Abstract
Background
To compare the accuracy of end-diastolic and end-systolic volumes (EDV, ESV) and LV ejection fraction (LVEF) measured by both GSPECT and GPET, using cardiac magnetic resonance imaging (CMR) as a reference. Furthermore, the impacts of severe perfusion defects, akinetic/dyskinetic segments, and residual viable myocardium on the accuracy of LV functional parameters were investigated.
Methods
Ninety-six consecutive patients with LV aneurysm and LV dysfunction (LVEF 32 ± 9%) diagnosed by CMR were studied with GSPECT and GPET. EDV, ESV, and LVEF were calculated using QGS software.
Results
Correlations of volumes were excellent (r 0.81-0.86) and correlation of LVEF was moderate (r 0.65-0.76) between GSPECT vs CMR and between GPET vs CMR. Compared with CMR, ESV was overestimated by GSPECT (P < .01) and underestimated by GPET (P < .0001); EDV was underestimated by GPET (P < .001); LVEF was underestimated by GSPECT but overestimated by GPET (both P < .001). Multivariate regression analysis revealed that the number of segments with severe perfusion defects (P < .001) was the only independent factor which was correlated to the EDV difference between GSPECT and CMR, the number of akinetic/dyskinetic segments with absent wall thickening (WT) was the only independent factor which was significantly correlated to the differences of ESV and LVEF measurements between GSPECT vs CMR and between GPET vs CMR (P < .0001), respectively. Neither the mismatch score nor the segments with viable myocardium were correlated to the differences of LV volumes and LVEF measurements between different imaging modalities.
Conclusions
In LV aneurysm patients, LV volumes and LVEF measured by both GSPECT and GPET imaging correlated well with those determined by CMR, but should not be interchangeable in individual patients. The accuracy of LVEF measured by GSPECT and GPET was affected by the akinetic/dyskinetic segments with absent WT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with left ventricular (LV) aneurysm usually have severe LV remodeling and LV dysfunction, which may result in a poor prognosis if treated medically only.1-4 An accurate assessment of global LV function, myocardial perfusion and viability in patients with LV aneurysm (LVA) is crucial for management and cardiac risk stratification. The clinical value of 99mTc-sestamibi (MIBI) SPECT and 18F-fluorodeoxyglucose (18F-FDG) PET for assessing myocardial viability in LVA patients has been demonstrated previously.4,5 However, at that time, gated acquisition was not routinely performed in both SPECT and PET studies, while LV function was analyzed by echocardiography.
Nowadays, electrocardiography gated myocardial perfusion SPECT (GSPECT) combined with automated quantitative algorithms enables the simultaneous assessment of myocardial perfusion and LV function, and its value has been extensively validated in patients with coronary artery disease (CAD)6-8 and further investigated in patients with myocardial infarction (MI).9-14 Although severe perfusion defects (SPD) and akinetic/dyskinetic segments were assumed to affect the accuracy of LV volumes and LV ejection fraction (LVEF) measured by GSPECT, there is no previous investigation systematically demonstrated that these two factors were correlated to the differences of LV volumes and LVEF measurements by GSPECT and the other imaging mordalites.9-14 Therefore, the value of GSPECT in LVA patients remains to be established.15 In addition, compared with SPECT imaging modality, PET imaging system has a higher temporal and spatial resolution, and gated acquisition is routinely performed for viability assessment and thus can simultaneously assess LV function. Several earlier studies have demonstrated that the value of gated PET (GPET) analyzing LV function compared with different imaging modalities in patients with CAD.16-21 Yet, the value of GPET for assessing LV function in LVA patients compared with cardiac magnetic resonance imaging (CMR) as gold standard remains to be defined. Finally, it was well known that dysfunctional but viable myocardium often shows preserved uptake of 18F-FDG in perfusion defects, GPET may provide more accurate LV functional parameters compared with that assessed by GSPECT. However, no previous study thoroughly compared the accuracy of LV volumes and LVEF measured by GSPECT and GPET, and little information has become available whether GSPECT and GPET-derived functional parameters are interchangeable.22,23
Therefore, we aimed to compare the accuracy of LV end-diastolic and end-systolic volumes (EDV, ESV) and LVEF from 99mTc-MIBI GSPECT and 18F-FDG GPET in LVA patients, using CMR as a gold standard. Additionally, we analyzed the impacts of SPD, the residual viable myocardium, and the number of akinetic/dyskinetic segments on the accuracy of LV volumes and LVEF measured by both GSPECT and GPET.
Methods
Patient Population
Patients with LVA documented by MRI were recruited retrospectively from a study population referred to the Fu Wai Hospital between September 2009 and February 2012 for routinely scheduled myocardial viability assessment with 99mTc-sestamibi GSPECT rest perfusion imaging and 18F-FDG GPET/CT metabolic imaging, using a 2-day protocol. All patients were examined with CMR within a 2-week period (median 4 days) and they were in a stable state and none of them had any cardiac events or additional therapeutic intervention between PET, SPECT, and CMR examinations. Patients with severe arrhythmia, rheumatic valvular disease, dilated cardiomyopathy, previous LVA resection surgery, metal fragments, and implanted ferromagnetic devices were excluded. Further, patients with impaired SPECT or PET imaging quality (very low activity) were also excluded (n = 6). Accordingly, the finally study population consisted of 96 patients (88 males and 8 females; mean age 57 ± 10 years, mean LVEF 32 ± 9% by CMR). All patients had a history of at least one previous MI. The clinical characteristics are summarized in Table 1. The study protocol was approved by the ethics committee of the Cardiovascular Institute and Fu Wai Hospital.
Gated 99mTc-Sestamibi SPECT at Rest
Gated SPECT perfusion images were acquired over a 180° arc with a dual-head SPECT system (e.cam, Siemens Medical Systems) equipped with a low-energy, high-resolution, parallel-hole collimator 90-120 minutes after injection of 99mTc-sestamibi (925 MBq) at rest. GSPECT imaging was performed for 15 minutes with 32 views, at 25 seconds per view, using 64 × 64 matrix size with a zoom factor of 1.45. The cardiac cycle was divided into eight equal intervals with a 20% window centered over the 140 keV photo peak. Gated transaxial images were reconstructed using the Butterworth-filtered back-projection method (order 5; cutoff frequency 0.40) and displayed as short-axis and horizontal and vertical long-axis slices.
Gated 18F-FDG PET
Myocardial 18F-FDG images were obtained with a high-spatial-resolution full-ring PET scanner (Truepoint Biography 64, Siemens Healthcare, Knoxville, TN). Patients were studied with the glucose-loading method (25-50 g glucose) or a regular short-acting insulin intravenous injection according to the serum glucose level after an overnight fast.4,5 18F-FDG 185 MBq (Chinese Atomic Energy Institute, Beijing, China) was administered intravenously; gated images were acquired after 1 hour for 10 minutes (3D mode), dividing the cardiac cycle into eight equal intervals and formatted into a 128 × 128 image matrix and a zoom factor of 2.0 was applied.
Analysis of SPECT and PET Images
Both non-gated and gated, SPECT and PET data sets were transferred to a Siemens e.soft workstation, transaxial SPECT and PET images were reconstructed using the ordered-subsets expectation maximization (OSEM, 4 iterations, 8 subsets) and displayed as short-axis and horizontal and vertical long-axis slices. Both GSPECT and GPET were reprocessed by one trained observer (Tian CN), unaware of the clinical and CMR data. LV functional parameters, including EDV, ESV, and LVEF, were automatically calculated by using QGS software (version 3.1, Cedars-Sinai Medical Center, Los Angeles, CA, USA), with manual correction in case of inadequate endocardium and epicardium delineation, especially in patients with large severe perfusion defects (20% of the total study population). Regional functional parameters, which including wall motion (WM) and wall thickening (WT), were assessed automatically with the American Heart Association 17-segment model, 6-point scoring system with WM (0 = normokinesis, 1 = mild hypokinesis, 2 = moderate hypokinesis, 3 = severe hypokinesis, 4 = akinesis, and 5 = dyskinesis) and a 4-point scoring system with WT (0-3: from normal to absent WT).24 An akinetic/dyskinetic segment was defined as WM score ≥ 4, or WT score = 3.
Two experienced observers (ZXL, TYQ), unaware of the clinical data and LV functional parameters, visually graded both MIBI and FDG myocardial activity with 5-point score and 17-segment model.24 The segment with the highest perfusion activity was defined as normal, and the relative perfusion and metabolic activity in the residual segments were graded where 0 is normal radiotracer activity, 1 is mildly reduced activity, 2 is moderately reduced activity, 3 is severely reduced activity, and 4 is absence of activity. Severe perfusion defect (SPD) was defined as segments with absence of activity (MIBI score = 4). The mismatch score of the LV was calculated as the summed rest perfusion score minus the summed FDG score, and viability in perfusion defect was defined as a mismatch score of 1.0 or greater.
Cardiac MRI (CMR)
All patients underwent CMR on a 1.5-T system (Magnetom Avanto®, Siemens Medical Systems, Erlangen, Germany), equipped with gradient magnets with a maximum strength of 50 mT·m−1, a maximum slew rate of 200 mT·m−1 ms−1, using an eight-element cardiac phased-array coil. An ECG-triggered, breath-hold steady-state free precession pulse cine sequence was used, with flip angle of 80°, matrix of 256 × 256 (field of view: 350-400 mm) and slice thickness of 8 mm. Each slice was acquired in a separate breath-hold cycle at the end expiration inspiration and 25 frames were acquired per cardiac cycle. All data were transferred to a separate workstation and analyzed by one physician using the commercially available MASS software (version 5.0, Medis Medical Imaging Systems, Leiden, The Netherlands). Endocardial and epicardial borders were outlined automatically with manual correction in case of inadequate anatomic delineation on both the ED and ES frames. The trabeculation and papillary muscles were included as part of LV volumes. LVEF was expressed as a percentage, which was calculated as the stroke volume divided by the EDV.
Statistical Analysis
Data were analyzed using SPSS software (version 17.0, Chicago, IL). Continuous data were expressed as mean value ± SD. Mean values of continuous variables were compared by paired Student’s t test or by one-way ANOVA analysis. Categorical data were expressed as a percentage and the Chi square test was used. The degree of agreement was tested using the method of Bland-Altman analysis and the Bland-Altman limits were calculated using the mean of the differences ±1.96 SDs of the differences. Intraclass correlation was calculated to assess the strength of agreement between two measurements from different imaging mortalities (GSPECT vs CMR, GPET vs CMR, and GSPECT vs GPET). To test the processing variability in GSPECT, GPET, and CMR, all imaging datasets were processed again by the same observer and another experienced observer for evaluation of the intra- and inter-observer reproducibility.
Factors which may correlate to the discrepancies of LV functional parameters between different imaging modalities were analyzed by the linear regression analysis. Only variables with a statistically significant association with the correlation by univariate analysis were included in the multivariate analysis, which was created by a stepwise method. Statistical significance was defined as two-sided if a P value <.05.
Results
Mean EDV, ESV, and LVEF
Mean values of EDV, ESV, and LVEF from GSPECT, GPET, and CMR are presented in Table 2. Compared with CMR, ESV was overestimated (P < .01) by GSPECT, EDV and ESV were underestimated by GPET (P < .001), while LVEF was underestimated by GSPECT (P < .001) and overestimated by GPET (P < .001).
Correlation and Regression Analysis of GSPECT Vs CMR, GPET Vs CMR, and GSPECT Vs GPET
Table 3 listed the correlation and regression analysis results. Between GSPECT and CMR, correlations of EDV (P < .001) and ESV (P < .0001) were excellent, and correlation of LVEF (P < .001) was good. Compared with CMR, EDV (r = 0.28, P < .01) and ESV (r = 0.34, P = 0.001) assessed by GSPECT showed a higher trend with increasing magnitude of LV volumes. The bias in EF measurement was independent of EF magnitude (P > 0.05) (Figure 3 in Appendix).
Correlations of EDV (P < .001) and ESV (P < .001) were excellent and correlation of LVEF (P < .001) was good between GPET and CMR. Compared with CMR, no significant trend was found for estimation of EDV and ESV by GPET with increasing magnitude of LV volumes (P > 0.05). The Bland-Altman plot displayed a trend to overestimation of LVEF by GPET increasingly with higher LVEF (r = 0.26, P = 0.01) (Figure 4 in Appendix).
Correlations of EDV (P < .001) and ESV (P < .001) between GSPECT and GPET were excellent. Compared with GSPECT, with increasing of LV volumes, GPET showed a trend toward lower EDV (r = −0.36, P < .001) and lower ESV (r = −0.29, P < .01), respectively. Correlation of LVEF between GPET and GSPECT was good (P < .001). The overestimated measurement of LVEF by GPET was dependent on EF magnitude (r = 0.40, P < .001) (Figure 5 in Appendix).
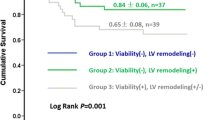
Influence of SPD on the Discrepancies Between GSPECT and GPET
Patients were divided intro three subgroups according to the number of segments with SPD. Group 1 (n = 18, 19%): ≤2 segments; Group 2 (n = 30, 31%): 3-4 segments (Figure 1); Group 3 (n = 48, 50%): ≥5 segments (Figure 2). Mean values of LV volumes and LVEF are presented in Table 4. The correlation of LVEF between GSPECT and GPET was fair in Groups 2 and 3 (P < .0001). In comparison with those values measured by CMR: (1) In Group 1, both EDV (P < .005) and ESV (P < .05) were mildly underestimated by GSPECT, and LVEF was overestimated by GPET (P < .05); (2) in Group 2, LV volumes were underestimated by GPET (P < .05). LVEF was slightly underestimated by GSPECT (P < .05) and overestimated by GPET (P < .05); (3) In Group 3, LV volumes were severely overestimated by GSPECT (P < .0001) and underestimated by GPET (P < .0001). LVEF was severely underestimated by GSPECT (P < .0001). The difference of EDV between GSPECT and GPET in Group 3 was greater than that in Groups 2 (P < .001) and 1 (P < .0001). And the difference of ESV between GSPECT and GPET in Group 3 was greater than that in Groups 2 (P < .01) and 1 (P < .0001). However, no such difference was observed for LVEF measurement (P > 0.05).
Influence of Residual Myocardial Viability on the Discrepancies Between GSPECT and GPET
Patients were grouped into three subgroups according to the number of segments with viable myocardium. Group A (n = 22): ≤1 viable segment; Group B (n = 27): 2-3 viable segments; and Group C (n = 47): ≥4 viable segments. Mean values of LV volumes and LVEF are presented in Table 5. The correlations of LV volumes measurement between GSPECT and GPET were good in all the subgroups while the correlation of LVEF measurement was fair (P < .0001). In Group A, LVEF from GSPECT had no significant difference with that from CMR, but it was overestimated by GPET (P < .05). In Group B, mean LVEF measured by GPET was similar with that by CMR, whereas LVEF assessed by GSPECT was lower than that by CMR (P < .001). Further, in Group C, compared with CMR, LVEF was underestimated by GSPECT (P < .001) while overestimated by GPET (P < .01). In subgroups with different extent of residual viable myocardium, no significant difference was found for the biases of EDV, ESV, and LVEF measurements between GSPECT and GPET (P > 0.05).
Univariate and Multivariate Regression Analysis
Variables correlated with the differences of LV volumes and EF measurements are illustrated in Table 6. Univaritate regression analysis showed that many factors were correlated to the differences of LV volumes and LVEF measurements between GSPECT and CMR, and few were correlated to the differences of LV functional parameters between GPET and CMR. Moreover, multivariate regression analysis identified (1) SPD (P < .001) was the only independent factor which was correlated to the differences of EDV measurement between GSPECT and CMR, and absent MIBI WT (P < .001) was the only independent factor which was correlated to the differences of ESV and LVEF measurements between GSPECT and CMR; (2) absent FDG WT was the only independent factor which was correlated to the differences of ESV and LVEF measurements between GPET and CMR (P < .001). In surprise, neither the mismatch score nor the number of segments with myocardial viability was proved to be statistically significant correlated to differences of LV volumes and LVEF measurements between different imaging modalities (GSPECT vs CMR, GPET vs CMR, and GSPECT vs GPET) (P > 0.05).
Reproducibility
As shown in Table 7, both intra- and inter-observer comparisons of repeated measurements of EDV, ESV, and LVEF revealed significant correlations in GSPECT, GPET, and CMR (all P < 0.001), indicating excellent reproducibility.
Discussion
The main findings were as follows: (1) In LVA patients, LV volumes and LVEF measured by both GSPECT and GPET correlated well with those determined by CMR over a wide range, while GSPECT and GPET-derived functional parameters do not appear to be interchangeable in individual patients; (2) the number of segments with SPD was the only independent factor which was correlated to the EDV difference between GSPECT and CMR. The number of akinetic/dyskinetic segments with absent wall thickening (WT) was the only independent factor which was significantly correlated to the differences of ESV and LVEF measurements between GSPECT vs CMR, and between GPET vs CMR, respectively. (3) In patients with small extent of SPD or without viable myocardium, LVEF by GSPECT was more accurate. In patients with large extent of SPD or moderate extent of viable myocardium, LVEF by GPET was more reliable. In patients with moderate extent of SPD or with large extent of viable myocardium, LVEF was underestimated by GSPECT and overestimated by GPET.
LV Volumes and LVEF by GSPECT, Compared with CMR
The value of GSPECT in LVA patients remains to be established.15 In addition, both SPD and akinetic/dyskinetic segments were assumed to affect the accuracy of LV volumes and LVEF measured by GSPECT. However, it has not been systematically proved, as the populations studied were not homogeneous.9-15,25 Chua et al10 found that LVEF did not differ between GSPECT and radionuclide ventriculography in patients with larger MI. Manrique et al9 reported that underestimation of LVEF by GSPECT was not correlated to the size and severity of perfusion defects, and dyskinesia segments. Similarly, Bax et al11 revealed that in patients with ischemic cardiomyopathy, the underestimation of LV volumes by GSPECT was not correlated to the number of akinetic/dyskinetic segments, nor to the number of segments with SPD.
To our best knowledge, in current study, we recruited a largest group of LVA patients with LV dysfunction, who had SPD and akinetic/dyskinetic segments. We found that measurements of LV volumes and LVEF were correlated well between GSPECT and CMR over a wide range. Further, LVEF was underestimated by GSPECT, which was consistent with earlier studies in CAD patients.10-15,26 The 95% of agreement limits were wide, but it was similar with a meta-analysis in CAD patients.27,28 In contrast to prior investigations,9-11 we found that the number of segments with SPD was positively correlated to the overestimation of EDV by GSPECT, and the number of akinetic/dyskinetic segments was the only independent factor which was positively correlated to the overestimation of ESV and negatively correlated to underestimation of LVEF measurement by GSPECT. This denoted that the larger extent of SPD, the less reliable was the endocardial surface detection and EDV measurement by GSPECT, and more partial volume effects on the overestimation of ESV than EDV, and finally induced underestimation of LVEF. Further, in patients with small extent of SPD, LVEF did not differ between GSPECT and CMR, which was consistent with an earlier study.10 In patients with large extent of SPD, LV volumes were overestimated and LVEF was underestimated, which was in agreement with the study reported by Manrique et al.9
There are other factors which may influence LV function assessment by GSPECT, such as (1) outflow tract tissue, papillary, and trabecular muscle were included as LV volumes by CMR algorithm, and the border tracing by CMR encompasses the membraneous part of the septum, while not in GSPECT. CMR should therefore indicate larger volumes; (2) the lower temporal resolution of GSPECT compared with CMR may induce the lower LVEF.6 However, the differences in temporal resolution are more relevant in ventricles with good LV function than in dysfunctional enlarged ventricles. Our study with LVA patients in a small group (n = 16) revealed that mean values of EDV (186 ± 79 vs 188 ± 82 mL), ESV (136 ± 71 vs 135 ± 71 mL), and LVEF (29 ± 8% vs 31 ± 8%) did not differ (P > 0.05) between 8 vs 16 frames/cycle. It implied that the lower termporal resolution did not have much influence on the LV volumes and LVEF measurements by GSPECT in LVA patients with severe LV dysfunction; (3) LV volume measurements were affected by the reconstruction parameters, the higher cutoff value, LV volumes were more overestimated by GSPECT, but not much influence on LVEF.
LV Volumes and LVEF by GPET, Compared with CMR
Previous studies have demonstrated 18F-FDG GPET could accurately determine LV volumes and LVEF in CAD patients.16-21 But it is not well established its value of assessing LV function in patients with severe FDG defects.20 Our current study with LVA patients showed that correlations of LV volumes calculated by GPET and CMR were excellent, and the correlation of LVEF was good, but LV volumes were underestimated and LVEF was overestimated by GPET. These results were in line with earlier studies in CAD patients,16-21 which did not find any correlation between underestimation of volumes by GPET with FDG defects and akinetic/dyskinetic segments. Yet, our results revealed that the number of akinetic/dyskinetic segments analyzed by absent FDG WT was the only independent predictor which was positively correlated with the underestimation of ESV and negatively correlated with the overestimation of LVEF by GPET. In other words, the larger extent of myocardium with absent WT, the less underestimation of ESV and thus, the less overestimation of LVEF was measured by GPET. Some other factors which may affect LV function assessment by GPET were similar as described in GSPECT perfusion imaging.
Effects of Residual Viable Myocardium on the Accuracy of LV Volumes and EF Measured by GSPECT and GPET
It was well known that dysfunctional but viable myocardium often shows preserved uptake of 18F-FDG in perfusion defects,4,5 in this kind of cases, it was assumed that exact delineation of endo- and epicardial contours by GPET may provide more accurate LV functional parameters compared with that assessed by GSPECT. However, no previous study systemically compared the accuracy of LV volumes and LVEF measured by GSPECT and GPET, and little information has become available on the differences of LV volumes and LVEF between GSPECT and GPET.22,23 In our current study, we found that the correlations of LV volumes measurements between GSPECT and GPET were excellent and correlation of LVEF was fair, but the Bland-Altman limits were wider. Therefore, on individual patient’s level, GSPECT and GPET-derived functional parameters (especially LV volumes) should not be interchangeable. Further, it was appreciated that the number of segments with SPD was correlated to overestimation of volumes by GSPECT, compared with that by GPET (Table 8 in Appendix). Notably, we found that the number of segments with absent FDG WT was the only independent factor, which was positively correlated to the LVEF differences between GSPECT and GPET (Table 8 in Appendix). It indicated that the more extent of akinetic/dyskinetic segments revealed by absent FDG WT, the more consistent of LVEF value measured by GSPECT and GPET. These findings were different from that in previous studies.22,23 Kanayama et al23 found that LVEF did not differ between gated 13N-NH3 PET and 99mTc-MIBI SPECT in CAD patients, and the extent of perfusion defects had no influence on the underestimation of LV volumes determined by GPET, compared with that measured by GSPECT.
Conversely, it was somehow surprising to observe that the extent and severity of hibernation myocardium was not correlated to the differences of LV functional parameters between GSPECT and GPET. Further subgroup analysis showed that in patients without or with a small extent of viable myocardium, LVEF measured by GSPECT was more reliable while overestimated by GPET, and in patients with moderate extent of viable myocardium, LVEF measured by GPET was more accurate while underestimated by GSPECT. Finally, in patients with large amount of viable myocardium, LVEF was underestimated by GSPECT and overestimated by GPET. The exact reason is not very clear. In current study, myocardial perfusion was performed by 99mTc-MIBI SPECT without attenuation correction rather by PET perfusion with N-13 ammonia or Rb-82, thus the extent and severity of hibernation myocardium could be overestimated, especially in inferior and posterior wall with mild reduced perfusion activity. But if these segments with normal regional function, they were regarded as normal myocardium. Further, it would be possible, only in patients with large extent of SPD, the differences of LV volumes measured by GSPECT and GPET were correlated to the extent of viable myocardium. However, no any trend was found even if we clarified patients into four subgroups according to the extent of SPD and extent of viable myocardium together.
Study Limitations
Our study had some limitations. Drug treatment and patient’s pathophysiological changes may have affected current observations, due to the time interval between radionuclide imaging and CMR examinations. Yet, 85% of patients were performed within 7 days, which should have widely excluded effects of confounding factors on measurements of LV function with different imaging modalities.
In conclusions, in LVA patients, LV volumes and LVEF measured by both GSPECT and GPET imaging correlated well with those determined by CMR, while the accuracy of EDV measurement by GSPECT was affected by SPD, and the accuracy of ESV and LVEF measurements by both GSPECT and GPET was affected by the extent of akinetic/dyskinetic segments with absent WT.
New Knowledge Gained
This study revealed that in routine clinical practice for viability assessment, GSPECT and GPET-derived functional parameters could not be used interchangeably on individual’s patient level, even though each has its own advantages. In patients with small extent of SPD or without viable myocardium, LVEF by GSPECT was more reliable. In patients with large extent of SPD or moderate extent of viable myocardium, LVEF by GPET was more accurate. In patients with moderate extent of SPD or with large extent of viable myocardium, LVEF was underestimated by GSPECT and overestimated by GPET.
References
Meizlish JL, Berger HJ, Plankey M, Errico D, Levy W, Zaret BL. Functional left ventricular aneurysm formation after acute anterior transmural myocardial infarction. Incidence, natural history, and prognostic implications. N Engl J Med 1984;311:1001-6.
Faxon D, Myers W, McCabe C, Davis KB, Schaff HV, Wilson JW, et al. The influence of surgery on the natural history of angiographically documented left ventricular aneurysm: The Coronary Artery Surgery Study. Circulation 1986;74:110-8.
Louagie Y, Alouini T, Lesperance J, Pelletier LC. Left ventricular aneurysm with predominating congestive heart failure. A comparative study of medical and surgical treatment. J Thorac Cardiovasc Surg 1987;94:571-81.
Zhang XL, Liu XJ, Wu QY, Shi R, Gao R, Liu Y, et al. Clinical outcome of patients with previous myocardial infarction and left ventricular dysfunction assessed with 99mTc-MIBI myocardial SPECT and 18F-FDG myocardial PET. J Nucl Med 2001;42:1166-73.
Zhang XL, Liu XJ, Hu SS, Thomas S, Tian YQ, Gao RL, et al. Long-term survival of patients with viable and nonviable aneurysms assessed by 99mTc-MIBI SPECT and 18F-FDG PET: A comparative study of medical and surgical treatment. J Nucl Med 2008;49:1288-98.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138-47.
Lipke CS, Kuhl HP, Nowak B, Kaiser HJ, Koch KC, Buell U. Validation of 4D-MSPECT and QGS for quantification of left ventricular volumes and ejection fraction from gated 99mTc-MIBI SPET: Comparison with cardiac magnetic resonance imaging. Eur J Nucl Med Mol Imaging 2004;31:482-90.
Schaefer WM, Lipke CS, Standke D, Kühl HP, Nowak B, Kaiser HJ, et al. Quantification of left ventricular volumes and ejection fraction from gated 99mTc-MIBI SPECT: MRI validation and comparison of the Emory Cardiac Tool Box with QGS and 4D-MSPECT. J Nucl Med 2005;46:1256-63.
Manrique A, Faraggi M, Vera P, Vilain D, Lebtahi R, Cribier A, et al. 201Tl and 99mTc-MIBI gated SPECT in patients with large perfusion defects and left ventricular dysfunction: Comparison with equilibrium radionuclide angiography. J Nucl Med 1999;40:805-9.
Chua T, Yin LC, Thiang HT, Choo TB, Ping DZ, Leng LY. Accuracy of the automated assessment of left ventricular function with gated perfusion SPECT in the presence of perfusion defects and left ventricular dysfunction: Correlation with equilibrium radionuclide ventriculography and echocardiography. J Nucl Cardiol 2000;7:301-11.
Bax JJ, Lamb H, Dibbets P, Pelikan H, Boersma E, Viergever EP, et al. Comparison of gated single-photon emission computed tomography with magnetic resonance imaging for evaluation of left ventricular function in ischemic cardiomyopathy. Am J Cardiol 2000;86:1299-305.
Canbaz F, Basoglu T, Yapici O, Aygul S, Yazici M. Myocardial perfusion defects with near-to-absent count reduction: A comparison of gated SPECT to radionuclide ventriculography in the determination of left ventricular function. Int J Cardiovasc Imaging 2006;22:231-41.
Kakhki VR, Zakavi SR, Sadeghi R. Comparison of two software in gated myocardial perfusion single photon emission tomography, for the measurement of left ventricular volumes and ejection fraction, in patients with and without perfusion defects. Hell J Nucl Med 2007;10:19-23.
Harisankar CN, Mittal BR, Kamaleshwaran KK, Parmar M, Bhattacharya A, Singh B, et al. Reliability of left ventricular ejection fraction calculated with gated myocardial perfusion single photon emission computed tomography in patients with extensive perfusion defect. Nucl Med Commun 2011;32:503-7.
Canbaz F, Basoglu T, Durna K, Semirgin SU, Canbaz S. Left ventricular aneurysm in the scope of gated perfusion SPECT: Accuracy of detection and ejection fraction calculation. Int J Cardiovasc Imaging 2008;24:585-96.
Willemsen AT, Siebelink HJ, Blanksma PK, Paans AM. Automated ejection fraction determination from gated myocardial FDG-PET data. J Nucl Cardiol 1999;6:577-82.
Hattori N, Bengel FM, Mehilli J, Odaka K, Ishii K, Schwaiger M, et al. Global and regional functional measurements with gated FDG PET in comparison with left ventriculography. Eur J Nucl Med 2001;28:221-9.
Saab G, Dekemp RA, Ukkonen H, Ruddy TD, Germano G, Beanlands RS. Gated fluorine 18 fluorodeoxyglucose positron emission tomography: Determination of global and regional left ventricular function and myocardial tissue characterization. J Nucl Cardiol 2003;10:297-303.
Schaefer WM, Lipke CS, Nowak B, Kaiser HJ, Buecker A, Krombach GA, et al. Validation of an evaluation routine for left ventricular volumes, ejection fraction and wall motion from gated cardiac FDG PET: A comparison with cardiac magnetic resonance imaging. Eur J Nucl Med Mol Imaging 2003;30:545-53.
Schaefer WM, Lipke CS, Nowak B, Kaiser HJ, Reinartz P, Buecker A, et al. Validation of QGS and 4D-MSPECT for quantification of left ventricular volumes and ejection fraction from gated 18F-FDG PET: Comparison with cardiac MRI. J Nucl Med 2004;45:74-9.
Slart RH, Bax JJ, de Jong RM, de Boer J, Lamb HJ, Mook PH, et al. Comparison of gated PET with MRI for evaluation of left ventricular function in patients with coronary artery disease. J Nucl Med 2004;45:176-82.
Yamakawa Y, Takahashi N, Ishikawa T, Uchino K, Mochida Y, Ebina T, et al. Clinical usefulness of ECG-gated 18F-FDG PET combined with 99mTc-MIBI gated SPECT for evaluating myocardial viability and function. Ann Nucl Med 2004;18:375-83.
Kanayama S, Matsunari I, Kajinami K. Comparison of gated N-13 ammonia PET and gated Tc-99m sestamibi SPECT for quantitative analysis of global and regional left ventricular function. J Nucl Cardiol 2007;14:680-7.
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol 2010;17:941-73.
Stegger L, Lipke CS, Kies P, Nowak B, Schober O, Buell U, et al. Quantification of left ventricular volumes and ejection fraction from gated 99mTc-MIBI SPECT: Validation of an elastic surface model approach in comparison to cardiac magnetic resonance imaging, 4D-MSPECT and QGS. Eur J Nucl Med Mol Imaging 2007;34:900-9.
Hedeer F, Palmer J, Arheden H, Ugander M. Gated myocardial perfusion SPECT underestimates left ventricular volumes and shows high variability compared to cardiac magnetic resonance imaging—A comparison of four different commercial automated software packages. BMC Med Imaging 2010;10:10-21.
Ioannidis J, Trikalinos T, Danias P. Electrocardiogram gated single-photon emission computed tomography versus cardiac magnetic resonance imaging for the assessment of left ventricular volumes and ejection fraction: A meta-analysis. J Am Coll Cardiol 2002;39:2059-68.
Kondo C, Fukushima K, Kusakabe K. Measurement of left ventricular volumes and ejection fraction by quantitative gated SPET, contrast ventriculography and magnetic resonance imaging: A meta-analysis. Eur J Nucl Med Mol Imaging 2003;30:851-8.
Acknowledgments
This work was supported by the Natural Science Foundation of China (8107177 and 81130029), PUMC Youth Fund and the Fundamental Research Funds for the Central Universities (3332013105) and by a Research Grant, from Ministry of Education of the People’s Republic of China.
Disclosure
We do not have any relationship with industry and financial associations from within the past 2 years that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Hongxing Wei and Xiaoli Zhang contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Wei, H., Tian, C., Schindler, T.H. et al. The impacts of severe perfusion defects, akinetic/dyskinetic segments, and viable myocardium on the accuracy of volumes and LVEF measured by gated 99mTc-MIBI SPECT and gated 18F-FDG PET in patients with left ventricular aneurysm: cardiac magnetic resonance imaging as the reference. J. Nucl. Cardiol. 21, 1230–1244 (2014). https://doi.org/10.1007/s12350-014-9978-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-9978-1