Abstract
Background
Previous studies have reported a favorable outcome of patients with normal single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI). The aim of this study was to assess the very long-term prognosis of patients with known coronary artery disease (CAD) and normal SPECT MPI results.
Methods
The population consisted of 266 patients with known CAD (defined as a healed myocardial infarction and/or a previous coronary revascularization), who underwent exercise bicycle or dobutamine-atropine stress SPECT MPI and had normal perfusion during stress and at rest. End points during follow-up were all-cause mortality, cardiac mortality, and nonfatal myocardial infarction. Univariate and multivariate analyses were performed to identify predictors of long-term outcome.
Results
Follow-up was completed in 261 (98%) patients. During a median follow-up of 12 years, 94 (36%) patients died, of which 26 (10%) died due to cardiac causes, and 15 (6%) had a nonfatal myocardial infarction. The annualized mortality rate was 3.1%, annualized cardiac mortality rate was 0.9%, and the annualized event rate for cardiac death and/or nonfatal infarction was 1.2%. Independent predictors of total mortality were age, diabetes mellitus, and rate-pressure product at peak stress. Independent predictors of cardiac mortality were age, male gender, and rate-pressure product at peak stress.
Conclusion
Patients with known CAD and a normal SPECT MPI study have a favorable long-term prognosis. Clinical and stress test variables can be used to identify patients with a higher risk status.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is a widely used tool for the assessment of prognosis in patients with known or suspected coronary artery disease (CAD). Multiple studies have reported a favorable outcome of patients with a normal SPECT MPI study.1-4 A recent meta-analysis4 pooled the results of 17 studies, including 8,008 patients, and confirmed that a normal stress MPI has a high negative predictive value for cardiac events during a median follow-up 3 years. The proportion of patients with a previous myocardial infarction varied from 0% to 55% in the studies included in that meta-analysis.4 Assessment of prognosis is particularly relevant in patients with known CAD, i.e., after myocardial infarction and/or previous coronary revascularization. Currently, information on the prognostic implications of a normal stress MPI in patients with known CAD is limited. Moreover, very long-term follow-up data in patients with known CAD and with normal SPECT MPI are not available. This creates uncertainties in patient management recommendations. Therefore, the aim of this study was to determine the long-term prognosis of patients with a known CAD and normal stress SPECT MPI results.
Methods
Study Design
The study included 266 patients, with known CAD, defined as a previous myocardial infarction and/or previous coronary revascularization, who underwent a stress SPECT MPI between November 1990 and March 2003, and had normal myocardial perfusion during stress and at rest. The medium-term outcome of 147 of these patients has been previously reported.5 The patients underwent an exercise bicycle or a dobutamine-atropine stress SPECT MPI study. The type of stress test was selected based on the patient’s ability to exercise. The test was requested for evaluation of myocardial ischemia in all patients. Patients who underwent coronary revascularization within 60 days of myocardial perfusion imaging were excluded from analysis. In these patients, the decision to revascularize may be influenced by test results. All patients gave informed consent before the test. The local medical ethics committee approved the study protocol. Before the stress test, a structured clinical interview and cardiac risk factors were acquired. Hypertension was defined as a blood pressure ≥140/90 mm Hg or treatment with antihypertensive medication. Diabetes mellitus was defined as a fasting glucose level ≥7.8 mmol/L or the need for insulin or oral hypoglycemic medication. Hypercholesterolemia was defined as a total cholesterol level ≥6.4 mmol/L or treatment with lipid-lowering medication.
Stress Test Protocol
Symptom-limited, upright, bicycle ergometry with stepwise increments of 20 W every minute was performed according to a standard protocol.6 Three electrocardiographic leads were continuously monitored. Cuff blood pressure measurements and 12-lead electrocardiograms were recorded at rest and every minute during exercise and recovery. In patients who were unable to perform exercise tests, dobutamine stress testing was performed as previously reported.7 Dobutamine was administered intravenously, starting at a dose of 5 μg/kg/minutes for 3 minutes, then 10 μg/kg/minutes for 3 minutes, increasing by 10 μg/kg/minutes every 3 minutes up to a maximum dose of 40 μg/kg/minutes. If the test endpoint was not reached at a dobutamine dose of 40 μg/kg/minutes, atropine (up to 2 mg) was given intravenously. Blood pressure, heart rate, and electrocardiography were monitored continuously. Test endpoints were achievement of target heart rate (85% of maximum age- and gender-predicted heart rate), horizontal or downsloping ST-segment depression >2 mm at an interval of 80 ms after the J point, ST-segment elevation >1 mm in patients who had no previous myocardial infarction, severe angina, systolic blood pressure decrease >40 mm Hg, blood pressure >240/120 mm Hg, or significant cardiac arrhythmias.
SPECT MPI
An intravenous 370-MBq dose of 99mTc-tetrofosmin or 99mTc-sestamibi was administered ~1 minute before termination of the stress test. For studies at rest, 370 MBq of the same tracer was injected ≥24 hours after stress testing. Image acquisition was performed with a triple-head γ-camera system (Prism 3000 XP, Picker International, Cleveland, Ohio). Projections were obtained over a 180° arc, from the left posterior oblique to right anterior oblique views. Images were reconstructed using a filtered back projection algorithm and a ramp reconstruction filter. Forty-seven segments were identified (3 long axis and 44 short axis), as described previously.7 Tomographic views during stress and at rest were reviewed side by side by an experienced observer who was unaware of patients’ clinical data. A reversible perfusion defect was defined as a perfusion defect on stress images that partly or completely resolved at rest in ≥2 contiguous segments or slices in the 47-segment model. A fixed perfusion defect was defined as a perfusion defect on stress images in ≥2 contiguous segments or slices that persisted on images at rest in the 47-segment model. An abnormal study result was considered in the presence of a fixed and/or reversible perfusion defect. Patients who presented with abnormal perfusion were not included per enrolment criteria.
Follow-Up
Follow-up was successful in 261 (98%) patients. Clinical outcome data were obtained by reviewing hospital records and by contacting patients’ general practitioners. Vital status was verified through data from the civil registry. All patients alive were sent a questionnaire to retrieve the major cardiac events, which were checked against the hospital’s records. Events that were noted during follow-up were all-cause mortality, cardiac mortality, and nonfatal myocardial infarction. Cardiac mortality was defined as death caused by myocardial infarction, significant cardiac arrhythmias, or refractory congestive heart failure. Sudden death that occurred without another explanation was recorded as cardiac death. Myocardial infarction was defined according to standard criteria, as defined by the joint European Society of Cardiology/American College of Cardiology committee.8
Statistical Analysis
Statistical analysis was performed using SPSS statistical software version 15.0, SPSS, Chicago, IL. Continuous data are expressed as mean ± SD and percentages are rounded. Continuous variables were compared with Student’s t test for unpaired samples. Differences between proportions were compared with the χ2 test. Univariate and multivariate Cox’s proportional hazard regression models were used to identify independent predictors of outcome.9 The predictive value of each model was expressed using the χ2 statistic. The risk of a variable was expressed as a hazard ratio with a corresponding 95% confidence interval. Variables were selected in a stepwise forward selection manner with entry and retention set at a significance level of .05. To calculate the allowed number of variables for inclusion in the multivariate analysis, the square root of the number of events was used. The probability of survival was calculated using the Kaplan-Meier method. A P value <.05 was considered statistically significant.
Results
Demographics and Stress Test Results
Clinical data are presented in Table 1. The mean age was 61 ± 11 years and 49% of the patients were male. There was a significant difference in age between the patients who performed an exercise test and those who underwent dobutamine-atropine stress testing (mean age 59 vs 63 years, P = .001). Stress testing resulted in a significantly increased heart rate (72.5 ± 14.7 to 130.8 ± 21.0, P < .001), blood pressure (139.1 ± 12.9 to 171.7 ± 33.4, P < .001), and rate-pressure product (10.1 ± 2.6 to 22.6 ± 6.4, P < .001).
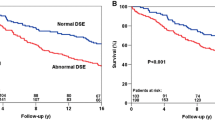
Patient Outcomes
During a median follow-up of 12 years (range 8 to 21 years), 94 patients (36%) died, of whom 26 (10%) died due to cardiac causes. Nonfatal myocardial infarction occurred in 15 patients (6%). Table 2 shows the event rates per year for total mortality, cardiac death, and cardiac death and/or nonfatal myocardial infarction. The annualized all-cause mortality rate was 3.1%. The annualized cardiac mortality rate was 0.9% (Figure 1). The annualized cardiac mortality and/or nonfatal myocardial infarction rate was 1.2% (Figure 2). The inability to perform an exercise test was associated with an impaired outcome (Figure 3).
Predictors of Long-Term Outcome
Univariate and multivariate predictors of long-term outcome are presented in Table 3. Independent predictors of all-cause mortality were age, diabetes mellitus, and rate-pressure product at peak stress. Independent predictors of cardiac mortality were age, male gender, and rate-pressure product at peak stress. Independent predictors of cardiac mortality and/or nonfatal myocardial infarction were diabetes mellitus and rate-pressure product at peak stress.
Discussion
In this study, very long-term outcome after normal stress SPECT MPI was assessed in 266 patients with known CAD, which was defined as a history of myocardial infarction and/or previous coronary revascularization. During a median follow-up of 12 years (range 8 to 21 years), the overall outcome of these patients was relatively good. The annualized event rates were relatively low during the entire follow-up period. Predictors of increased risk were identified by multivariate analysis of clinical and exercise test variables. Clinical predictors of increased risk were age, gender, diabetes mellitus, and the inability to perform an exercise stress test. Patients who were unable to perform an exercise test and underwent a dobutamine-atropine stress test had a twofold higher mortality. Stress test variables associated with an increased risk of events during follow-up were rate-pressure product at rest and rate-pressure product at peak stress.
There is strong evidence that patients with known or suspected CAD and a normal stress SPECT MPI have a favorable short- to medium-term outcome. Shaw et al3 selected 4 large observational series, including approximately 30,000 patients with normal or low-risk SPECT MPI. A meta-analysis of these 4 cohorts demonstrated an annualized all-cause mortality of 0.7% and annualized cardiac mortality rate of 0.5%. More recently, Metz et al4 performed a pooled analysis of 17 studies including 8,008 patients with normal exercise SPECT MPI results. The proportion of patients with a previous myocardial infarction varied from 0% to 55% in the studies included in the meta-analysis. During a median follow-up of 3 years, the pooled annualized cardiac mortality/nonfatal myocardial infarction rate was 0.45%.
Currently, information on the very long-term prognostic implications of a normal SPECT MPI study in patients with known CAD is limited. Patients with known CAD may have a normal SPECT MPI because of patent bypass grafts or coronary stents, or a previous small (subendocardial) myocardial infarction with a patent infarct-related artery. Previously, Schinkel et al5 studied 147 patients with known CAD and normal stress 99mTc-tetrofosmin SPECT MPI. During a mean follow-up of 6.5 ± 1.9 years annualized all-cause mortality was 2.6% in the first 3 years and 2.4% during the subsequent 3-year period (4 to 6 years of follow-up). Annualized cardiac mortality was 0.5% during the first 3 years and 1.3% during the subsequent 3-year period. The results of that study implied a very low cardiac mortality rate especially in the first 3 years after normal SPECT MPI. Georgoulias et al10 studied 246 patients 6 months after percutaneous coronary intervention using exercise 99mTc-tetrofosmin SPECT MPI. All patients were asymptomatic. During a median follow-up of 9.5 years SPECT MPI provided incremental prognostic value for the prediction of cardiac events. Patients with normal SPECT MPI results, defined as a summed stress score ≤2, had an annualized cardiac mortally/nonfatal myocardial infarction rate of 0%. Acampa et al11 studied 362 patients, 5 years after coronary bypass surgery, using exercise or dipyridamole stress 99mTc-sestamibi SPECT MPI. During a median follow-up of 27 months event-free survival was 96% in patients with normal SPECT MPI. In 2003, Hachamovitch et al12 followed 7,376 patients with normal SPECT MPI results for a mean time period of 665 ± 200 days. Patients with known CAD had significantly higher event rates as compared with patients without previous CAD. Importantly, in patients with known CAD the risk of adverse events increased with time. The authors concluded that the risk of hard events after a normal SPECT MPI, and its change over time, were a function of the clinical and historical factors of the patients tested.
This study with a median follow-up of 12 years is the first study providing information on the very long-term outcome of patients with known CAD and normal stress SPECT MPI results. This knowledge may aid clinical decision making and follow-up in patients with known CAD. Risk stratification is particularly relevant in patients with known CAD (i.e., previous myocardial infarction, coronary artery bypass surgery, and/or previous percutaneous coronary revascularization). These patients generally have a higher risk and more comorbidities than patient cohorts reported in previous studies.4 This study has several clinical implications. During the median follow-up of 12 years, the overall outcome of these patients was relatively good. Therefore, a watchful waiting approach in these patients is justified, and routine use of additional diagnostic strategies (such as coronary angiography) can be avoided. The multivariate analysis demonstrates that several clinical parameters and stress test variables can be used to identify patients at increased risk of future cardiac events. Follow-up in patients with higher risk status should be closer. Clinical judgment of patients with known CAD is of course important, even in the presence of a normal SPECT MPI. Repeated testing or additional diagnostic procedures should be considered in patients with a change in symptoms or deterioration of clinical status.
Limitations
This study does have a few limitations. As the sensitivity of myocardial perfusion imaging is 80% to 85%, it is possible that this study has included false-negative tests. No attenuation or scatter correction was used for SPECT MPI. Application of attenuation or scatter correction may have further improved the accuracy of SPECT MPI.
Conclusion
Patients with known CAD and a normal SPECT MPI study have a favorable long-term prognosis. Clinical and stress test variables can be used to identify patients with a higher risk status.
References
Beller GA, Zaret BL. Contributions of nuclear cardiology to diagnosis and prognosis of patients with coronary artery disease. Circulation 2000;101:1465-78.
Schinkel AF, Bax JJ, Geleijnse ML, Boersma E, Elhendy A, Roelandt JR, et al. Noninvasive evaluation of ischaemic heart disease: Myocardial perfusion imaging or stress echocardiography? Eur Heart J 2003;24:789-800.
Shaw LJ, Hendel R, Borges-Neto S, Lauer MS, Alazraki N, Burnette J, et al. Prognostic value of normal exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: Results from the multicenter registry of 4,728 patients. J Nucl Med 2003;44:134-9.
Metz LD, Beattie M, Hom R, Redberg RF, Grady D, Fleischmann KE. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: A meta-analysis. J Am Coll Cardiol 2007;49:227-37.
Schinkel AF, Elhendy A, Bax JJ, van Domburg RT, Huurman A, Valkema R, et al. Prognostic implications of a normal stress technetium-99m-tetrofosmin myocardial perfusion study in patients with a healed myocardial infarct and/or previous coronary revascularization. Am J Cardiol 2006;97:1-6.
Schinkel AF, Elhendy A, van Domburg RT, Bax JJ, Vourvouri EC, Bountioukos M, et al. Incremental value of exercise technetium-99m tetrofosmin myocardial perfusion single-photon emission computed tomography for the prediction of cardiac events. Am J Cardiol 2003;91:408-11.
Schinkel AF, Elhendy A, van Domburg RT, Bax JJ, Roelandt JR, Poldermans D. Prognostic value of dobutamine-atropine stress (99m)Tc-tetrofosmin myocardial perfusion SPECT in patients with known or suspected coronary artery disease. J Nucl Med 2002;43:767-72.
Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined—A consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959-69.
Cox DR. Regression models and life-tables. J R Stat Soc (B) 1972;34:187-202.
Georgoulias P, Demakopoulos N, Tzavara C, Giannakou S, Valotassiou V, Tsougos I, et al. Long-term prognostic value of Tc-99m tetrofosmin myocardial gated-SPECT imaging in asymptomatic patients after percutaneous coronary intervention. Clin Nucl Med 2008;33:743-7.
Acampa W, Petretta M, Evangelista L, Nappi G, Luongo L, Petretta MP, et al. Stress cardiac single-photon emission computed tomographic imaging late after coronary artery bypass surgery for risk stratification and estimation of time to cardiac events. J Thorac Cardiovasc Surg 2008;136:46-51.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans. What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-013-9769-0.
Rights and permissions
About this article
Cite this article
Ottenhof, M.J.M., Wai, M.C.G.T.J., Boiten, H.J. et al. 12-Year outcome after normal myocardial perfusion SPECT in patients with known coronary artery disease. J. Nucl. Cardiol. 20, 748–754 (2013). https://doi.org/10.1007/s12350-013-9713-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9713-3