Abstract
Background
An impaired chronotropic response to exercise is an accepted risk marker but the relationship between heart rate reserve (HRR) with pharmacologic stress is less well-established. The primary aim of this analysis was to evaluate the prognostic significance of HRR in patients undergoing rest/stress myocardial perfusion positron emission tomography (PET) in estimating coronary artery disease (CAD) mortality.
Methods
This subset analysis from the PET Prognosis Multicenter Registry includes a total of 2,398 patients undergoing rest/stress Rb-PET from three participating sites. The HRR from rest to peak stress was categorized into tertiles of ≤4, 5-14, and ≥15 beats per minute (bpm). At stress, the % abnormal myocardium was categorized as <5 %, 5-9.9 %, and ≥10 %. We estimated CAD mortality using univariable and multivariable Cox proportional hazard models.
Results
CAD mortality was 12.8 %, 3.4 %, and 0.8 %, respectively, for HRR measurements of ≤4, 5-14, and ≥15 bpm (P < 0.0001). In a multivariable model, the HRR was independently predictive of CAD mortality (P < 0.0001) with adjusted hazard ratios elevated 3.5- and 8.4-fold for HRR of 5-14 and ≤4 versus ≥15 bpm. In a multivariable model, both the HRR and stress MPI % abnormal myocardium were independently and highly predictive of CAD mortality. Moreover, the net reclassification improvement was 0.18 for the HRR when compared to a model including risk factors, symptoms, rest HR, and PET variables (P = 0.0008). For those with ≥10 % abnormal myocardium on stress PET, there was a graded relationship between HRR and CAD mortality with adjusted hazards exceeding 50-fold for measurements of 5-14 and ≤4 bpm (P < 0.0001) compared to stress MPI with <5 % abnormal myocardium and a HRR ≥15 bpm.
Conclusion
A diminished HRR to vasodilator stress is a novel but increasingly important predictor of CAD mortality. HRR measurements of ≤4, 5-14, and ≥15 bpm were independently predictive of CAD mortality and underscore the importance of optimizing readily available novel markers of risk as highly relevant to identifying high and low risk patient subsets.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
For over two decades, pharmacologic stress is a well-established technique for elucidating the extent and severity of myocardial perfusion imaging (MPI) abnormalities. An abundance of evidence reports that pharmacologic stress MPI effectively and independently risk stratifies patients with suspected myocardial ischemia.1 Populations referred for pharmacologic stress are higher risk as a result of functional disability and a greater degree of comorbidity when compared to the physically capable patients able to undergo exercise testing. An impaired chronotropic response with graded exercise testing2,3 is an established risk marker and only recently has the evidence of easily identified heart rate responses (HRR) following vasodilator stress been reported to risk stratify patients with functional limitations.4-8 Recently, novel predictors have been added to the list of prognostically important variables derived during pharmacologic stress by including ancillary markers such as the changes in heart rate following intravenous administration of vasodilator agents.4,7 A blunted HRR to vasodilator stress has been associated with cardiac autonomic dysfunction.4,5,7
Despite the intriguing early reports,4,6-8 there has been a limited expansion of these findings to a diverse population of patients undergoing pharmacologic stress. The Positron Emission Tomography (PET) Prognosis Registry is a prospective, multicenter registry that has reported risk stratification evidence in a large series of patients presented for evaluation of suspected myocardial ischemia.9,10 The aim of the current report was to explore the prognostic utility of HRR in this contemporary PET registry; with the aim to define the independent and additive value of HRR following vasodilator stress in conjunction with the extent and severity of stress myocardial perfusion imaging (MPI) findings. We propose that the current analysis with the focus on the prognostic significance of HRR in patients undergoing rest/stress Rb-82 PET is important due to the current inability to perform graded exercise testing in this setting.
Methods
Registry
The findings from the PET Prognosis Registry have been previously reported9,10 and subsets of this cohort have been previously published.10-12 In brief, the PET Prognosis Registry consists of a total enrollment of 7,061 consecutively tested patients undergoing rubidium-82 (Rb-82) stress myocardial perfusion PET. From one center, dobutamine PET was used in selected indications but not identified in the database. We excluded data from this enrolling center and are presenting data on a total subset of 2,398 patients. Enrollment and clinical characteristics from this excluded center were similar to those reported herein. All participating centers obtained institutional review board approval for the stress imaging procedures as well as follow-up methods.
Collection of Past Medical History Data
All centers agreed upon a uniform data collection for relevant clinical history variables.10 At each center, MPI staff collected data on relevant cardiac risk factors including age, gender, hypertension, diabetes, dyslipidemia, and smoking. Prior cardiac history including myocardial infarction and coronary revascularization procedures were documented. A patient’s body mass index was calculated. Ongoing medications including beta blocker, calcium channel blocker, ACE inhibitor, nitrates, diuretic, and anti-diabetic usage were detailed in the database.
MPI Protocol and Interpretation
Patients underwent standardized PET MPI protocols as per the guidelines of the American Society of Nuclear Cardiology.13 Referred patients received Rb-82 MPI PET using dedicated PET (ECAT ART; Siemens-CTI, Knoxville, TN; Posicam HZL/R, Positron Corporation, Houston, TX) or hybrid PET/CT (Discovery Rx or STE Light Speed (16, 64 slice CT), GE Healthcare, Milwaukee, WI; Biograph 64, Siemens, Knoxville, TN) cameras. Infusion of 20-60 mCi of Rb-82 occurred during rest and stress protocol with dipyridamole (142 mcg/kg/min for 5 min) or adenosine (140 mcg/kg/min for 4-6 min) used for vasodilator stress. As stated previously, one center used dobutamine under the following circumstances: (1) bronchospastic airway disease requiring active oral steroid use or active oral theophylline, (2) systolic blood pressure <100 mmHg, (3) second or third degree AV block without pacemaker in place, (4) patients on oral dipyridamole, and (5) caffeine within 12 h. Although this represented an estimated small proportion of patients (i.e., <5 %), documentation of dobutamine use was not reported in their database. The current analysis represents all included centers minus this enrolling site. In a separate analysis, the presented findings were similar to that from the entire registry. We chose to include only this smaller series so as to affirm that the heart rate changes were solely documented following vasodilator stress MPI.
Standardized MPI interpretation was applied including segmental scoring (using the 17 segment scoring system). Based on the 17-segment scores, the summed rest and stress scores were calculated and categorized into <5 %, 5-9.9 %, and ≥10 % abnormal myocardium.14,15 A subset of 2,097 patients had rest left ventricular ejection fraction (LVEF) measurements obtained; as previously reported.9,10 The rest LVEF was categorized as ≤45 % and >45 %. Rest and maximum heart rate measurements before and following intravenous vasodilator stress were recorded. As well, rest and maximum blood pressure measurements were also recorded.
HRR was defined as subtracting the peak minus the resting heart rate (in beats per minute, bpm). HRR was categorized into tertiles for the following measurements including a change of ≤4, 5-14, and ≥15 bpm. These tertiles were chosen based on the approximate equal size of the tertiles as well as the convenience of the cut-points.
Follow-Up Methods
A more detailed description of follow-up methodologies has been reported.10 The primary endpoint for this analysis was coronary artery disease (CAD) death. The timing and occurrence of CAD mortality was documented for all patients. CAD mortality was described as time to first occurrence causing a fatal event (fatal myocardial infarction, arrhythmia, or primary cardiovascular abnormality including death from end-stage CAD or heart failure). The timing and occurrence of all-cause death was also documented.
Each institution employed a scripted telephone interview that was employed during patient or family member contact. The interviews were supplemented by review of the patient’s electronic medical record or by confirmation of the patient’s primary care physician. For US centers, the national death index was queried for ascertainment of survival status of patients during the study time period. The follow-up time period was, on average, 1.9 ± 0.9 years. For all survival analysis, the number of patients at-risk was documented during each year of follow-up.
Statistical Methods
Descriptive statistics were employed to compare clinical and MPI data by the HRR tertiles using linear-by-linear association Χ2 statistics. For rest and stress blood pressure measurements, we compared average measures by HRR tertiles using analysis of variance techniques.
We estimated the HRR ≤4 bpm using a multivariable logistic regression model. All candidate variables were based on prior literature including drug types (e.g., beta blockers) and clinical patient subsets (e.g., diabetics, advanced age) known to influence HRR. Model overfitting procedures were considered by limiting the final model to 1 variable for every 10 outcomes. From the multivariable model, the adjusted odds ratio and 95 % confidence intervals (CI) were calculated. We report on the model Χ2 statistic and model classification rate from the multivariable model in Table 2. The Hosmer and Lemeshow and Nagelkerke r 2 statistics were also reported. For PET data, we included the stress MPI % abnormal myocardium and categorical rest LVEF variables. The % ischemic myocardium was also included as a covariate but was not statistically significant (P = 0.99) and not presented.
The primary endpoint for this analysis was time to CAD mortality. A total of 64 CAD deaths were observed during follow-up. Univariable and multivariable Cox proportional hazards models were calculated. C statistics were calculated from the Cox models. From the univariable Cox model, we plotted time to CAD mortality for the HRR tertiles. Crude CAD mortality rates were compared for HRR tertiles and LVEF subsets using Χ2 statistics. From the Cox models, an unadjusted or adjusted hazard ratio and 95 % CI was calculated. The predicted or adjusted CAD mortality rates were calculated from the multivariable Cox model. These rates were annualized by dividing the predicted rate by the years of follow-up. These predicted rates were compared by HRR tertiles, stress MPI % abnormal myocardium, and in elderly (age ≥65 years) and non-elderly (age <65 years) patients. A receiver operating characteristics (ROC) curve analysis was employed to classify CAD mortality for rest and stress MPI % abnormal myocardium. In the ROC analysis, the area under the curve and 95 % CI was calculated. As well, the continuous and categorical net reclassification improvement (NRI) statistics as well as 95 % bootstrap CI was calculated. The categories for the NRI analysis included <1 %, 1-3.9 %, and ≥4 % annual CAD mortality.
We created a variable that combined the HRR and MPI % abnormal myocardium. The ranking for the HRR from low to high risk was ≥15, 5-14, and ≤4 bpm. The ranking for the % abnormal myocardium from low to high risk was <5 %, 5-9.9 %, and ≥10 %. For this variable, we classified a HRR ≥ 15 bpm and <5 % abnormal myocardium as the comparator and as the lowest risk group. All other subsets combining the rankings of HRR and % abnormal myocardium were evaluated in terms of the relative hazards when compared to this lowest risk group. Two combined HRR and MPI PET variables were calculated including the rest MPI % abnormal myocardium and stress MPI % abnormal myocardium.
We also developed a multivariable Cox model that included a priori chosen clinical and MPI variables. Only 1 variable for every ten deaths was included in this model. The proportional hazards assumption was assessed by visual examination of Logs(−Log) plot of survival curve; with all plotted lines being parallel. We also developed a multivariable model that included beta blocker therapy use and a first-order interaction of beta blocker use ×HRR as covariates. These variables were evaluated to examine if any attenuated impact of HRR on CAD mortality could be observed. For the final model, we included known CAD and not rest LVEF due to the reduced sample size available with this latter measure.
Results
Clinical Descriptors of the Patient Cohort by Changes in Heart Rate (Table 1)
From the 2,398 patients, a total of 480, 867, and 1,051 patients had HRR of ≤4, 5-14, and ≥15 bpm following vasodilator stress (Table 1). When categorized using these tertiles for HRR, patients with the lowest category of a ∆ ≤ 4 bpm were generally older, more often male, with prevalent CAD risk factors, and a prior history of known CAD. As expected, those patients with the lowest HRR had a higher (on average) resting heart rate and a lower (on average) peak stress heart rate (P < 0.0001 for both comparisons).
In the subset of patients with the lowest HRR (i.e., ≤4 bpm), >40 % had ≥10 % of the myocardium abnormal at rest and nearly one-third had a resting LVEF ≤ 45 % (P < 0.0001 for both comparisons). Similarly, this patient subset with a HRR of ≤4 bpm were also more likely to have mild-moderately abnormal stress MPI with ≥5 % abnormal stress myocardium in more than half of patients (P < 0.0001).
As expected, medication usage was more prevalent in patients with a diminished HRR following vasodilator stress. Of note, 67 % of patients with a HRR of ≤4 bpm were on beta blockers.
Multivariable Logistic Regression Model Estimating HRR ≤ 4 bpm
Table 2 reports on a multivariable model estimating diminished HRR ≤ 4 bpm. As expected, drug treatment with beta blocker (P = 0.027) and diuretic (P = 0.006) use was associated with a higher adjusted odds for a diminished HRR. As previously reported,7 diabetes was associated with a higher adjusted odds of a diminished HRR ≤ 4 bpm (OR 1.33, 95 % CI 1.04-1.69, P = 0.023). For every decile of age, the adjusted odds of a diminished HRR ≤ 4 bpm increased 1.32-fold (95 % CI 1.20-1.45, P < 0.0001).
With regards to MPI variables, rest LVEF ≤ 45 % was associated with an adjusted OR of 2.49 (95 % CI 1.90-3.27, P < 0.0001) for a diminished HRR. For every 5 % increase in the % abnormal myocardium at stress MPI, the adjusted odds of a diminished HRR ≤ 4 bpm was 1.11 (95 % CI 1.02-1.21, P = 0.019). In a multivariable model, the % ischemic myocardium was not associated with a diminished HRR (P = 0.99).
Estimation of CAD Mortality by Heart Rate Response and Rb-82 PET MPI Findings
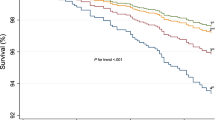
In this cohort of 2,398 patients, a total of 64 CAD deaths were observed during 1.9 ± 0.9 years of follow-up. Cox survival was 3.8 % at 3 years of follow-up for the overall patient cohort. When stratifying by the tertile HRR from rest to peak stress, unadjusted Cox mortality was 12.8 %, 3.4 %, and 0.8 %, respectively, for HRR measurements of ≤4, 5-14, and ≥15 bpm (Figure 1, P < 0.0001). The relative hazard for CAD death was 5.7 (95 % CI 2.1-14.9, P < 0.0001) and 18.7 (95 % CI 7.3-47.7, P < 0.0001) for patients with a HRR of 5-14 and ≤4 bpm.
CAD Mortality and Resting LVEF
CAD mortality rates may be further subdivided by the patient’s resting LVEF measurement (Figure 2, n = 2,097). In Figure 2, for the 1,710 patients with preserved resting LVEF > 45 %, the annual CAD mortality rates ranged from 0.3 % to 2.8 % for patients with a HRR from ≥15 to ≤4 bpm (P = 0.001). By comparison, in the setting of a resting LVEF ≤ 45 % (n = 387), the annual CAD mortality rates ranged from 1.2 % to 14.2 % for patients with a change in heart rate from ≥15 to ≤4 bpm (P = 0.001). The crude CAD mortality rates were significantly higher for patients with a resting LVEF ≤ 45 % but only for the lower 2 tertiles of HRR measurements of 5-14 and ≤4 bpm (P < 0.0001). No differences were reported in the annual CAD mortality for patients with a HRR of ≥15 bpm regardless of their LVEF measurement (P = 0.26).
CAD Mortality and Rest/Stress MPI Findings
When the HRR measurements were integrated with the stress MPI % abnormal myocardium, both variables were independently and highly predictive of CAD mortality. In Table 3, the adjusted (controlling for diabetes, age, known CAD, gender, and hypertension) CAD mortality was compared to patients with a low risk stress MPI PET (i.e., <5 % abnormal myocardium) and HRR ≥ 15 bpm. For all of the subsets of patients with a low risk MPI PET, the HRR was associated with similar CAD mortality (P = 0.11 for 5-14 and P = 0.09 for ≤4 bpm). When compared to patients with a low risk MPI PET and a HRR ≥ 15 bpm, the relative hazard for CAD mortality ranged from 16.8 for those with a HRR of 5-14 bpm to 63.7 with a HRR ≤ 4 bpm in the subset of patients with a mildly abnormal MPI scan. For those with ≥10 % abnormal stress myocardium, there was a graded relationship between HRR and CAD mortality with adjusted hazards ranging from 18.0 (P = 0.01) to 146.0 (P < 0.0001) for measurements from ≥15 to ≤4 bpm when compared to a low risk MPI PET and elevated HRR ≥ 15 bpm.
In a separate analysis, we also examined the inter-relationship between the rest MPI % abnormal myocardium and HRR (Table 3). Even in the setting of a low risk, rest MPI (<5 % abnormal myocardium), reduced HRR measurements were significant estimators of CAD mortality (≤4 bpm: P < 0.0001) and 5-14 bpm: P = 0.007) when compared to patients with HRR of ≥15 bpm. Patients with moderate-severely abnormal myocardium at rest had the highest relative hazard for CAD mortality; ranging from 10.5 (P = 0.01) to 75.9 (P < 0.0001) for HRR measures from ≥15 to ≤4 bpm.
Multivariable Model Estimating CAD Mortality
Table 4 reports the clinical multivariable model for estimating CAD mortality. In this model, the HRR variable was independently predictive of CAD mortality (P < 0.0001) with adjusted hazards in the range of 3.5-8.4. In a separate stepwise model, the % abnormal stress myocardium and HRR were rated as the two strongest estimators of CAD mortality. In prior clinical models, age was prominent and highly predictive of CAD mortality. When known CAD, HRR, and stress MPI % abnormal myocardium were added to the predictive model, age was of borderline significance in estimating CAD mortality (P = 0.076). In a related model, an interaction of beta blocker therapy by the HRR variable was not statistically significant (Table 5, P = 0.97).
This relationship may also be illustrated by plotting the annual CAD mortality rates by the % abnormal stress myocardium and HRR tertiles in elderly and non-elderly patients (Figure 3). There was a similar gradient relationship between HRR and stress MPI % abnormal myocardium. For younger patients <65 years of age, those at high risk were patients with ≥10 % abnormal stress myocardium, the annual CAD mortality rates ranged from 0.9 % for 7.5 % for those with HRR measurements of ≥15 to ≤4 bpm (P < 0.0001). Similarly, for elderly patients, the annual CAD mortality rates ranged from 1.3 % for 9.2 % for those with HRR measurements of ≥15 to ≤4 bpm (P < 0.0001). Patients with a low risk, stress MPI (i.e., <5 % abnormal myocardium) and elevated HRR measurement (≥15 bpm) had a very low risk of CAD death per year (0.1 %).
Gradient of annual adjusted * cardiac mortality for abnormal stress myocardial perfusion results (by % myocardium) and change in heart rate (defined as peak minus resting heart rate with pharmacologic stress). This figure shows an inverse relationship between the change in heart rate with pharmacologic stress and more extensive and severely abnormal stress myocardial perfusion PET imaging results
In two separate multivariable models, we examined the added independent value of HRR over and above resting HR. In Table 6, the first model reports that resting HR was highly predictive of CAD mortality (P = 0.0022) over and above the stress MPI % abnormal myocardium, age, hypertension, and smoking. However, in the second model, when HRR was added to the model, resting HR was no longer statistically significant (P = 0.36) and the HRR was highly significant (P < 0.0001).
CAD Death Classification Analysis
We examined the ability of the combination of % abnormal myocardium with the HRR variable to classify CAD mortality (Figure 4). The combination of stress MPI % abnormal myocardium with the variable HRR exhibited a high area under the curve for classifying CAD mortality (0.86, P < 0.0001). The combination of the rest MPI % abnormal myocardium with the HRR variable had an area under the curve of 0.81 for classifying CAD mortality (P < 0.0001).
Receiver operating characteristics curve analysis estimating cardiac mortality for the: 1 combination of the heart rate Δ and % rest abnormal myocardium, and 2 combination of the heart rate ∆ and % stress abnormal myocardium. The area under the curve and asymptotic 95 % confidence intervals are reported in the table
When compared to a multivariable model including resting HR, the categorical NRI for the HRR was 0.18 (95 % CI 0.02-0.35) (Table 6) when compared to a model that included the resting HR as well as risk factors and the stress MPI % abnormal myocardium. The proportion of events and non-events that were correctly reclassified with HRR was 10.8 % and 7.7 %.
Discussion
The inability of the heart rate to increase normally with exercise,2,16 during a timed walk,17 or, as in the current analysis, with pharmacologic stress4,5,7 has important implications for the detection of at-risk patients undergoing stress testing. The majority of evidence on changes in heart rate is reported for patients undergoing exercise testing.2,3,16,18 The exercise testing literature identifies an impaired chronotropic response as a major predictor of cardiovascular outcomes.2,3,16,19 From the current series, the measurement of the HRR to vasodilator stress was highly predictive of CAD mortality. In fact, CAD mortality was as high as 12.8 % for patients with a diminished HRR of ≤4 bpm (P < 0.0001) following administration of a vasodilator stressor. Conversely, CAD mortality was low for patients with high HRR measurements ≥15 bpm; often <1 % annual CAD mortality rates. Interestingly, there was a synergistic relationship between rest and stress MPI findings and HRR. Such that, the adjusted hazard for CAD mortality increased with the % abnormal myocardium on rest and stress MPI and was further exacerbated based on the HRR measurements. This data is consistent with previous single center registry data that identified a diminished HRR to vasodilator stress as prognostically significant.6-8
Impaired Chronotropic Response and CAD Mortality
The body of evidence on the prognostic significance of changes in heart rate to stress has largely been put forth in exercising patients.2,3,16 In these reports, a failure to achieve predicted maximum heart rate of 85 % or greater at maximal exertional stress or a defined reduced peak heart rate (e.g., <110-120 bpm at peak exercise) is consistently reported and validated as prognostically important.3,20-23 The common definition for an impaired chronotropic response is a failure of the heart to adequately increase its beating rate commensurate with the higher metabolic demands of graded exercise.3 For pharmacologic stress, one may similarly propose to define an impaired chronotropic response as a failure to adequately increase the heart rate commensurate with the vasodilatory action of the infused pharmacologic stressor. The normative response to infusion of a vasodilating stress agent is a drop in blood pressure that is associated with a compensatory increase in heart rate. Although one may subset this data many ways, we defined the HRR by categorizing the HRR into tertiles of ≤4, 5-14, and ≥15 bpm. These results indicate that patients with a diminished heart rate reserve of ≤4 bpm are at high risk of CAD mortality. Our analysis revealed an improved risk reclassification (NRI = 0.18) with the addition of HRR to a model including resting heart rate. However, the risk associated with HRR is augmented in the setting of mild (5-9.9 % of the myocardium) to moderate-severely (≥10 % of the myocardium) abnormal stress MPI findings with relative hazards for CAD death in excess of 50-times higher than that of patients with low risk MPI (<5 % of the myocardium) and a normal HRR ≥ 15 bpm (P < 0.0001). In the current series and as previously reported,4-7 the HRR was independently associated with CAD mortality. In a recent report on rest-stress Rb-82, the change in heart rate following dipyridamole infusion was inversely related to all-cause death (P = 0.0006).6 That is, the lower the HRR, the higher the all-cause death rates. In the current report, similar findings were reported with those at highest CAD mortality risk having a HRR of ≤4 bpm.
Key Patient Subsets with Abnormal HRR
The underlying etiology for an abnormal HRR has been reported to be autonomic dysfunction which is prevalent in patients with CAD, left ventricular dysfunction, and in diabetics.3,7,24-26 Our report similarly highlights the greater prevalence of impaired HRR (≤4 bpm) in subsets of diabetics, in older age subgroups, and in patients with an impaired LVEF. Of the latter group, a subset of 2,097 had resting LVEF measurements. In this group, the estimated annual CAD mortality rates were demonstrably higher for patients with impaired systolic function and a diminished HRR (Figure 2). Specifically, for patients with a HRR of ≤4 bpm, the annual CAD mortality rate was 14.2 % versus 2.8 % for patients with rest LVEF measures of ≤45 % and >45 % (P < 0.0001). A similar relationship was reported for patients with intermediate HRR values of 5-14 bpm (P < 0.0001). However, in patients with preserved HRR of 15 bpm or greater, there was no difference in the CAD death rates for patients with and without impaired rest LVEF (P = 0.26). We also reported a synergistic relationship between the resting MPI abnormalities and HRR. These data support the prognostic strength of HRR measures as highly predictive of CAD mortality and an important means to risk stratify patient subsets with expectedly high death risk (i.e., patients with systolic dysfunction or scarred myocardium).
HRR and the Aging Cardiovascular System
With regards to aging, there is a well-established relationship whereby maximal heart rate values decline with age.3 That is the rationale for the commonly used measure to predict maximal heart rate which is inclusive of patient age.2 One may postulate that our analysis of the prognostic significance of HRR is merely emulating the age-related effects on the vascular system and the higher CAD mortality risk associated with advanced age. Historically, age is commonly the most prominent prognostic variable in multivariable models. Interestingly, in our cohort, the inclusion of HRR into the Cox models attenuated the influence of age, such that there was only a trend toward significance in estimating CAD mortality (P = 0.076). These data imply that the prognostic significance of patient age may be better elucidated by examining the HRR to stress. In our analysis, higher CAD death rates were reported for elderly patients but were low for the aged with preserved HRR ≥ 15 bpm. From the Cardiovascular Health Study of older subjects (mean age: 77 years), the lowest tertile of HRR (<20 bpm) with a timed 6-min walk was associated with a 20 % increase in mortality risk.17 Moreover, this analysis also confirms an earlier analysis by Abidov and colleagues8 showing the importance of HRR in older patients. In this report of 3,444 patients who were 55 years of age and older, resting and peak HR were independently predictive of CAD mortality. From this series,8 the beta coefficient for CAD mortality was positive (β = 0.042) suggesting that those with higher resting HR had an elevated death risk. As well, the beta coefficient for CAD mortality was negative (β = −0.026) suggesting that those with a lower peak HR had an elevated death risk. Combining this result renders findings similar to the current analysis that a diminished HRR was a highly significant estimator of CAD mortality.
Study Limitations
Limitations to this registry have been previously defined by Dorbala et al.10 We included a consecutive series of patients and, as such, our findings reflect the pattern of testing from the participating institutions. Selection bias is operational and may have influenced our findings. Our findings do validate prior series6-8 and support the consistency of the prognostic relationships reported herein. Data were collected prospectively but with limited depth of detail on past medical history of enrolled patients. A greater depth of detail in key patient subsets including symptom burden and onboard medications may have provided further detail as to the relationship between HRR and prognosis. Specifically, we did not evaluate the potential influences of arrhythmias and prescribed anti-arrhythmic medication. Moreover, the presence of electrocardiographic rhythm abnormalities including atrial fibrillation or a paced rhythm was not available. We did not compare the type of vasodilatory agent and combined all pharmacologic stressors with a vasodilatory mechanism of action together. We attempted to control for the influence of beta blockers and other drugs which have an effect on heart rate. Information was unavailable with regards to pre-test caffeine intake. However, additional details on dosing or type of prescribed drug were not available which may further defined, for example, the short- or long-term effects of beta blockade on HRR. Irrespective of medications involved, we employed a tertile analysis to define HRR subsets. Although we examined other approaches, alternative categorization may have resulted in a varied analysis to that reported in the current manuscript.
New Knowledge Gained
Simple measures, often minimized in lieu of more advanced imaging risk markers, can provide important clues as to patient risk. The current report details the prognostic significance of heart rate reserve (HRR) measures obtained during pharmacologic stress PET imaging from a multicenter registry. We reported that the simple HRR independently risk stratifies and improves risk reclassification over and above clinical and PET variables. This finding validates prior reports on the prognostic significance of heart rate measurements with exercise and single site reports using SPECT imaging.
Conclusion
Data from this PET prognosis multicenter registry demonstrates that a diminished HRR to vasodilator stress was an independent predictor of CAD mortality. We simplified the HRR measurements by categorizing them into subsets of ≤4, 5-14, and ≥15 bpm. Consistent with prior findings that report on the prognostic significance of impaired chronotropic responses with exercise, the current report details the relationship between HRR and MPI findings as they relate to CAD mortality. From the current series, CAD mortality was high in patients with a diminished HRR of ≤4 bpm (P < 0.0001) following administration of vasodilator stress while CAD mortality was low for patients with high HRR measurements (≥15 bpm); with <1 % annual CAD mortality rates. In particular, high risk elderly and patients with systolic dysfunction were effectively risk stratified based on HRR measurements. These data underscore the importance of optimizing readily available novel markers of risk as highly relevant to identifying high and low risk patient subsets.
References
Fihn SD, Gardin JM, Abrams J, et al. ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44-164.
Gulati M, Shaw LJ, Thisted RA, Black HR, Bairey Merz CN, Arnsdorf MF. Heart rate response to exercise stress testing in asymptomatic women: the St. James women take heart project. Circulation. 2010;122:130-7.
Brubaker PH, Kitzman DW. Chronotropic incompetence: causes, consequences, and management. Circulation. 2011;123:1010-20.
Hage FG, Dean P, Bhatia V, Iqbal F, Heo J, Iskandrian AE. The prognostic value of the heart rate response to adenosine in relation to diabetes mellitus and chronic kidney disease. Am Heart J. 2011;162:356-62.
Hage FG, Iskandrian AE. Cardiac autonomic denervation in diabetes mellitus. Circ Cardiovasc Imaging. 2011;4:79-81.
Ling LF, Marwick TH, Flores DR, et al. Identification of therapeutic benefit from revascularization in patients with left ventricular systolic dysfunction: inducible ischemia versus hibernating myocardium. Circ Cardiovasc Imaging. 2013;6:363-72.
Hage FG, Dean P, Iqbal F, Heo J, Iskandrian AE. A blunted heart rate response to regadenoson is an independent prognostic indicator in patients undergoing myocardial perfusion imaging. J Nucl Cardiol. 2011;18:1086-94.
Abidov A, Hachamovitch R, Hayes SW, et al. Prognostic impact of hemodynamic response to adenosine in patients older than age 55 years undergoing vasodilator stress myocardial perfusion study. Circulation. 2003;107:2894-9.
Kay J, Dorbala S, Goyal A, et al. Influence of gender on risk stratification with stress myocardial perfusion Rb-82 positron emission tomography: results from the PET prognosis multicenter registry. J Am Coll Cardiol. 2013;62(20):1866-76. doi:10.1016/j.jacc.2013.06.017.
Dorbala S, Di Carli MF, Beanlands RS, et al. Prognostic value of stress myocardial perfusion positron emission tomography: results from a multicenter observational registry. J Am Coll Cardiol. 2013;61:176-84.
Dorbala S, Hachamovitch R, Curillova Z, et al. Incremental prognostic value of gated Rb-82 positron emission tomography myocardial perfusion imaging over clinical variables and rest LVEF. JACC Cardiovasc Imaging. 2009;2:846-54.
Merhige ME, Breen WJ, Shelton V, Houston T, D’Arcy BJ, Perna AF. Impact of myocardial perfusion imaging with PET and (82)Rb on downstream invasive procedure utilization, costs, and outcomes in coronary disease management. J Nucl Med. 2007;48:1069-76.
Hachamovitch R, Rozanski A, Shaw LJ, et al. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012-24.
Dilsizian V, Beanlands S et al. ASNC IMAGING GUIDELINES FOR NUCLEAR CARDIOLOGY PROCEDURES: PET myocardial perfusion and metabolism clinical imaging. http://www.asnc.org/imageuploads/ImagingGuidelinesPETJuly2009.pdf. 2009. Accessed December 7 2012.
Lauer MS. Chronotropic incompetence: ready for prime time. J Am Coll Cardiol. 2004;44:431-2.
Girotra S, Kitzman DW, Kop WJ, Stein PK, Gottdiener JS, Mukamal KJ. Heart rate response to a timed walk and cardiovascular outcomes in older adults: the cardiovascular health study. Cardiology. 2012;122:69-75.
Myers J, Tan SY, Abella J, Aleti V, Froelicher VF. Comparison of the chronotropic response to exercise and heart rate recovery in predicting cardiovascular mortality. Eur J Cardiovasc Prev Rehabil. 2007;14:215-21.
Khan MN, Pothier CE, Lauer MS. Chronotropic incompetence as a predictor of death among patients with normal electrograms taking beta blockers (metoprolol or atenolol). Am J Cardiol. 2005;96:1328-33.
Singh JP, Larson MG, O’Donnell CJ, Tsuji H, Evans JC, Levy D. Heritability of heart rate variability: the Framingham Heart Study. Circulation. 1999;99:2251-4.
Kupper NH, Willemsen G, van den Berg M, et al. Heritability of ambulatory heart rate variability. Circulation. 2004;110:2792-6.
Gerstenblith G, Lakatta EG, Weisfeldt ML. Age changes in myocardial function and exercise response. Prog Cardiovasc Dis. 1976;19:1-21.
Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37:153-6.
Cay S, Ozturk S, Biyikoglu F, et al. Association of heart rate profile during exercise with the severity of coronary artery disease. J Cardiovasc Med. 2009;10:394-400.
Halon DA, Dobrecky-Mery I, Gaspar T, et al. Heart rate recovery after exercise and coronary atheroma in asymptomatic individuals with type 2 diabetes mellitus: a study using 64-slice coronary CT angiography. Int J Cardiol. 2010;145:102-3.
Seshadri N, Acharya N, Lauer MS. Association of diabetes mellitus with abnormal heart rate recovery in patients without known coronary artery disease. Am J Cardiol. 2003;91:108-11.
Disclosures
This study was supported in part by an unrestricted grant from Astellas Pharma Global Development, Bracco Diagnostics, Inc., National Heart, Lung, and Blood Institute grant (K23HL092299) and by a program grant from the Heart and Stroke Foundation of Ontario (#PRG6242). Dr. Beanlands is a Career Investigator supported by the Heart and Stroke Foundation of Canada.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi: 10.1007/s12350-014-9860-1
Rights and permissions
About this article
Cite this article
Bellam, N., Veledar, E., Dorbala, S. et al. Prognostic significance of impaired chronotropic response to pharmacologic stress Rb-82 PET. J. Nucl. Cardiol. 21, 233–244 (2014). https://doi.org/10.1007/s12350-013-9820-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9820-1