Abstract
Background
In patients undergoing regadenoson SPECT myocardial perfusion imaging (MPI), it is unknown how soon and at which dose intravenous aminophylline can be administered to reverse regadenoson-related adverse effects without blunting stress-induced myocardial ischemia.
Methods and Results
We analyzed the pooled database of the ASSUAGE and ASSUAGE-CKD trials (n = 548). These were double-blinded, placebo-controlled, randomized clinical trials in which 75 mg of aminophylline or placebo was administered intravenously 90 seconds following 99mTc-tetrofosmin injection. There were no statistically significant differences in summed difference score (SDS) burden (P = .87) and in the rates of myocardial ischemia (SDS ≥ 2) (P = .93) between the aminophylline (n = 274) and placebo (n = 274) groups. There was no interaction between aminophylline use and SDS as a determinant of the composite endpoint of cardiac death or MI (P = .32) or the composite endpoint of cardiac death, MI, or coronary revascularization (P = .92).
Conclusion
In patients undergoing regadenoson-stress SPECT-MPI, the intravenous administration of 75 mg of aminophylline as early as 90 seconds after radioisotope injection does not seem to attenuate the burden of myocardial ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Regadenoson is a selective A2A adenosine receptor agonist used as vasodilator stress agent; it is utilized in nearly 80% of patients undergoing pharmacologic stress myocardial perfusion imaging (MPI) with single-photon emission computed tomography (SPECT).1-4 Like other vasodilator stress agents, regadenoson is commonly associated with adverse effects such as headache, flushing, and gastrointestinal symptoms. These side-effects can be effectively aborted with intravenous administration of aminophylline, a non-selective adenosine receptor antagonist.5,6 However, aminophylline also reverses adenosine receptor-mediated myocardial hyperemia. Therefore, if administered too soon after radioisotope injection, aminophylline may attenuate stress-induced perfusion abnormality.
In two double-blinded, placebo-controlled randomized clinical trials, the ASSUAGE and ASSUAGE-CKD,5,6 our group demonstrated that the routine intravenous administration of 75 mg of aminophylline 90 seconds following 99mTc-tetrofosmin injection (approximately 2 minutes following regadenoson) profoundly attenuates the incidence of regadenoson-related adverse effects.5,6 However, the impact of aminophylline administration, at this dose and timing, on the detectable burden of regadenoson-induced myocardial ischemia is not adequately studied. Given the myocardial uptake kinetics of SPECT-MPI radioisotopes,7 we hypothesize that administering aminophylline according to the ASSUAGE protocol does not significantly impact the burden of regadenoson-induced perfusion abnormality detected by SPECT-MPI.
Methods
We tested the study hypothesis in the pooled database of the ASSUAGE and ASSUAGE-CKD trials.5,6 Briefly, these are identically designed double-blinded, placebo-controlled randomized clinical trials, except that the ASSUAGE trial (n = 248) was open to all participants, irrespective of kidney function, while the ASSUAGE-CKD trial (n = 300) was limited to patients with severe chronic kidney disease (stage 4 or 5), defined as glomerular filtration rate < 30 mL·minute−1/1.73 m2 or dialysis therapy.5,6 The purpose of these trials was to investigate whether the administration of intravenous aminophylline following regadenoson in patients undergoing SPECT-MPI can attenuate the adverse effects associated with regadenoson. Patients were randomized in 1:1 ratio to receive 75 mg of intravenous aminophylline or a matching placebo, administered 90 seconds following 99mTc-tetrofosmin injection (approximately 2 minutes following regadenoson). Aminophylline or placebo were administered as a slow 30-second bolus. All patients signed informed and HIPAA consents. Both trials were registered on clincialtrials.gov (NCT01250496 and NCT01336140) and their findings were previously reported.5,6,8
SPECT Myocardial Perfusion Imaging
Image acquisition and analysis methods were detailed elsewhere.5,6,9-11 Briefly, MPI scans were analyzed using 4DM-SPECT software (INVIA—Ann Arbor, MI) by a single expert reader (AA) who was blinded to patients’ study assignment and clinical data. Using standard 17-segment model, quantitative and semi-quantitative summed stress scores (SSS), summed rest scores (SRS), and summed difference scores (SDS) were tabulated. Myocardial ischemia and abnormal MPI were defined as semi-quantitative SDS ≥ 2 and SSS ≥ 4, respectively. Scintigraphic evidence of myocardial infarction (MI) was defined as SRS ≥ 4. Quantitative defect size, as percentage of the left ventricular myocardium, and transient cavity dilation ratio from ungated SPECT-MPI were recorded. The post-stress change in left ventricular ejection fraction (LVEF), defined as stress minus rest LVEF by gated-SPECT, was calculated.
Follow-Up
Patients were prospectively followed for cardiac death, MI, and any post-MPI percutaneous or surgical coronary revascularization. Events were determined using chart review, social security death index, and death certificates by an adjudicator blinded to study arm, clinical data, and MPI findings. Detailed follow-up methods were reported elsewhere.9,10
Endpoints
The primary endpoint was the semi-quantitative SDS, as a measure of myocardial ischemic burden. The secondary endpoint was myocardial ischemia (SDS ≥ 2) by semi-quantitative analysis. Furthermore, we explored interactions between aminophylline use and SDS, and between aminophylline use and myocardial ischemia (SDS ≥ 2) as determinants of the composite endpoint of cardiac death or MI as well as the composite endpoint of cardiac death, MI, or coronary revascularization.
Statistical Analyses
Based on post hoc power analysis, the study has 80% power to detect an absolute 0.6-point difference in the mean SDS burden, assuming mean SDS of 1.5 ± 2.5, and 80% power to detect 33% difference in the rate of myocardial ischemia (SDS ≥ 2), assuming 30% prevalence of myocardial ischemia in the placebo arm (two-tailed α = 0.05).
The Chi-square test was used to compare dichotomous variables, which were expressed as frequencies and percentages. The Student’s t test was used to compare normally distributed continuous variables, which were expressed as means ± standard deviations. The Mann-Whitney test was used to compare skewed variables. The analysis of covariance (ANCOVA) method was used to study the impact of aminophylline on SDS and SSS, adjusting for relevant covariates. Multivariate logistic regression models were used to determine the association between aminophylline use and incidents of myocardial ischemia or abnormal MPI, adjusting for relevant covariates.
The log-rank test was used to compare unadjusted survival. Cox-logistic regression models were used to assess the impact of aminophylline use on event-free survival compared to placebo, adjusting for important clinical and imaging predictors of outcome, namely SDS (or ischemia), SRS, history of MI, and LVEF. In these models, we also explored interactions between SDS (or ischemia) and aminophylline use as a determinant of cardiac outcomes. Survival analyses treated the date of MPI as “time 0” and all patients were censored at their last encounter or at 46 months, whichever occurred first. In all analyses, two-tailed P values <.05 were considered statistically significant. All statistical analyses were performed using SPSS software package—version 23 (IBM, Inc., Armonk, NY). The study was approved by the institutional review board of Rush University Medical Center (Chicago, IL).
Results
A total of 548 subjects enrolled in the ASSUAGE (n = 248) and ASSUAGE-CKD (n = 300) trials were analyzed. The baseline characteristics of the study population were summarized in Table 1. Notably, the baseline characteristics of patients randomized to receive aminophylline (n = 274) vs placebo (n = 274) were similar, except that patients in the placebo group had significantly higher rate of prior MI (P = .03), representing a randomization failure. Therefore, to verify whether any observed differences in perfusion abnormalities are not due to disparity in MI history, we adjusted for prior MI in subsequent multivariate analyses.
As compared to patients in the placebo group, those who received aminophylline had similar SDS and SSS by quantitative and semi-quantitative analyses (Table 2). As illustrated in Figure 1, the distribution of semi-quantitative SDS values was nearly identical between the study groups (P = .87). Moreover, there were no significant differences in reversible defect size, post-stress change in LVEF, and mean TID ratio (Table 2). After adjusting for history of MI, there were no significant differences between the study groups in the semi-quantitative SDS and SSS (ANCOVA P values .66 and .41, respectively).
There was no significant difference between the study groups in the rates of myocardial ischemia (SDS ≥ 2) in univariate analysis (Table 2) and after adjusting for prior MI (P = .78) in multivariate logistic regression analysis. In this model, prior MI was associated with incidents of myocardial ischemia (odds-ratio 1.63; 95% confidence interval 1.001-2.62; P = .045). In univariate analysis, there was a trend toward higher rate of abnormal MPI (SSS ≥ 4) among patients in the placebo group (Table 2). However, after adjusting for history of MI in multivariate logistic regression analysis, there was no significant association between aminophylline use and abnormal MPI (P = .19), while history of MI was associated with incidents of abnormal MPI (odds-ratio 3.18; 95% confidence interval 1.99-5.08; P < .001).
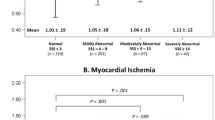
During follow-up of 29 ± 14 months, there were 81 events of the composite endpoint of cardiac death or MI and 102 events of the composite endpoint of cardiac death, MI, or coronary revascularization. There were no significant differences in the event-free survival between the study groups, after adjusting for SDS, SRS, history of MI, and LVEF (Figure 2). In the same model, there was no significant interaction between aminophylline use and semi-quantitative SDS as a determinant of study outcomes (Figure 2). Moreover, there was no significant interaction between aminophylline use and myocardial ischemia (SDS ≥ 2) as a determinant of the composite endpoint of cardiac death or MI (P = .67) or the composite endpoint of cardiac death, MI, or coronary revascularization (P = .79), adjusting for myocardial ischemia (SDS ≥ 2), SRS, history of MI, and LVEF.
Sensitivity Analyses
We sought to determine whether any differences in ischemic burden were due to blunted regadenoson effect by aminophylline versus baseline difference in the prevalence of prior MI. To that end, we repeated all study analyses after excluding patients with clinical or MPI evidence (SRS ≥ 4) of prior MI. In the subgroup of patients without prior MI (n = 309), there were no significant differences in the burden of semi-quantitative or quantitative SDS and SSS, and there were no differences in the incidence of abnormal MPI or myocardial ischemia (Table 3). Similarly, among patients without evidence of prior MI, there were no significant differences in survival free of either study outcome between aminophylline vs placebo group (P values ≥.16), adjusting for SDS, SRS, and LVEF. Furthermore, there was no significant interaction between aminophylline use and SDS as a determinant of either study outcome (P values ≥.49). Finally, among patients with normal resting perfusion (SRS ≤ 3) and no myocardial ischemia (SDS ≤ 1), there were no significant differences between aminophylline and placebo groups in the rates of cardiac death or MI [10% vs 13%, respectively, log-rank P = .32] and the rates of cardiac death, MI, or coronary revascularization [13% vs 16%, respectively, log-rank P = .32].
Discussion
Aminophylline is frequently administered to treat adverse effects of adenosine receptor agonists.12,13 Typically, aminophylline administration is delayed several minutes following the stress radioisotope injection to allow for maximal myocardial radioisotope uptake before reversing myocardial hyperemia. Premature administration of aminophylline can potentially blunt stress-induced perfusion abnormality. In a dog model, Sinusas et al demonstrated that 99mTc-tetrofosmin uptake by ischemic and non-ischemic myocardium plateaus is approximately 100 seconds following the radioisotope injection.7 On this basis, aminophylline injection in the ASSUAGE protocol was timed at 90 seconds, allowing additional 10 seconds for slow aminophylline bolus to reach coronary capillary bed. Therefore, 90 seconds after radioisotope injection was thought to be the earliest aminophylline can be administered to attenuate regadenoson adverse effects without compromising the detection of myocardial ischemia by SPECT-MPI. Indeed, aminophylline administration, according to the ASSUAGE protocol, led to reductions in the incidence of gastrointestinal symptoms, headache, and any regadenoson-related adverse effects by 50%, 70%, and 34%, respectively, and improved the overall tolerability of regadenoson stress.5 However, the effect of this aminophylline administration protocol on the burden of detectable regadenoson-induced perfusion abnormality was not properly explored. In the original reports of the ASSUAGE trials, we demonstrated that there were no significant differences in the quantitative SDS burden between subjects in the aminophylline vs placebo arms.5,6 However, the reported analyses were limited by small sample size within each trial and by the fact that myocardial perfusion was assessed quantitatively, rather than more appropriate blinded semi-quantitative analysis. Moreover, the original reports where not supported by long-term outcome data confirming a neutral effect of aminophylline use on outcome. In this report, we demonstrated, in high-quality data in randomized study groups, a “neutral effect” of aminophylline administered according to the ASSUAGE protocol on myocardial perfusion burden and patient outcome. The study cohort comprises a population with high comorbidity (49% diabetes mellitus; 68% severe chronic kidney disease; 31% known coronary artery disease) and high ischemic burden, thus providing the study added power to detect differences in SDS. Our analyses are predicated on the assumption that ischemic burden is evenly distributed between the study groups due to randomization. Indeed, the study groups were well balanced, given the randomized assignment in the original trials. However, there was a slight imbalance with excess of patients with prior history of MI (randomization failure); this manifested in a trend toward higher SRS and SSS burden in the placebo group. The slight statistically insignificant difference in SSS was entirely due to baseline difference in SRS (prior MI) but not SDS (myocardial ischemia). When we adjusted for prior MI or excluded patients with prior MI, any trends of higher SSS in the placebo group further diminished, thus indicating that slight SSS differences is due to baseline imbalance in MI burden rather than differences in regadenoson-induced ischemia. Moreover, extensive analysis of quantitative ancillary evidence of myocardial ischemia such as reversible defect size, transient ischemic dilation, and change in LVEF was not different between the study groups. These analyses showed no evidence that aminophylline administered according to the ASSUAGE protocol attenuates the burden of regadenoson-induced myocardial ischemia.
Among SPECT-MPI radiopharmaceuticals, 99mTc-tetrofosmin has most inferior myocardial uptake characteristics in terms of extraction fraction and linearity.14 Thus, imaging with this agent is most vulnerable to premature reversal of myocardial hyperemia with aminophylline. Therefore, the study findings can be extrapolated to 99mTc-sestamibi and 201Tl, since those agents have superior myocardial uptake properties.
It is important to note, however, that the ASSUAGE trials were not primarily designed or powered to assess the impact of aminophylline administration on the burden of regadenoson-induced myocardial ischemia. An optimal methodology would be a crossover design in which subjects serve as their own controls, assessing agreement in MPI findings between standard and ASSUAGE protocols.
New Knowledge Gained
Analyses of the pooled database of the ASSUAGE and ASSUAGE-CKD trials indicate that, in patients undergoing regadenoson-stress SPECT-MPI, intravenous administration of 75 mg of aminophylline, 90 seconds following radioisotope injection, does not seem to impact the detectable burden of regadenoson-induced perfusion abnormality. Aminophylline use does not seem to be associated with excess cardiac events which may occur from missed myocardial ischemia.
Conclusion
In patients undergoing regadenoson-stress SPECT-MPI, the use of intravenous aminophylline (75 mg) as early as 90 seconds following radioisotope injection to attenuate regadenoson-related adverse events does not seem to impact the diagnostic performance of regadenoson-stress SPECT-MPI. This finding need to be confirmed in a specifically designed and adequately powered study.
Abbreviations
- LVEF:
-
Left ventricular ejection fraction
- MI:
-
Myocardial infarction
- MPI:
-
Myocardial perfusion imaging
- SDS:
-
Summed difference score
- SPECT:
-
Single-photon emission computed tomography
- SRS:
-
Summed rest score
- SSS:
-
Summed stress score
References
Gao Z, Li Z, Baker SP, Lasley RD, Meyer S, Elzein E, et al. Novel short-acting A2A adenosine receptor agonists for coronary vasodilation: Inverse relationship between affinity and duration of action of A2A agonists. J Pharmacol Exp Ther 2001;298:209-18.
Lieu HD, Shryock JC, von Mering GO, Gordi T, Blackburn B, Olmsted AW, et al. Regadenoson, a selective A2A adenosine receptor agonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol 2007;14:514-20.
Shryock JC, Snowdy S, Baraldi PG, Cacciari B, Spalluto G, Monopoli A, et al. A2A-adenosine receptor reserve for coronary vasodilation. Circulation 1998;98:711-8.
Zhao G, Linke A, Xu X, Ochoa M, Belloni F, Belardinelli L, et al. Comparative profile of vasodilation by CVT-3146, a novel A2A receptor agonist, and adenosine in conscious dogs. J Pharmacol Exp Ther 2003;307:182-9.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “The ASSUAGE trial”. J Nucl Cardiol 2012;19:448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Margeta B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease—The ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29:1029-37.
Sinusas AJ, Shi Q, Saltzberg MT, Vitols P, Jain D, Wackers FJ, et al. Technetium-99 m-tetrofosmin to assess myocardial blood flow: Experimental validation in an intact canine model of ischemia. J Nucl Med 1994;35:664-71.
Rangel MO, Morales Demori R, Voll ST, Wassouf M, Dick R, Doukky R. Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE and ASSUAGE-CKD trials. J Nucl Cardiol 2015;22:1008-18.
AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0234-0.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0303-4.
Ballany W, Mansour K, Morales Demori R, Al-Amoodi M, Doukky R. The impact of regimented aminophylline use on extracardiac radioisotope activity in patients undergoing regadenoson stress SPECT myocardial perfusion imaging: A substudy of the ASSUAGE trial. J Nucl Cardiol 2014;21:496-502.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: The first prospective evaluation. J Nucl Cardiol 2013;20:205-13.
Lin LF, Cheng CY, Hou CH, Ku CH, Tseng NC, Shen DH. Experience of low-dose aminophylline use to relieve minor adverse effects of dipyridamole in patients undergoing stress myocardial perfusion imaging. J Nucl Cardiol 2014;21:563-9.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016. doi:10.1007/s12350-015-0387-x.
Disclosure
Rami Doukky received research support from Astellas Pharma US (none of which was used to fund this investigation) and serves on the Advisory Board of Astellas Pharma US. No conflict of interests to be reported by other authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Rights and permissions
About this article
Cite this article
Fughhi, I., Campagnoli, T., Ali, A. et al. Impact of a regimented aminophylline administration protocol on the burden of regadenoson-induced ischemia detected by SPECT myocardial perfusion imaging. J. Nucl. Cardiol. 24, 1571–1578 (2017). https://doi.org/10.1007/s12350-016-0506-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0506-3