereafter.
Measurements of plasma noradrenaline concentration and other parameters
To assess the plasma noradrenaline concentration, serum sodium, and creatinine levels, blood sampling was performed from an intravenous cannula after resting for at least 30 min in the supine position. The estimated glomerular filtration rate was calculated by the Modification of Diet in Renal Disease formula. Plasma noradrenaline concentration was determined in ethylenediaminetetraacetic acid plasma by high-performance liquid chromatography at Shionogi Biomedical Laboratory (Osaka, Japan).
Follow-up
All study patients were then followed in our hospital by clinicians who were not aware of the results of cardiac MIBG imaging. The primary endpoint of this study was SCD, defined as witnessed cardiac arrest or death within 1 h after the onset of acute symptoms or unexpected or unwitnessed death in a patient known to have been well within the previous 24 h. The secondary endpoint was the development of sustained ventricular tachycardia lasting ≥30 s.
Statistical analysis
Data are shown as the mean value ± SD. Differences among continuous and discrete variables were compared using Student’s t test and Fisher’s exact test in patients with and without cardiac events, respectively. Cardiac event-free rates were calculated using the Kaplan-Meier method, and differences between each group were detected using the log-rank test. The Cox proportional hazards regression model was used to determine the significance of variables predictive of outcomes by univariate analysis (P < 0.05) as independent predictors of cardiac events on multivariate analysis. All data were statistically analyzed using StatView version 5 (SAS Institute, Cary, North Carolina). P values < 0.05 were considered to indicate statistical significance.
Results
Patient characteristics
The mean age of the patients was 64 ± 12 years. There were 54 men and 19 women. CHF was due to ischemic heart disease in 37 patients and due to idiopathic dilated cardiomyopathy in 36 patients. Mean New York Heart Association (NYHA) functional class was 2.1 ± 0.6, with 10% of patients in class I, 67% in class II, and 22% in class III. Mean LVEF was 29 ± 7%.
Comparison of baseline characteristics between patients with and without SCD
During a mean follow-up of 7.5 ± 4.1 years, 15 patients had SCD. The baseline characteristics of patients with and without SCD are listed in Table 1. There were no differences in age, gender, the proportion of patients with ischemic heart disease, NYHA functional class, heart rate, blood pressure, drug use, left ventricular end-diastolic dimension, left atrial dimension, serum sodium and creatinine levels, estimated glomerular filtration rate, or plasma concentration of noradrenaline. Patients with SCD had a significantly greater Lown’s grade.
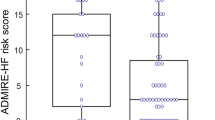
The results of cardiac MIBG planar and SPECT imaging are shown in Table 2. In the planar image analysis, patients with SCD had a significantly smaller HMR on the delayed images and greater global WR than those without SCD. Representative SPECT images in patients with and without SCD are shown in Figures 1 and 2, respectively. In SPECT image analysis, abnormal regional WR was more frequently observed in patients with SCD than in those without SCD, while patients with SCD had non-significantly greater SSS on the delayed image.
Prognostic analysis
Univariate and multivariate analyses for the identification of CHF patients at risk for SCD are shown in Table 3. Multivariate analysis revealed that both abnormal global WR and abnormal regional WR were significantly and independently associated with SCD, although HMR or SSS on the delayed image showed the significant association at univariate analysis.
SCD-free rate curves, according to abnormal global WR and abnormal regional WR, are shown in Figure 3. Patients with both abnormal global WR and abnormal regional WR had a significantly higher rate of SCD than those with either abnormal global WR or abnormal regional WR or than patients with none of these criteria (P < 0.0001, 45% vs. 15% vs. 9%, respectively). The hazard ratio for SCD prediction in the patients with both abnormal global WR and abnormal regional WR was about sixfold higher than that of patients with either abnormal global WR or abnormal regional WR. Furthermore, it was threefold higher than that of patients with abnormal global WR only.
As for the development of sustained ventricular tachycardia, patients with both abnormal global WR and abnormal regional WR had a significantly higher rate of the arrhythmic event than those with either abnormal global WR or abnormal regional WR or than patients with none of these criteria (P = 0.0001, 16% vs. 10% vs. 0%, respectively).
Discussion
The major findings of this study were that the abnormal regional WR in SPECT imaging was significantly associated with SCD, independently of global WR in the planar imaging, and that the combination of abnormal global WR and abnormal regional WR could improve the prediction of SCD in CHF patients. These data suggest that the analysis of regional WR on SPECT imaging provides additional prognostic value to global WR for the prediction of SCD in CHF patients, which suggests that imaging assessment of regional inhomogeneity of adrenergic innervations also holds promise to identify patients with CHF who are at risk for SCD.
Factors that increase the electrical heterogeneity in the ventricles may be important in promoting the development of ventricular arrhythmias. Theoretically, a ventricle that is totally homogenous electrically would not be arrhythmogenic. One such factor responsible for electrical heterogeneity is sympathetic heterogeneity. Sympathetically denervated areas of myocardium exhibit abnormal ventricular refractoriness such as greater shortening of the effective refractory period with norepinephrine infusion compared to normally innervated regions, predisposing to re-entrant arrhythmia.17 These findings suggest the present result that abnormal regional WR, which would reflect the regional heterogeneity of sympathetic activity, provides additional value to global WR for the prediction of SCD in CHF patients.
Impaired regional myocardial sympathetic heterogeneity can be imaged with SPECT with MIBG.24 Previous studies with regard to regional MIBG WR have evaluated the severity of dilated cardiomyopathy,18 the effectiveness of beta-blocker therapy in patients with dilated cardiomyopathy,19 and the relationship between cardiac sympathetic nerve function and myocardial necrosis in patients with CHF due to ischemic heart disease.20 However, there is no information available on the prognostic significance of regional WR in CHF patients. In the present study, abnormal regional WR in SPECT imaging was significantly associated with SCD. This finding is supported by previous basic and clinical studies that have documented an important role for sympathetic activation in the development of lethal ventricular tachyarrhythmias and that have shown that inhomogeneity in myocardial innervations might create a myocardial substrate that is particularly vulnerable to arrhythmic death.25
Most investigators performing MIBG SPECT studies had shown that arrhythmic event risk increases with the size of denervated area. Patients with inducible ventricular tachycardia during electrophysiology testing had a greater total MIBG SPECT defect score than those who did not have inducible ventricular tachycardia.26 In prospective studies in CHF patients with ICDs, MIBG SPECT defect size was a significant and independent predictor of ventricular arrhythmia requiring ICD therapy.27,28 In the present study, although the summed severity score on the delayed SPECT image was significantly associated with SCD within univariate analysis, multivariate analysis showed that the MIBG defect size had no independent association with SCD. The difference in results between this study and previous studies might be partially due to the definition of the study endpoint (SCD vs. appropriate ICD shock therapy). The occurrence of ICD shock in CHF patients does not necessarily mean that they would have expected SCD if not for the device, although this is the currently accepted hypothesis.
Based on several large prospective randomized trials, ICD implantation as primary prevention is a Class IA indication for CHF patients with NYHA II-III CHF and LVEF ≤ 35%.29 Nevertheless, most patients who receive an ICD based on these criteria do not use their device, and it is widely acknowledged that LVEF is an imperfect predictor of arrhythmic death. The patients included in his study were treated during the last century, and we realized the advantage for this study of being able to follow patients who did not have an ICD as it was before these guidelines were established. In the present study, the hazard ratio for SCD prediction in patients with both abnormal global WR and abnormal regional WR was about threefold higher than that in patients with abnormal global WR alone. These results suggest that the combination of global WR and regional WR could identify a subset of patients who are at higher risk of SCD and who could benefit from ICD implantation.
There are several limitations to the present study. For example, the small sample size, the empirically chosen study population, and the empirically chosen follow-up time represent the major limitations. The prognostic value was evaluated in a too small sample size. So the prognostic value should be verified in another study with a larger sample size. Second, no study patients were treated according to current standards of care (e.g., beta-blockers or ICD) at study entry, because most study patients were participants of our prospective cohort study that were treated during the last century. The medications used during follow-up may also have affected the MIBG uptake and clinical outcomes. Beta-blocker was administered in 35 of 73 study patients just after enrollment. In patients with such beta-blocker, abnormal regional WR was significantly associated with SCD (P = 0.01). Third, we excluded patients with global MIBG defects, as this made SPECT reconstruction difficult, and we excluded patients with poor tomographic images (secondary to accumulation of tracer within the liver and lung accumulation that interferes with cardiac visibility). Forth, the subtracting minimal regional WR from maximal WR, the WR range, might not reflect the regional WR dispersion. However, in the present study, the abnormal regional WR was defined not only as the WR range > median value but also maximum regional WR > median value. The standard deviation of regional WR was significantly greater in patients with than those without increased abnormal regional WR (10.0 ± 2.4 vs. 6.9 ± 3.0%, P < 0.0001). From this finding, the definition of abnormal regional WR in this study would reflect the regional WR dispersion. Furthermore, a technique known as modified fractal analysis may be better to assess the regional WR dispersion.30 Further study will be needed to investigate the clinical significance of fractal analysis in MIBG SPECT image. Lastly, because we only studied stable outpatients, patients with NYHA functional class IV disease were not included. Therefore, our results should not be generalized to inpatients with severe CHF.
New knowledge gained
The abnormal regional MIBG WR in SPECT imaging provides additional prognostic value to global WR for the prediction of SCD in CHF patients.
Abbreviations
- SPECT:
-
Single-photon emission computed tomography
- MIBG:
-
Meta-iodobenzylguanidine
- WR:
-
Washout rate
- SCD:
-
Sudden cardiac death
- CHF:
-
Chronic heart failure
- LVEF:
-
Left ventricular ejection fraction
- ICD:
-
Implantable cardioverter defibrillator
- HMR:
-
Heart-to-mediastinum ratio
- SES:
-
Summed extent score
- SSS:
-
Summed severity score
References
Wellens HJJ, Shwartz PJ, Lindemans FW, Buxton AE, Goldberger JJ, Hohnloser SH, et al. Risk stratification for sudden cardiac death: Current status and challenges for the future. Eur Heart J. 2014;35:1642–51.
Cohn JN, Levine BT, Olivari MT, Garberg V, Lura D, Francis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic heart failure. N Engl J Med. 1984;311:819–23.
Floras JS. Clinical aspects of sympathetic activation and parasympathetic withdrawal in heart failure. J Am Coll Cardiol. 1993;22:72A–84A.
Merlet P, Valette H, Dubois-Randé JL, Moyse D, Duboc D, Dove P, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med. 1992;33:471–7.
Yamada T, Shimonagata T, Fukunami M, Kumagai K, Ogita H, Hirata A, et al. Comparison of the prognostic value of cardiac iodine-123 metaiodobenzylguanidine imaging and heart rate variability in patients with chronic heart failure: A prospective study. J Am Coll Cardiol. 2003;41:231–8.
Kioka H, Yamada T, Mine T, Morita T, Tsukamoto Y, Tamaki S, et al. Prediction of sudden death in patients with mild-to-moderate chronic heart failure by using cardiac iodine-123 metaiodobenzylguanidine imaging. Heart. 2007;93:1213–8.
Tamaki S, Yamada T, Okumura Y, Motita T, Sanada S, Tsukamoto Y, et al. Cardiac iodine-123 metaiodobenzylguanidine imaging predicts sudden cardiac death independently of left ventricular ejection fraction in patients with chronic heart failure and left ventricular systolic dysfunction. J Am Coll Cardiol. 2009;53:426–35.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial 123I-mIBG imaging and cardiac events in heart failure: Results of the prospective ADMIRE-HF study. J Am Coll Cardiol. 2010;55:2212–21.
Kuramoto Y, Yamada T, Tamaki S, Okuyama Y, Morita T, Furukawa Y, et al. Usefulness of cardiac iodine-123 meta-iodobenzylguanidine imaging to improve prognostic power of Seattle heart failure model in patients with chronic heart failure. Am J Cardiol. 2011;107:1185–90.
Nakata T, Nakajima K, Yamashina S, Yamada T, Momose M, Kasama S, et al. A pooled analysis of multicenter cohort studies of 123I-mIBG imaging of sympathetic innervation for assessment of long-term prognosis in heart failure. JACC Cardiovasc Imaging. 2013;6:772–84.
Al Badarin FJ, Wimmer AP, Kennedy KF, Jacobson AF, Bateman TM. The utility of ADMIRE-HF risk score in predicting serious arrhythmic events in heart failure patients: Incremental prognostic benefit of cardiac 123I-mIBG scintigraphy. J Nucl Cardiol. 2014;21:756–62.
Kawai T, Yamada T, Tamaki S, Morita T, Furukawa Y, Iwasaki Y, et al. Usefulness of cardiac meta-iodobenzylguanidine imaging to identify patients with chronic heart failure and left ventricular ejection fraction < 35% at low risk of sudden cardiac death. Am J Cardiol. 2015;115:1549–54.
Hakui H, Yamada T, Tamaki S, Morita T, Furukawa Y, Iwasaki Y, et al. Usefulness of cardiac metaiodobenzylguanidine imaging to improve prognostic power of the model for end-stage liver disease scoring system in patients with mild-to-moderate chronic heart failure. Am J Cardiol. 2016;117:1947–52.
Chen J, Folks RD, Verdes L, Manatunga DN, Jacobson AF, Garcia EV. Quantitative I-123 mIBG SPECT in differentiating abnormal and normal mIBG myocardial uptake. J Nucl Cardiol. 2012;19:92–9.
Dimitriu-Leen AC, Sholte AJHA, Jacobson AF. 123I-MIBG SPECT for evaluation of patients with heart failure. J Nucl Med. 2015;56:25S–30S.
Clements IP, Garcia EV, Chen J, Folks RD, Butler J, Jacobson AF. Quantitative iodine-123-metaiodobenzylguanidine (MIBG) SPECT imaging in heart failure with left ventricular systolic dysfunction: Development and validation of automated procedures in conjunction with technetium-99 m tetrofosmin myocardial perfusion SPECT. J Nucl Cardiol. 2016;23:425–35.
Stanton MS, Zipes DP. Modulation of drug effects by regional sympathetic denervation and supersensitivity. Circulation. 1991;84:1709–14.
Yamazaki J, Muto H, Ishiguro S, Okamoto K, Hosoi H, Nakano H, et al. Quantitative scintigraphic analysis of 123I-MIBG by polar map in patients with dilated cardiomyopathy. Nucl Med Com. 1997;18:219–29.
Fukuoka S, Hayashida K, Hirose Y, Shimotsu Y, Ishida Y, Kakuchi H, et al. Use of 123I-MIBG myocardial imaging to predict the effectiveness of beta-blocker therapy in patients with dilated cardiomyopathy. Eur J Nucl Med. 1997;24:523–9.
Marini C, Giorgetti A, Gimelli A, Kusch A, Sereni N, Abbate AL, et al. Extension of myocardial necrosis differently affects MIBG retention in heart failure caused by ischemic heart disease or by dilated cardiomyopathy. Eur J Nucl Med Mol Imaging. 2005;32:682–8.
McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: The Framingham study. N Engl J Med. 1971;285:1441–6.
Ogita H, Shimonagata T, Fukunami M, Kumagai K, Yamada T, Asano Y, et al. Prognostic significance of cardiac I-123 metaiodobenzylguanidine imaging for mortality and morbidity in patients with chronic heart failure: A prospective study. Heart. 2001;86:656–60.
Okuda K, Nakajima K, Hosoya T, Ishikawa T, Matsuo S, Kawano M, et al. Quantification of myocardial perfusion SPECT using freeware package (cardioBull). Ann Nucl Med. 2011;25:571–9.
Witcher T, Hindricks G, Lerch H, Bartenstein P, Borgreffe M, Shober O, et al. Regional myocardial sympathetic denervation in arrhythmogenic right ventricular cardiomyopathy. An analysis using 123I-MIBG scintigraphy. Circualtion. 1994;89:667–83.
Tomaselli GF, Zipes DP. What causes sudden death in heart failure? Circ Res. 2004;95:754–63.
Bax JJ, Kraft O, Buxton AE, Fjeld JG, Parízek P, Agostini D, et al. 123I-mIBG scintigraphy to predict inducibility of ventricular arrhythmias on cardiac electrophysiology testing: A prospective multicenter pilot study. Circ Cardiovasc Imaging. 2008;1:131–40.
Boogers MJ, Borleffs CJ, Henneman MM, van Bommel RJ, van Ramshorst J, Boersma E, et al. Cardiac sympathetic denervation assessed with 123-iodine metaiodobenzylguanidine imaging predicts ventricular arrhythmias in implantable cardioverter-defibrillator patients. J Am Coll Cardiol. 2010;55:2769–77.
Marshall A, Cheetham A, George RS, Mason M, Kelion AD. Cardiac iodine-123 metaiodobenzylguanidine imaging predicts ventricular arrhythmia in heart failure patients receiving an implantable cardioverter-defibrillator for primary prevention. Heart. 2012;9:1359–65.
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–847.
Pretorius H, Menke D, Richards N, Budke B. Modified fractal analysis of brain PET and SPECT defines three distinct cognitive groups in medical office patients: Near normal, mild cognitive impairment and early dementia. J Nucl Med. 2014;55:1851.
Disclosure
No financial or other relationships that could lead to a conflict of interest are associated with this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Daniel Berman, MD.
Rights and permissions
About this article
Cite this article
Yamamoto, H., Yamada, T., Tamaki, S. et al. Prediction of sudden cardiac death in patients with chronic heart failure by regional washout rate in cardiac MIBG SPECT imaging. J. Nucl. Cardiol. 26, 109–117 (2019). https://doi.org/10.1007/s12350-017-0913-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-017-0913-0