Abstract
The burden of cardiovascular diseases (CVDs) in the world is ever growing. They represent the first cause of death worldwide and in Latin America. Nuclear cardiology has a well-established role in the management of patient with CVDs and is being increasingly integrated into the healthcare systems in the region. However, there remains variability as to the infrastructure available across the countries, in terms of existing technology, radiopharmaceuticals, and human resources. The approximate number of gamma (γ) cameras in the region is 1348, with an average of 2.25 per million population; Argentina and Brazil having the largest number. Nearly 80% of the existing cameras are single-photon emission tomography (SPECT), of which 8% are hybrid SPECT-CT systems. Positron emission tomography technology is steadily increasing, and currently, there is an average of 0.25 scanners per million inhabitants, indicating that there is a potential to expand the capacities in order to cover the needs. Four countries have nuclear reactors for research purposes, which allow the production of technetium-99 m (Argentina, Chile, Mexico and Peru), while four (Argentina, Brazil, Cuba, and Mexico) assemble 99Mo-99mTc generators. As for the nuclear cardiology studies, about 80% of studies performed are gated SPECT myocardial perfusion imaging; less than 10% are multi-gated acquisition (mainly for evaluation of cardiac toxicity in cancer patients), and the other 10% correspond to other types of studies, such as viability detection, and adrenergic innervation studies with 123I-MIBG. Physical stress is preferred, when possible, based on the clinical condition of the patient. Regarding human resources, there is an average of 1.1 physicians and 1.3 technologists per γ camera, with 0.1 medical physicists and 0.1 radiopharmacists per center in the region. The future of nuclear cardiology in Latin America and the Caribbean is encouraging, with great potential and possibilities for growth. National, regional, and international cooperation including support from scientific societies and organizations such as International Atomic Energy Agency, American Society of Nuclear Cardiology, and Latin American Association of Biology and Nuclear Medicine Societies, as well as governmental commitment are key factors for the development of the specialty. A multimodality approach in cardiac imaging will contribute to a better management of patients with CVDs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Latin America and the Caribbean (LAC) has a total population of over 600 million inhabitants, with roughly 80% concentrated in urban areas. Life expectancy reaches a mean of 76.9 years (74.1 and 79.7 years for men and women, respectively), and the population is growing at an average of 1.0% annually.1 The region is heterogeneous in terms of mortality due to different prevalence of chronic diseases and investment in health care. Public expense in health care as a percentage of the gross national product varies between 4.4 and 10.9.2
Cardiovascular diseases (CVDs) are the main cause of death in Latin America.3 Data from the World Health Organization (WHO) indicate that the region is currently experiencing a large-scale epidemic of CVDs, which is in part due to increased life expectancy and changes in the epidemiological transition from communicable to noncommunicable diseases. The enormous burden of CVDs in the region coincides with a high prevalence of cardiovascular risk factors such as diabetes mellitus, high blood pressure, obesity, smoking, and dyslipidemia, which results in a higher incidence of coronary events and heart failure with increasing age.3-5 However, it is important to note that in some countries, like Bolivia for example, the most common CVD is Chagas’ cardiomyopathy (70% of cardiac diseases).
Among the possible factors that could explain the high mortality due to CVDs in the LAC region are the heterogeneous investment in prevention, technology, and therapy, including the underuse of therapies that have been shown to be effective, as well as a more conservative approach with later use of surgical and percutaneous coronary interventions (PCI). In Latin America, heart failure tends to occur in younger subjects than in the rest of the world and is most frequently related to ischemic heart disease (IHD).3,5
It is important to point out that an effective way to reduce cardiovascular mortality is to promote primary prevention by identifying and controlling modifiable risk factors and by initiating secondary prevention measures in individuals with established CVD, in which cardiovascular imaging plays a significant role.6
In order to improve the outcomes and optimize the utilization of available resources, it is of pivotal importance to select appropriate treatment options for patients with IHD, including PCI and coronary artery bypass grafting (CABG).
More than 10 years ago, trials such as the Economics of myocardial perfusion imaging (MPI) in Europe: the EMPIRE study7 and the Economics of noninvasive diagnosis: the END study8 demonstrated that MPI can be used as a gatekeeper to prevent patients from undergoing unnecessary invasive procedures and revascularization, leading to cost reduction, which is of particular importance in low- and middle-income countries (LMICs) where resources are scarce. In addition, it has been already shown that an abnormal MPI has the potential to detect patients with increased mortality risk, which increases with the severity and extension of perfusion defects. Identifying a patient with IHD by MPI could allow the initiation of an aggressive secondary prevention strategy using guideline-directed optimal medical treatment as a way to reduce mortality, as well as an adequate invasive treatment selection guided by the amount of ischemia in those patients with severe defects.
Gated SPECT MPI is a valuable technique that offers, in a reproducible and quantitative manner, information about global and regional ventricular function, assessment of intraventricular synchronism and myocardial perfusion. Due to the burden of CVDs in Latin America and in order to support its Member States to tackle this health problem, the International Atomic Energy Agency (IAEA) is currently implementing a regional technical cooperation project entitled “Facing the high incidence of cardiovascular diseases in Latin America and the Caribbean through nuclear cardiology”, with the aim of strengthening capacities for early diagnosis and risk stratification, as well as providing guidance for interventional procedures.
During the first coordination meeting of this regional project held in April 2016, the 16 participating countries (Argentina, Bolivia, Brazil, Chile, Colombia, Costa Rica, Cuba, Dominican Republic, Ecuador, Mexico, Nicaragua, Panama, Paraguay, Peru, Uruguay, and Venezuela) provided information regarding the epidemiological situation and nuclear cardiology practice during 2015 that has been included in the present manuscript. When referring to the nuclear cardiology, this manuscript covers the 16 countries mentioned above, while the information on the general status of nuclear medicine practice also includes data pertaining to El Salvador, Guatemala, Haiti, Honduras, and Jamaica for a total of 21 countries which were included in the recent IAEA publication on the current status of nuclear medicine practice in Latin America and the Caribbean.9 The opinions of various nuclear medicine experts and consultants in the region were also considered.
Trends and Projections of Resources
According to data from the IAEA Nuclear Medicine Database (NUMDAB), the average equipment installation time is beyond 6 years for all types of cameras in low- and middle-income countries. Africa and the Middle East have on average the oldest SPECT cameras, whereas prolonged use of planar cameras, including dedicated small field of view cameras, is observed in Latin America and the Caribbean region, Eastern Europe, and Northern Asia, where some systems have been in operation for more than 30 years.10
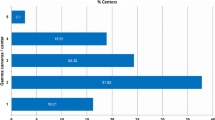
The approximate number of γ cameras in the Latin American and the Caribbean region is 1, 348 with an average of 2.25 per million inhabitants (Figure 1), Argentina and Brazil having the largest number (389 and 360, respectively). Haiti has no nuclear medicine services established.
Figure 2 shows the number of operating γ cameras per million inhabitants in the 16 Latin American countries included in the present analysis, which ranges from 0.3 to 9.6. Argentina, Uruguay, and Chile have the highest ratio, followed by Mexico and Costa Rica.
In countries such as Brazil, Chile, Colombia, Mexico and Uruguay, SPECT technology is dominant. In the whole region, nearly 80% of the existing cameras are SPECT, of which 8% are hybrid (SPECT-CT). Currently, the region has a high replacement rate of existing outdated planar technology, with increasing numbers of SPECT and SPECT-CT instruments.9,11 PET technology is steadily increasing, with a mean of 0.25 per million inhabitants, and a range of 0-0.61 PET cameras per million inhabitants (Figure 3).
As a comparison in the Middle East for instance, the total number of γ cameras is 910 with an average of 2.3 per million inhabitants, which is very similar to the availability of cameras in LAC. Out of the 910 cameras, 107 (12%) are SPECT-CT, while in LAC is 8%. When comparing the PET-CT availability the Middle East has a higher ratio of scanners per population with an average of one PET-CT scanner for 2.04 million vs. one scanner for every 4 million people in LAC.12
In the LAC region, approximately 70% of all nuclear medicine centers are in the private sector and concentrated in capital cities and other large metropolitan areas.
With respect to the production of radioisotopes and radiopharmaceuticals, four countries (Argentina, Chile, Mexico, and Peru) have nuclear reactors for research purposes, which allow some production of technetium-99 m (99mTc). Brazil, though having a nuclear research reactor does not produce 99mTc. Four countries (Argentina, Brazil, Cuba, and Mexico) assemble molybdenum-99 (99Mo)-99mTc generators, using either imported or in situ production 99Mo, which is the case in Argentina. Brazil is the major generator manufacturer in the region. Countries with no generator production import from other LAC countries, the U.S. or Europe.9
Cold kits are produced by public or private institutions in Argentina, Brazil, Chile, Cuba, Mexico and Peru, and Uruguay. Most manufacturers commercialize these kits locally in their own countries as well as in the rest of the region. Of the 19 types of cold kits produced in the region, methoxyisobutylisonitrile (MIBI) accounts for 15% and pyrophosphate for 4%.9
There are 35 operative cyclotrons in the region, with a 300% growth of installed capacity between 2006 and 2013, mainly for the production of fluorine-18 (18F).
Types of Cardiac Studies
Data compiled during the first coordination meeting of the IAEA regional project for CVDs in the 16 participating countries show that there is some variability regarding the types of cardiac studies and stress protocols applied (Figure 4). As a summary, about 80% of studies performed are gated SPECT MPI; less than 10% are multi-gated acquisition (MUGA), mainly for evaluation of cardiac toxicity in cancer patients, and the remaining 10% corresponds to other type of procedures, such as detection of viability, adrenergic innervation studies with 123I-MIBG, rest gated SPECT in patients with dilated cardiomyopathy (including intraventricular synchronism assessment), and to evaluate acute chest pain in patients with normal or inconclusive electrocardiograms in the emergency room. Ecuador is the country with the highest proportion of MUGA studies performed (70%), while Cuba is the country with the highest number of viability studies (23%). Cardiac PET studies are still uncommon, both for viability and perfusion/myocardial blood flow measurement. Mexico is the country with the highest number of cardiac PET studies.
In general, physical stress is preferred when possible according to the clinical condition of the patient. Some countries do not use pharmacological stress protocols due to high costs or lack of availability of pharmacologic stress agents. In some countries like Costa Rica and Panama, adenosine is used, although the vast majority prefers dipyridamole.
Manpower and Training
There are approximately 1389 nuclear medicine physicians and 1695 technologists in the region, with an average of 1.1 physicians (range: 0.6-2.3), and 1.3 technologists per camera (range: 0.4-6.2), respectively (Figure 5).
University-accredited programs for nuclear medicine physicians are available in Argentina, Brazil, Colombia, Chile, Mexico, Peru, Dominican Republic, Uruguay, and Venezuela, conferring a specialization degree or diploma in nuclear medicine, sometimes within a larger training scheme, such is the case in Venezuela where the training encompasses nuclear medicine and radiation oncology. The programs vary in duration, content, and professional requirements from country to country. In some countries, nuclear medicine can be considered as a primary specialization, while in others, it is a subspecialty of internal medicine or radiology. Some nuclear medicine physicians working in nuclear cardiology hold another specialty, most frequently cardiology or internal medicine.
Availability of training programs for technologists also varies among countries of the region. Formal university degrees can be obtained in Argentina, Brazil, Chile, Costa Rica, Cuba, Mexico, and Uruguay.13 The training does not only address nuclear medicine, but also covers other areas of radiation medicine such as radiology and radiation oncology. Uruguay is the only country in the region with a specific university degree for nuclear medicine technologists.
The number of formally trained technologists does not meet the demand, and many positions are occupied by personnel with training in other biomedical-related areas.9 To help with this problem, common to many Member States, the IAEA has introduced a worldwide Distance-Assisted Training (DAT) program for nuclear medicine technologists, which is a comprehensive online set of training resources covering basic sciences and clinical applications, with special attention on SPECT-CT and PET-CT.13 The program (originally in English) has been translated into Spanish and partially into Portuguese and is accessible to all countries in the region. Over 1000 trainees have benefited from the DAT program in the region, and currently more than 200 students from 12 countries are actively enrolled.
There is a shortage of medical physicists and radiopharmacists in the region. Only 12 out of the 21 countries included in the general analysis have medical physicists working in nuclear medicine practices, with 0.1 medical physicists per center (Figure 6). Argentina, Brazil, Cuba, and Venezuela are the countries with the largest number of physicists. Some countries have postgraduate training programs in medical physics, namely Argentina, Brazil, Chile, Costa Rica, Cuba, Colombia, Mexico, and Venezuela, including Masters or PhD degrees. Availability of training programs has increased in the last few years, but the number of graduates still does not cover the needs.9
There are approximately 122 radiopharmacists/radiochemists in 11 countries of the region (0.1 radiopharmacists/radiochemists per center) (Figure 6). Some countries have university programs as in the case of Argentina, Brazil, Costa Rica, Cuba, Mexico and Uruguay, with graduates having access to Masters or PhD degrees.9
Professionals working in the field of nuclear medicine in countries without established training programs have received their training abroad.
Besides national training programs, all professionals involved in the practice of nuclear medicine benefit from many educational opportunities through activities organized or sponsored by the IAEA, as well as by local or regional scientific societies and organizations, such as the Latin American Association of Biology and Nuclear Medicine Societies (ALASBIMN) and the American Society of Nuclear Cardiology (ASNC).
Hurdles and Solutions on Regional Basis
In the Latin American and Caribbean region, the development of nuclear cardiology studies and other advanced imaging modalities are hampered by many factors including high cost of equipment, lack of equipment maintenance and service, as well as insufficient cardiac-specific training and, in some cases, lack of awareness of cardiologists or other referring physicians on the clinical applications of nuclear cardiology.14
It is particularly important to include training in hybrid imaging (SPECT-CT and PET-CT), as well as in cardiac CT. Critical components of the training for physicians dedicated to nuclear cardiology should include not only image interpretation skills and pathophysiologic knowledge, but also physics, radiopharmacy, and quality assurance. In this sense, there is a need of a broad participation of professionals involved in nuclear cardiology in training programs, certification courses, fellowships, and seminars, where the support of IAEA, ALASBIMN, and ASNC, as well as the national societies, is of crucial importance. Distance-assisted learning is a very cost-effective option.
Another hurdle to overcome is related to equipment and ensuring the stable supply of radioisotopes/radiopharmaceuticals, both for SPECT and PET studies. In this line, programs that could make isotopes, drugs, and equipment available at a lower cost for LMICs have been proposed,14 but further work is needed to completely set them up.
PET applications in cardiology should be made available in the region, not only for viability assessment purposes with 18F-FDG, but also for myocardial blood flow evaluation for the detection of multivessel disease and microvascular angina.
Increased awareness on the clinical application of nuclear cardiology among end-users is also needed including appropriateness criteria. In this line, inclusion of devoted lectures on nuclear cardiology in national, regional, and international congresses of internal medicine and cardiology, among others, can contribute to raising awareness on the clinical value of nuclear cardiology studies.
In the region, patients with stable IHD frequently undergo revascularization without prior functional assessment.15 Given that nuclear cardiology is an excellent tool for appropriate selection of such treatment options, this provides a great incentive to integrate and strengthen the practice of nuclear cardiology in the LAC region.
Interestingly, the introduction of the computed coronary tomography angiography has not significantly affected the utilization of nuclear cardiology in this part of the world, pointing to the fact that these techniques are more often complimentary than competitive.6,16
Finally, with constant advances in many medical imaging techniques and their applications in the field of cardiology as well as due to growing availability of multimodality cardiac imaging, it is imperative to carefully evaluate and select the most appropriate study e.g., SPECT, PET, cardiac computed tomography angiography, and cardiac magnetic resonance imaging, to be performed in each individual patient in order to optimize diagnosis, risk stratification, and ischemia-guided therapies in IHD patients.
The increase in number of centers and equipment available in the region, with a clear trend towards the modernization of existing infrastructure, as well the significant number of well-qualified, highly competent experts, and high level university training centers able to provide specialized education can be considered as a strength. Moreover, in some countries, there is governmental support for the use of nuclear techniques and they are incorporated into healthcare systems.17 The abovementioned strengths are reinforced through horizontal cooperation among countries, especially in the development of human resources and the supply of consumables and radiotracers.9
Conclusions
Latin America and the Caribbean region is experiencing a great burden of CVDs, which account for the highest proportional mortality in the region. Nuclear cardiology is instrumental to address this health challenge. In light of the ever increasing number of facilities and the improvement in the training of professionals involved in the clinical practice, the future of nuclear cardiology in the region is encouraging. National, regional, and international cooperation including support from scientific professional societies such as ASNC and ALASBIMN and organizations such as IAEA, as well as governmental commitment are key factors for further strengthening the practice of nuclear cardiology. This strengthening of nuclear cardiology practice may serve as part of overall efforts to tackle the burden of CVDs in the region.
Abbreviations
- ALASBIMN:
-
Latin American Association of Biology and Nuclear Medicine Societies
- ASNC:
-
American Society of Nuclear Cardiology
- CABG:
-
Coronary artery bypass grafting
- CT:
-
Computed tomography
- CVD:
-
cardiovascular disease
- DAT:
-
Distance-Assisted Training
- 18F:
-
Fluorine-18
- FDG:
-
Fluor-deoxy-glucose
- IAEA:
-
International Atomic Energy Agency
- IHD:
-
Ischemic heart disease
- 123I:
-
Iodine-123
- LAC:
-
Latin America and the Caribbean
- LMIC:
-
Low- and middle-income country
- MIBG:
-
Metaiodobenzylguanidine
- MIBI:
-
Methoxyisobutylisonitrile
- 99Mo:
-
Molybdenum-99
- MPI:
-
Myocardial perfusion imaging
- MUGA:
-
Multi-gated acquisition
- NUMDAB:
-
Nuclear Medicine Database
- OMT:
-
Optimal medical treatment
- PCI:
-
Percutaneous coronary intervention
- PET:
-
Positron emission tomography
- SPECT:
-
Single-photon emission tomography
- WHO:
-
World Health Organization
References
Organización Panamericana de la Salud/Organización Mundial de la Salud/Información y Análisis de Salud: Situación de Salud en las Américas: Indicadores Básicos 2015. Washington, DC; 2015.
Global Health Observatory Data Repository. Geneva: World Health Organization; 2013.
OPS. Salud en las Américas. Washington, DC: OPS; 2007, vol I, p. 132.
Global status report on noncommunicable diseases 2010. Geneva: World Health Organization; 2011.
Lanas F, Avezum A, Bautista L, Díaz R, Luna M, Islam S, et al. Risk factors for acute myocardial infarction in Latin America. The INTERHEART Latin American Study. Circulation. 2007;115:1067–74.
Vitola J. Nuclear Cardiology and CVD in the developing world—are we applying our scarce resources appropriately? Why is our mortality rate so high? Editorial. J Nucl Cardiol. 2016;. doi:10.1007/s12350-016-0562-8.
Underwood SR, Godman B, Salyani S, Ogle JR, Ell PJ. Economics of myocardial perfusion imaging in Europe—the EMPIRE study. Eur Heart J. 1999;20:157–66.
Shaw L, Hachamovitch R, Berman DS, Marwick TH, Lauer MS, Heller GV, et al. The economic consequences of available diagnostic and prognostic strategies for the evaluation of stable angina patients: An observational assessment of the value of precatheterization ischemia. J Am Coll Cardiol. 1999;33:661–9.
Paez D, Orellana P, Gutierrez C, Ramirez R, Mut F, Torres L. Current status of nuclear medicine practice in Latin America and the Caribbean. J Nucl Med. 2015;56:1629–34.
Dondi M, Kashyap R, Paez D, Pascual T, Zaknun J, Mut F, et al. Trends in nuclear medicine in developing countries. J Nucl Med. 2011;52:16S–23S.
Kashyap R, Dondi M, Paez D, Mariani G. Hybrid imaging worldwide: Challenges and opportunities for the developing world: A report of a technical meeting organized by the IAEA. Semin Nucl Med. 2013;43:208–23.
Paez D, Becic T, Bhonsle U, Jalilian AR, Nunez-Miller R, Osso JA. Current status of nuclear medicine practice in the Middle East. Semin Nucl Med. 2016;46:265–72.
Patterson HE, Nunez M, Philoteou GM, Hutton BF. Meeting the challenges of global nuclear medicine technologists training in the 21st century: The IAEA Distance Assisted Training (DAT) program. Semin Nucl Med. 2013;3:195–201.
Vitola JV, Shaw LJ, Allam AH, Orellana P, Peix A, Ellman A, et al. Assessing the need for nuclear cardiology and other advanced cardiac imaging modalities in the developing world. J Nucl Cardiol. 2009;16:956–61.
Cerci JJ, Trindade E, Preto D, Cerci RJ, Lemos PA, Cesar LA, et al. Investigation route of the coronary patient in the public health system in Curitiba, São Paulo and in InCor-IMPACT study. Arq Bras Cardiol. 2014;103:192–200.
Santos MA, Santos MS, Tura BR, Félix R, Brito AS, De Lorenzo A. Budget impact of applying appropriateness criteria for myocardial perfusion scintigraphy: The perspective of a developing country. J Nucl Cardiol. 2016;. doi:10.1007/s12350-016-0505-4.
Casas-Zamora JA, Kashyap R. The IAEA technical cooperation program and nuclear medicine in the developing world: Objectives, trends and contributions. Semin Nucl Med. 2013;43:172–80.
Acknowledgments
Participants in IAEA RLA 6078 project “Facing the high incidence of cardiovascular diseases in Latin America and the Caribbean through nuclear cardiology”: Roberto Aguero, MD (Nuclear Medicine Center, Buenos Aires, Argentina); Raul Araujo, MD (San Francisco Xavier de Chuquisaca University, Sucre, Bolivia); Jader Cunha de Azevedo, MD (Nuclear Medicine; Federal Fluminense University (UFF), Niteroi, Brazil); Pilar Orellana, MD (Nuclear Medicine Unit, Radiology Department, Pontificia Universidad Católica de Chile, Santiago, Chile); Claudia Gutierrez, MD (Cardiology Institute, Fundación Cardioinfantil, Bogotá, Colombia); María Isabel Berrocal, MD (San Juan de Dios Hospital, Caja Costarricense de Seguro Social, San Jose, Costa Rica); Amalia Peix, MD (Nuclear Medicine Department, Institute of Cardiology, Havana, Cuba); Alfredo Perez, MD (National Cancer Institute Rosa Emilia Sánchez de Tavares, Santo Domingo, Dominican Republic); Mayra Sanchez, MD (Carlos Andrade Marin Hospital, Quito, Ecuador); Erick Alexanderson, MD (National Heart Institute Ignacio Chavez, Mexico DF, Mexico); Teresa Cuadra, MD (National Center of Radiotherapy, Managua, Nicaragua); Yariela Herrera, MD (Santo Tomas Hospital, Panama City, Panama); Angel Jose Ortellado, MD (National Institute of Cardiovascular Prevention-INPCARD, Asuncion, Paraguay); Aurelio Mendoza, MD (Cardiovascular National Institute-INCOR, Lima, Peru; Fernando Mut, MD (Nuclear Medicine Service, Asociación Española, Montevideo, Uruguay); Carlos Castellanos, MD (Dr Carlos Arvelo Hospital, Caracas, Venezuela).
Disclosure
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Paez, D., Peix, A., Orellana, P. et al. Current status of nuclear cardiology practice in Latin America and the Caribbean. J. Nucl. Cardiol. 24, 308–316 (2017). https://doi.org/10.1007/s12350-016-0650-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0650-9