Abstract
Purpose
Adaptive servo-ventilation (ASV) therapy has been reported to be effective for improving central sleep apnea (CSA) and chronic heart failure (CHF). The purpose of this study was to clarify whether ASV is effective for CSA, cardiac sympathetic nerve activity (CSNA), cardiac symptoms/function, and exercise capacity in CHF patients with CSA and Cheyne-Stokes respiration (CSR-CSA).
Methods
In this study, 31 CHF patients with CSR-CSA and a left ventricular ejection fraction (LVEF) ≤ 40% were randomized into an ASV group and a conservative therapy (non-ASV) group for 6 month. Nuclear imagings with 123I-Metaiodobenzylguanidine (MIBG) and 99mTc-Sestamibi were performed. Exercise capacity using a specific activity scale (SAS) and the New York Heart Association (NYHA) class were evaluated. CSNA was evaluated by 123I-MIBG imaging, with the delayed heart/mediastinum activity ratio (H/M), delayed total defect score (TDS), and washout rate (WR).
Results
The ASV group had significantly better (P < .05) results than the non-ASV group with respect to the changes of AHI (−20.8 ± 14.6 vs −0.5 ± 8.1), TDS (−7.9 ± 4.3 vs 1.4 ± 6.0), and H/M(0.16 ± 0.16 vs −0.04 ± 0.10) on 123I-MIBG imaging, as well as the changes of LVEF (5.3 ± 3.9% vs 0.7 ± 32.6%), SAS (1.6 ± 1.4 vs 0.3 ± 0.7), and NYHA class (2.2 ± 0.4 vs 2.7 ± 0.5) after 6-month therapy.
Conclusions
Performing ASV for 6 months achieved improvement of CSR-CSA, CSNA, cardiac symptoms/function, and exercise capacity in CHF patients with CSR-CSA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prognosis of patients with chronic heart failure (CHF) remains poor. Activation of the sympathetic nervous system is one of the prominent cardiac pathophysiologic abnormalities in patients with CHF.1
Cheyne-Stokes respiration and central sleep apnea (CSR-CSA) occur in some patients with left ventricular dysfunction and are indicators of a poor prognosis, being associated with a higher mortality than in CHF patients without CSR-CSA matched for age, sex, and ejection fraction.2,3 CSR-CSA causes an increase of sympathetic nerve activity that maintains afterload at a high level4 but elevation of afterload leads to further reduction of the left ventricular ejection fraction (LVEF).
123I-Metaiodobenzylguanidine (MIBG) imaging has been used to study cardiac sympathetic nerve activity. Uptake of 123I-MIBG by the heart is altered in patients with CHF compared to normal individuals.5,6 Because cardiac uptake of 123I-MIBG is correlated with the LVEF,5,6 123I-MIBG imaging can be a useful prognostic marker in patients with CHF.6 ADMIRE-HF provides prospective validation of the independent prognostic value of 123I-MIBG scintigraphy in assessment of patients with HF.7
There have been no data about whether ASV can stabilize cardiac sympathetic nerve activity in CHF patients with CSR-CSA. The aim of the present study is to clarify whether ASV can stabilize cardiac sympathetic nerve activity in CHF patients with CSR-CSA, and then improve cardiac symptoms/function, and exercise capacity compared with conventional treatment in CHF patients with CSR-CSA.
Methods
Study population
Between 2008 and 2011, 31 consecutive patients (2 women and 29 men with a mean age of 68 ± 9 years, range: 42 to 82 years) with dilated cardiomyopathy (DCM) or ischemic cardiomyopathy (ICM) and CSR-CSA were assigned to groups with or without ASV (HEART PAP, Respironics) in addition to conventional treatment for heart failure that included β-blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, diuretics, aldosterone blockers, and anti arrythmic drugs. All patients had experienced at least one episode of heart failure requiring short-term hospitalization. All patients were symptomatic at the start of treatment, being in New York Heart Association (NYHA) functional Class II or III and having an LVEF ≤ 40% by quantitative gated SPECT (QGS). The following patients were excluded: (1) patients with CHF due to organic valvular heart disease; (2) patients with chronic pulmonary disease; (3) patients on dialysis; and (4) patients with a history of stroke and neurological deficits. After at least 3 months of optimal medical treatment, patients were randomized to the ASV or non-ASV groups. Of the 31 patients, 16 were allocated to the ASV group and 15 to the non-ASV group. One patient in the ASV group withdrew from the study for personal reasons and failed to complete the trial, leaving 30 patients available for analysis. All patients gave informed consent in accordance with the guidelines of the Human Clinical Study Committee of our hospital prior to participation in the study.
Polysomnography
Patients underwent overnight attended polysomnography using a computerized system (Alice PDx; Respironics; Murrysville, PA, USA) that automatically recorded and analyzed the electroencephalogram, electrooculogram, electromyogram, and electrocardiogram. Air flow from the nose or mouth was recorded with a thermistor, while thoracic and abdominal wall motion were monitored by plethysmography. Arterial oxygen saturation (SaO2%) was measured transcutaneously by pulse oximetry. Hypopnea was defined as a fall in oronasal air flow ≥30% of baseline for more than 10 seconds associated with a decrease of SaO2% by ≥3%. Apnea was defined as the absence of oronasal air flow for the same period. The number of episodes of apnea and hypopnea per hour was calculated as the apnea-hypopnea index (AHI), and patients with an AHI ≥ 5/h were classed as having significant sleep apnea syndrome. CSR-CSA was defined as follows: (1) at least 3 consecutive cycles of a cyclic crescendo-decrescendo change in breathing and an AHI ≥ 5/h, or (2) persistence of a cyclic crescendo-decrescendo breathing pattern for at least 10 consecutive minutes.8,9 The follow-up AHI data were taken from ASV device in ASV group and second PSG in non-ASV group.
ASV treatment
The principles of flow-triggered ASV have been described previously.10-12 It provides a manually set level of expiratory positive airway pressure (EPAP) to maintain upper airway patency and automatically modulates the inspiratory positive airway pressure (IPAP) within a preset range to maintain a target inspiratory airflow, thereby eliminating CSA events. In addition, the device provides an automatic back-up rate when sustained apnea is detected. EPAP was automatically titrated to the effective pressure over a range from 4 cm H2O to the maximum of 10 cm H2O. Minimum IPAP was set at the same level as EPAP or 2 cm H2O higher in patients with obstructive flow limitation, while maximum IPAP was set at 10 cm H2O above minimum IPAP. In addition, an automatic back-up rate was initially set for all subjects. When central apnea was not corrected, the automatic back-up rate was changed to a fixed back-up rate of 10/min or more.
123I-MIBG and 99mTc-MIBI imagings
123I-MIBG and 99mTc-Sestamibi (MIBI) were obtained commercially (FUJIFILM RI Pharma, Tokyo, Japan). Patients were injected intravenously with 111 Mbq of 123I-MIBG. Anterior planar images and single-photon emission computed tomography (SPECT) images were acquired both 15 minutes after injection and 4 hours later. SPECT imaging was performed using a dedicated 3-detector system (IRIX, PICKER Cleveland, OH) with low-energy, all-purpose resolution, parallel-hole collimators. The detectors were constantly corrected for energy, uniformity, and linearity. Projection images were acquired for 55 seconds in 5° increments over a 360° orbit and were recorded at a digital resolution of 64 × 64 pixels. On a different day, patients were injected with 740 MBq of 99mTc-MIBI at rest and imaging was done 30 minutes later to evaluate myocardial perfusion and cardiac function. 99mTc-MIBI SPECT images were acquired for 40 seconds in 5° increments over a 360° orbit. Energy discrimination was provided by a 20% window around the 159 keV photopeak of 123I-MIBG and a 15% window around the 140 keV photopeak of 99mTc-MIBI.
On the anterior planar delayed 123I-MIBG images, the heart-to-mediastinum (H/M) activity ratio was obtained by placing a region of interest (ROI) over the heart (H) and over the upper mediastinum (M). The ROI over the heart included the blood pool. The washout rate was calculated using the formula: (H-M)early − (H-M)delayed/(H-M)early × 100. We used the delayed H/M activity ratio and delayed TDS. (The institutional normal H/M ratio was 2.32 ± 0.19 and the washout rate was 28.1 ± 7.0%.)
The myocardial SPECT image was evaluated according to the previous report.13 Then regional uptake was assessed semiquantitatively using a five-point score (0 = normal uptake; 1 = slightly reduced uptake; 2 = moderately reduced uptake; 3 = severely reduced uptake; and 4 = absent uptake). The total defect score was calculated as the sum of the scores for all 17 segments. We defined the difference between delayed 123I-MIBG and 99mTc-MIBI SPECT defect scores as the mismatch score. The total mismatch score (TMS) was calculated as the sum of the mismatch scores. TMS was calculated as TDS (delayed 123I-MIBG) minus TDS (99mTc-MIBI).
Commercially available quantitative gated SPECT (QGS) software (Cedars-Sinai Medical Center, Los Angeles, CA) with a temporal resolution of 16 frames per RR interval was used to create a 3-dimensional surface cinemode display. Then this display was employed to calculate the LVEF, left ventricular end-diastolic volume (LVEDV), and left ventricular end-systolic volume (LVESV) throughout the cardiac cycle using an automatic edge detection algorithm.14
Cardiac symptoms and exercise capacity
Cardiac symptoms were assessed using the NYHA functional classification. Exercise capacity was estimated using the specific activity scale (SAS), with all patients being asked 21 questions at the beginning of this study and after 6 months of therapy.15
Statistical analysis
All examinations were performed and evaluated by researchers who had no information about which group the patients were enrolled in. Statistical analysis was done with JMP software (SAS Institute Inc., Cary, NC). Comparisons of parameters were performed using paired two-tailed t-tests, while the unpaired two-tailed t test was used for comparison between the ASV and non-ASV groups. Results are expressed as the mean ± SD.
Results
Patient characteristics
Both groups were well matched for baseline characteristics (Table 1). Fifteen patients (2 women and 13 men with a mean age of 69 ± 9 years) received ASV and 15 patients (all men with a mean age of 68 ± 10 years) did not receive ASV. During the study period, no changes were made to their baseline medications, including β-blockers, ACE inhibitors/ARBs, diuretics, aldosterone blockers, and antiarrhythmic drugs. There were no significant differences of age, gender, body mass index, NYHA functional class, LVEF, and medications between the 2 groups. Atrial fibrillation was present in 7 patients (44%) from the ASV group and 2 patients (13%) from the non-ASV group. Cardiac resynchronization therapy was performed in 2 patients (13%) from the ASV group.
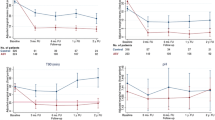
Polysomnography data and the change of apnea-hypopnea-index
Polysomnography data are summarized in Table 2. The baseline AHI and arousal index were comparable between the ASV and non-ASV groups. In the ASV group, the AHI decreased significantly from baseline to 6 months of therapy (from 25.5 ± 14.7 to 4.7 ± 2.8, P = .0002), but it did not change in the non-ASV group. The change of AHI of the ASV group was significantly different to that of the non-ASV group (−20.8 ± 14.6 vs −0.5 ± 8.1/h; P = .0003, Figure 1).
Total Defect Score and the H/M ratio of the 123I-MIBG images
The total defect scores obtained from delayed 123I-MIBG images are summarized in Table 3. In the non-ASV group, the total defect score did not change significantly after 6 months of therapy (36 ± 11) in comparison with the baseline value (35 ± 13). In the ASV group, however, the total defect score decreased significantly after 6 months in comparison with baseline (from 35 ± 13 to 27 ± 13, P < .01). The defect score of the ASV group after treatment was significantly lower than that of the non-ASV group (P < .05). In addition, the change of TDS of the ASV group was significantly lower than that of the non-ASV group (−7.9 ± 4.3 vs 1.4 ± 6.0, P < .0001, Figure 2).
The H/M ratios obtained from delayed 123I-MIBG images are summarized in Table 3. In the non-ASV group, the H/M ratio did not change significantly after 6 months of therapy (1.53 ± 0.17) in comparison with the baseline value (1.57 ± 0.18). In the ASV group, however, the H/M ratio increased significantly after treatment in comparison with baseline (from 1.54 ± 0.19 to 1.70 ± 0.24, P < .01). The H/M ratio of the ASV group after 6 months of therapy was significantly higher than that of the non-ASV group (P < .05). Moreover, the change of H/M ratio of the ASV group was significantly higher than that of the non-ASV group (0.16 ± 0.16 vs −0.04 ± 0.10, P = .0003, Figure 3).
Washout Rate and the change of Washout Rate on 123I-MIBG images
Washout rates obtained from the 123I-MIBG images are also summarized in Table 3. In the non-ASV group, the washout rate did not change significantly after 6 months of therapy (51 ± 9%) in comparison with baseline (50 ± 11%). However, the washout rate of the ASV group decreased significantly after treatment in comparison with baseline (from 53 ± 9% to 44 ± 15%, P < .05).
Total Defect Score on 99mTc-MIBI images
The total defect scores obtained from 99mTc-MIBI images are summarized in Table 3. In the non-ASV group, the total defect score did not change significantly after treatment (from 10 ± 6 to 10 ± 7). In the ASV group, the total defect score decreased significantly after treatment (from 15 ± 13 to 12 ± 12, P < .05).
Total Mismatch Score between the 123I-MIBG images and the 99mTc-MIBI images
The total mismatch scores between delayed 123I-MIBG images and 99mTc-MIBI images are summarized in Table 3. In the non-ASV group, the total mismatch score did not change significantly after 6 months of therapy (26 ± 12) in comparison with the baseline value (24 ± 13). In the ASV group, however, the total mismatch score decreased significantly after 6 months in comparison with the baseline (from 20 ± 13 to 15 ± 10, P < .01). The defect score of the ASV group after treatment was significantly lower than that of the non-ASV group (P < .05).
LVEDV, LVESV, and LVEF on QGS images
The baseline LVEF, LVEDV, and LVESV were compared with those after 6 months of therapy (Table 4). In the ASV group, LVEF and ESV improved significantly after treatment from 26 ± 9% and 178 ± 67 ml to 31 ± 10% (P < .01) and 157 ± 65 ml (P < .05), respectively. In addition, the change of LVEF (5.3 ± 3.9%) of the ASV group was significantly higher than that of the non-ASV group (0.7 ± 2.6%; P = .0009, Figure 4).
Functional capacity
Changes of the NYHA functional class are summarized in Table 4. The non-ASV group did not show any improvement of functional class after 6 months of therapy in comparison with baseline (from 2.8 ± 0.4 to 2.7 ± 0.5). In contrast, the ASV group showed an improvement of NYHA functional class after treatment compared with baseline (from 2.8 ± 0.4 to 2.2 ± 0.4, P = .003). The NYHA class of the ASV group was significantly lower than that of the non-ASV group after treatment for 6 months (P = .026, Figure 5).
Changes of the SAS are summarized in Table 4. In the non-ASV group, the SAS did not increase significantly after 6 months of therapy (4.2 ± 0.9 METs) in comparison with its baseline value (3.9 ± 0.9 METs). In the ASV group, however, the SAS increased significantly after 6 months of therapy in comparison with its baseline value (from 3.4 ± 1.1 METs to 5.0 ± 1.0 METs, P < .01). The SAS of the ASV group was significantly higher than that of the non-ASV group after treatment (P < .05). Moreover, the change of SAS of the ASV group was significantly higher than that of the non-ASV group (1.6 ± 1.4 METs vs 0.3 ± 0.7 METs, P = .004, Figure 6). Figures 7 and 8 show representative cases from the non-ASV group and the ASV group, respectively.
Representative case from the non-ASV therapy group. 123I-metaiodobenzylguanidine (MIBG) images obtained from short-axis and vertical long-axis reconstructions. 123I-MIBG uptake decreased in all segments at the beginning, but was unchanged after 6 months. TDS changed from 22 to 27, H/M ratio changed from 1.46 to 1.49, and WR changed from 56% to 50%. These parameters remained unchanged after 6 months of therapy
Discussion
In the present study, performing ASV for 6 months led to a significant decrease of the AHI in CHF patients with CSR-CSA, in whom the functional capacity, exercise tolerance, and LVEF all increased, while cardiac sympathetic nerve activity was suppressed. There have been several previous clinical studies of ASV therapy for CHF and CSR-CSA. Oldenburg et al reported that ASV therapy decreased the AHI from 37.4 ± 9.4 to 9.4 ± 4.1/h of sleep.16 Similarly, Kasai et al reported that the AHI decreased from 37.4 ± 19.5 to 1.9 ± 2.1/h with ASV.17 The present study confirmed that the effectiveness of ASV therapy for CHF patients with CSR-CSA was sustained for at least 6 months in terms of the improvement of functional capacity, cardiac function, and cardiac sympathetic nerve activity as well as AHI.
In previous studies, sympathetic nerve activity has been estimated from plasma or urine norepinephrine concentrations in CHF patients with CSR-CSA.4 Staniforth et al reported that home oxygen therapy reduced the frequency of Cheyne-Stokes respiration and reduced overnight urinary excretion of noradrenaline in patients with CHF and CSR-CSA.4 They concluded that home oxygen therapy stabilized Cheyne-Stokes respiration and improved sympathetic nerve activity. However, there have been no data about whether ASV can stabilize cardiac sympathetic nerve activity in CHF patients with CSR-CSA. In the present study, we evaluated cardiac sympathetic nerve activity using 123I-MIBG scintigraphy. Myocardial scintigraphy with 123I-MIBG, an analog of norepinephrine, has been reported to provide images that reflect cardiac sympathetic nerve function,5,6 and assessing 123I-MIBG uptake is considered useful for evaluating the severity of heart failure.6,18 In addition, the H/M ratio, total defect score, and washout rate can be obtained from 123I-MIBG images to predict the prognosis and evaluate the efficacy of treatment.6,18-20
In the present study, improvement of the TDS, H/M ratio, and washout rate obtained from 123I-MIBG imaging was more marked in patients receiving ASV therapy than in patients who did not receive ASV. These results suggest that the improvement of CSR-CSA by ASV led to a decline of sympathetic nerve activity. Because elevated sympathetic nerve activity is a poor prognostic feature in CHF patients,21 improvement of sympathetic nerve activity is associated with lower mortality.22 Thus, performing ASV therapy in patients with CHF and CSR-CSA may have important implications for the treatment of CHF. There have been no previous reports that ASV directly improves sympathetic nerve activity in CHF patients with CSR-CSA. However, our data show that ASV can improve CSR-CSA in CHF patients. The mechanism underlying CSR-CSA has been postulated to involve upregulation of both central23-26 and peripheral23 chemoreceptors, which is thought to be due to elevation of circulating catecholamine levels.27 Mansfield et al28 supported the concept that heart failure is primarily responsible for the development of CSR-CSA in CHF patients, with the increase of sympathetic nerve activity and upregulation of chemosensitivity being secondary changes. ASV therapy can also stabilize sympathetic nerve activity and this effect could promote the improvement of cardiac symptom, cardiac function, and exercise capacity in CHF patients with CSR-CSA.
CRT was implanted in two patients in our study. In the previous study, CRT was reported to improve cardiac sympathetic nervous dysfunction in responder heart failure patients 6 months after CRT.29 However, CRT was already implanted over 6 months before our ASV study. Accordingly, the results of cardiac 123I-MIBG uptake were less affected by CRT.
The delayed normal H/M ratio in our institute was 2.32 ± 0.19, which was similar to 2.49 ± 0.25 evaluated from Japanese normal databases for myocardial 23I-MIBG imaging using LE collimeter.30 The H/M ratio of 123I-MIBG showed variations among institutions and needs to be standardized among various scinticamera-collimator combinations. In Nakajima’s research, a total of 225 phantom experiments were performed in 84 institutions in Japan to calculate cross-calibration coefficients of H/M ratio. The average conversion coefficients from the individual camera-collimator condition to the mathematically calculated reference H/M ratio ranged from 0.55 to 0.75 for low-energy groups and from 0.83 to 0.95 for medium-energy groups. The conversion coefficient of 0.88 was used to unify H/M ratios from all acquisition conditions. Using the reference H/M ratio and conversion coefficients for the system, H/M ratios with various conditions can be converted to the standard H/M ratios in a range of normal to low H/M ratios.31
In our study, there was no significant difference in the rate of non-ischemic or ischemic patients and myocardial perfusion damage calculated by 99mTc-MIBI perfusion imaging before study. TDS of ASV group improved after ASV treatment, but not in non-ASV group. The LV volume decreased after treatment in only ASV group. This finding could improve the quality of myocardial perfusion and decrease TDS.
The ASV usage improved chronic heart failure and cardiac sympathetic nerve function, which connected to the improvement of not only cardiac function and symptom, but also exercise capacity evaluated by SAS.
We used the low dose of 111 Mbq for 123I-MIBG imaging. Imaging quality was good enough to evaluate. That dose was supported by Japanese national insurance.
However, several limitations of this study need to be considered. First, because of the small number of patients enrolled, it was difficult to sufficiently evaluate the effectiveness of ASV for patients with CHF and CSR-CSA. Second, the duration of ASV therapy was relatively short. In the future, we need to study the long-term effects of ASV in a larger number of patients.
In conclusion, performing ASV therapy for 6 months was effective for improving CSR-CSA, and stabilized cardiac sympathetic nerve activity, which promoted the improvement of cardiac symptoms/function, and exercise capacity in CHF patients with CSR-CSA.
New Knowledge Gained
There have been no data about whether ASV can stabilize cardiac sympathetic nerve activity in CHF patients with CSR-CSA. Improvement of cardiac sympathetic nerve activity evaluated by 123I-MIBG imaging was obtained markedly in patients receiving ASV therapy. ASV therapy can stabilize sympathetic nerve activity and this effect could promote the improvement of cardiac symptom, cardiac function, and exercise capacity in CHF patients with CSR-CSA.
Abbreviations
- ASV:
-
Adaptive servo-ventilation
- CSA:
-
Central sleep apnea
- CHF:
-
Chronic heart failure
- CSNA:
-
Cardiac sympathetic nerve activity
- LVEF:
-
Left ventricular ejection fraction
- MIBG:
-
123I-Metaiodobenzylguanidine
- NYHA:
-
New York Heart Association
- H/M:
-
Heart/mediastinum activity ratio
- TDS:
-
Total defect score
- WR:
-
Washout rate
References
Thomas JA, Marks BH. Plasma norepinephrine in congestive heart failure. Am J Cardiol 1978;41:233–43.
Lanfranchi PA, Braghiroli A, Bosimini E, Mazzuero G, Colombo R, Donner CF, et al. Prognostic value of nocturnal Cheyne-Stokes Respiration in chronic heart failure. Circulation 1999;99:1435–40.
Hanly PJ, Zuberi-Khokhar NS. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med 1996;153:272–6.
Staniforth AD, Kinnear WJ, Starling R, Hetmanski DJ, Cowley AJ. Effect of oxygen on sleep quality, cognitive function and sympathetic activity in patients with chronic heart failure and Cheyne-Stokes respiration. Eur Heart J 1998;19:922–8.
Schofer J, Spielmann R, Schbert A, Weber K, Schluter M. Iodine-123 metaiodobenzylguanidine scintigraphy: A noninvasive method to demonstrate myocardial adrenergic system disintegrity in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol 1988;12:1252–8.
Merlet P, Valette H, Dubois-Randé JL, Moyse D, Duboc D, Dove P, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med 1992;33:471–7.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF. J Am Coll Cardiol 2010;55:2212–21.
Sleep-related breathing disorders in adults: Recommendation for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999;22:667–89.
Silber MH, Ancoli-Israel S, Bonnet MH, Chokroverty S, Grigg-Damberger MM, Hirshkowitz M, et al. The visual scoring of sleep in adults. J Clin Sleep Med 2007;3:121–31.
Kasai T, Narui K, Dohi T, Takaya H, Yanagisawa N, Dungan G, et al. First experience of using new adaptive servo-ventilation device for Cheyne-Stokes respiration with central sleep apnea among Japanese patients with congestive heart failure. Circ J 2006;70:1148–54.
Arzt M, Wensel R, Montalvan S, Schichtl T, Schroll S, Budweiser S, et al. Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest 2008;134:61–6.
Randerath WJ, Galetke W, Stieglitz S, Laumanns C, Schäfer T. Adaptive servo-ventilation in patients with coexisting obstructive sleep apnoea/hypopnoea and Cheyne-Stokes respiration. Sleep Med 2008;9:823–30.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539–42.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138–47.
Sasayama S, Asanoi H, Kihara Y, Yokawa S, Terada Y, Yoshida S, et al. Clinical effects of long-term administration of pimobendan in patients with moderate congestive heart failure. Heart Vessels 1994;9:113–20.
Oldenburg O, Schmidt A, Lamp B, Bitter T, Muntean BG, Langer C, et al. Adaptive servoventilation improves cardiac function in patients with chronic heart failure and Cheyne-Stokes respiration. Eur J Heart Fail 2008;10:581–6.
Kasai T, Usui Y, Yoshioka T, Yanagisawa N, Takata Y, Narui K, et al. Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and cheyne-stokes respiration. Circ Heart Fail 2010;3:140–8.
Toyama T, Aihara Y, Iwasaki T, Hasegawa A, Suzuki T, Nagai R, et al. Cardiac sympathetic activity estimated by 123I-MIBG myocardial imaging in patients with dilated cardiomyopathy after beta-blocker or angiotensin-converting enzyme inhibitor therapy. J Nucl Med 1999;33:217–23.
Imamura Y, Fukuyama T. Prognostic value of myocardial MIBG scintigraphy findings in patients with cardiomyopathy—importance of background correction for quantification of MIBG activity. Ann Nucl Med 2002;16:387–93.
Yamada T, Shimonagata T, Fukunami M, Kumagai K, Ogita H, Hirata A, et al. Comparison of the prognostic value of cardiac Iodine-123 metaiodobenzylguanidine imaging and heart rate variability in patients with chronic heart failure. J Am Coll Cardiol 2003;41:231–8.
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984;311:819–23.
Swedberg K, Eneroth P, Kjekshus J, Wilhelmsen L. Hormones regulating cardiovascular function in patients with severe congestive heart failure and their relation to mortality. CONSENSUS Trial Study Group. Circulation 1990;82:1730–6.
Solin P, Roebuck T, Johns DP, Walters EH, Naughton MT. Peripheral and central ventilatory responses in central sleep apnea with and without congestive heart failure. Am J Respir Crit Care Med 2000;162:2194–220.
Hall MJ, Xie A, Rutherford R, Ando S, Floras JS, Bradley TD. Cycle length of periodic breathing in patients with and without heart failure. Am J Respir Crit Care Med 1996;154:376–81.
Francis DP, Willson K, Davies C, Coats AJ, Piepoli M. Quantitative general theory for periodic breathing in chronic heart failure and its clinical implications. Circulation 2000;102:2214–21.
Javaheri S. A mechanism of central sleep apnea in patients with heart failure. N Engl J Med 1999;341:949–54.
Heistad DD, Wheeler RC, Mark AL, Schmid PG, Abboud FM. Effects of adrenergic stimulation on ventilation in man. J Clin Invest 1972;51:1469–75.
Mansfield D, Kaye DM, La Rocca HB, Solin P, Esler MD, Naughton MT. Raised sympathetic nerve activity in heart failure and central sleep apnea is due to heart failure severity. Circulation 2003;107:1396–400.
Shinohara T, Takahashi N, Saito S, Okada N, Wakisaka O, Yufu K, et al. Effect of cardiac resynchronization therapy on cardiac sympathetic nervous dysfunction and serum C-reactive protein level. Pacing Clin Electrophysiol 2011;34:1225–30.
Nakajima K. Normal values for nuclear cardiology: Japanese databases for myocardial perfusion, fatty acid and sympathetic imaging and left ventricular function. Ann Nucl Med 2010;24:125–35.
Nakajima K, Okuda K, Yoshimura M, Matsuo S, Wakabayashi H, Imanishi Y, et al. Multicenter cross-calibration of I-123 metaiodobenzylguanidine heart-to-mediastinum ratios to overcome camera-collimator variations. J Nucl Cardiol 2014;21:970–8.
Disclosure
The authors have indicated that they have no financial conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi: 10.1007/s12350-016-0584-2
Rights and permissions
About this article
Cite this article
Toyama, T., Hoshizaki, H., Kasama, S. et al. Adaptive servo-ventilation therapy improves cardiac sympathetic nerve activity, cardiac function, exercise capacity, and symptom in patients with chronic heart failure and Cheyne-Stokes respiration. J. Nucl. Cardiol. 24, 1926–1937 (2017). https://doi.org/10.1007/s12350-016-0529-9
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0529-9