Abstract
An asymptomatic epiphrenic diverticulum (ED) was diagnosed in a man undergoing annual esophagogastroduodenoscopy (EGD) at another hospital 40 years before he presented to our hospital at age 63 years for his annual EGD. However, because substantial food retention was found in the ED, we could not confirm a lesion. After the retained food was removed endoscopically, a second EGD showed a reddish, flat lesion with an elevated mass within the ED. Endoscopic ultrasonography indicated that the elevated mass was deep in the submucosal layer. An esophagram showed that the ED was approximately 80 mm in diameter, which is considered large. An endoscopic biopsy of the lesion confirmed squamous cell carcinoma. Total esophagectomy was performed. Microscopic examination revealed well-differentiated to moderately differentiated squamous cell carcinoma invading the adventitia at the elevated lesion. The final pathological stage was pT3N0M0. There was no evidence of recurrence for 3 years during the quarterly follow-up examinations. To our knowledge, this case involved the longest asymptomatic term (40 years) since the ED was detected. A review of 18 reported cases of carcinoma in an ED indicated that advanced cancer has a poor prognosis. Periodic follow-up of ED patients is essential for early diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An epiphrenic diverticulum (ED) of the esophageal diverticula is relatively rare and is often related to esophageal motor disorders. Previously reported symptoms of ED include dysphagia, chest pain, and regurgitation [1, 2]. Serious complications such as a tracheal fistula [3], hemorrhage [4], and vocal cord paralysis sometimes develop. If symptoms develop, then surgery is usually considered; however, approximately half of ED patients are asymptomatic [5]. Esophageal diverticula can lead to carcinoma [6,7,8] due to chronic inflammation cause by food retention, similar to achalasia. Heavy consumption of alcohol and frequent smoking habits may further contribute to carcinogenesis. Moreover, the depth of tumor invasion of an ED is sometimes deeper than it appears because the absence of the muscularis propria results in thinning of the diverticulum wall, which is known as pseudodiverticulum. The prognosis is usually poor; therefore, detecting tumors at an early stage is important to improve patient outcomes.
We present advanced squamous cell carcinoma in a patient with a large asymptomatic ED. To our knowledge, this case involved the longest asymptomatic term (40 years) since the ED was detected. We reviewed the duration of the diverticulum, symptoms, treatment, and prognosis reported for 18 previous cases of esophageal cancer in the ED and present clinically significance information regarding the management of ED.
Case report
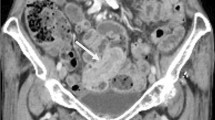
A 63-year-old man presented to our hospital with an ED. He had been diagnosed with an asymptomatic ED 40 years prior (age 23 years). He had been undergoing esophagogastroduodenoscopy (EGD) on an irregular basis; however, he had been undergoing annual EGD for the past 12 years at another hospital. He habitually drank approximately 30 g of alcohol daily and had no history of smoking. EGD was performed at our hospital. Because substantial food retention was found in the ED, we could not confirm a lesion (Fig. 1a). Therefore, after the patient fasted for 24 h, we performed a second EGD under sedation. After the retained food was removed endoscopically, a reddish, flat lesion with an elevated mass within the ED was found (Fig. 1b). The elevated mass had superficial necrosis. The entire lesion was not stained by iodine solution (Fig. 1c). Endoscopic ultrasonography (EUS) revealed that the wall of the diverticulum was devoid of a proper muscle layer. The elevated mass appeared deeper than the submucosal layer (Fig. 1d). An esophagram showed that the ED, which was approximately 80 mm in diameter, was present on the left side of the esophagus (Fig. 2). An endoscopic biopsy of the lesion confirmed the presence of squamous cell carcinoma. Therefore, total esophagectomy was performed. The pathological specimen showed that the lesion was confined to the ED and 52 × 56 mm (Fig. 3a). Microscopic examination revealed that it was well-differentiated to moderately differentiated squamous cell carcinoma that had invaded the adventitia at the elevated lesion (Fig. 3b, c). The depth of the flat area around the elevated lesion was at the level of the mucosal layer. The muscularis propria of the diverticulum was completely absent. The final pathological stage was pT3N0M0, stage IIB (Union for International Cancer Control, Geneva, 8th edition), and there was no evidence of recurrence for 3 years during the quarterly follow-up examinations.
Endoscopic findings of the epiphrenic esophageal diverticulum and tumor. a Endoscopic image showing retained food in the diverticulum. b Endoscopic image showing a reddish, flat lesion with an elevated mass in the diverticulum after removal of the retained food. c The entire lesion is not stained by iodine solution. d Endoscopic ultrasonography showing the wall of the diverticulum devoid of the proper muscle layer. The elevated mass appears to be deeper than the submucosal layer
Surgically extracted specimen and histological findings of the resected specimen. a Surgically extracted specimen: the pathological specimen shows a diverticulum containing a mass measuring 52 × 56 mm. b, c Microscopic examination (b hematoxylin and eosin (HE) stain, × 40; c HE stain, × 100). The microscopic examination reveals well-differentiated to moderately differentiated squamous cell carcinoma invading the adventitia at the elevated lesion
Discussion
Esophageal diverticula are relatively rare, with an incidence rate of 0.06–3.6% [9, 10]. They are classified as proximal, middle, and distal (epiphrenic) types. An ED usually occurs in the distal 10 cm of the esophagus, and it occurs with approximately 10% of all esophageal diverticula [3]. Diverticula occur because of herniation of the mucosa and submucosa through the muscle layers of the esophageal wall [11].
Cancer within an esophageal diverticulum is rare (0.3–3%) [12, 13]. Food retention is an important factor in its pathogenesis [6,7,8] because it increases the difficulty of endoscopic tumor detection. Moreover, the tumor in an ED easily invades the surrounding tissue because of the absence of the muscularis propria layer [14]. Therefore, if cancer in an ED is detected very late, then it may reach an advanced stage. ED management is very important, particularly periodic endoscopic observations after food retention is removed.
Eighteen cases of carcinoma in an ED were found following a PubMed search using the following search terms: “epiphrenic diverticula” and “carcinoma” or “lower esophageal diverticula” and “carcinoma.” The available clinical information is summarized in Table 1. Almost all patients underwent surgical resection of the tumor. Seven patients died due to complications associated with cancer, including surgical complications. Patients with advanced cancer (T2, T3, and T4) had a particularly poor prognosis, with a mortality rate of 54.5% (6/11). However, four patients with Tis and T1a non-invasive cancers survived. Two patients underwent surgical resection. One patient underwent additional photodynamic therapy after surgery and one patient underwent endoscopic submucosal dissection. Although these results have only been demonstrated in a few cases, they indicate that surgical resection with additional photodynamic therapy and endoscopic submucosal dissection at an early stage are essential for improving patient outcomes. To avoid a delayed diagnosis, careful ED management and correct cancer diagnoses are important. However, treatment guidelines have not been established because of the rarity of the condition.
In almost all of the reviewed cases, the patients (17/19) experienced some symptoms, such as dysphagia or regurgitation, during their clinical course. Our case, unlike those reviewed, involved an asymptomatic, long-term, large ED with tumor invasion to the deeper wall despite observation with an annual EGD. We speculate that he had become accustomed to the ED, which led him to become unaware of the symptoms. Moreover, because the cancer involved a small invasive lesion in the large diverticulum, no esophageal stricture appeared.
Surgical treatment is indicated for patients with symptomatic ED regardless of the presence of a cancerous lesion. However, it is difficult to determine whether surgery should be performed for asymptomatic patients without evidence of a cancerous lesion due to the surgical risks [11]. If surgical resection cannot be performed for an ED without a cancerous lesion, then the ED should be observed carefully with periodic EGD for early detection of cancer. Endoscopic removal of retained food in the ED under sedation, as performed for our patient, is occasionally necessary. Additional imaging studies are essential for patients when the retained food cannot be adequately removed; for example, fluorine-18 2-fluoro-2-deoxy-d-glucose positron emission tomography and computed tomography (FDG-PET/CT) may detect tumors during the early stage [15].
An accurate evaluation of the depth of cancer invasion is important when determining the treatment. Treatment strategies are different for esophageal cancer between cT1 and deeper than cT1. In the case of cT1 without metastasis, surgery or chemoradiation is performed. In cases deeper than cT1 (cT2, cT3) without metastasis, neoadjuvant chemotherapy is required before surgery. EUS is commonly used for predicting the depth of tumor invasion in patients with superficial esophageal carcinoma [16]. We believe that EUS should be performed to make informed decisions regarding the use of neoadjuvant chemotherapy. However, correctly determining the depth is sometimes difficult because the ED lacks the muscularis propria. Therefore, the depth of invasion is often underestimated. Furthermore, we believe that the diagnosis of the depth of invasion was clinically difficult in this case because the amount of cancer invading the adventitia was limited. Physicians should understand the difficulty in using EUS to diagnose an ED. For example, EUS-related complications such as a perforation, which is caused by the thin-walled diverticulum, can occur.
In conclusion, because advanced cancer with an ED has a poor prognosis, periodic follow-up and subsequent early diagnosis of cancer in the ED are important. Further studies of this rare disease should be performed to help establish appropriate diagnostic and management approaches.
References
Tedesco P, Fisichella PM, Way LW, et al. Cause and treatment of epiphrenic diverticula. Am J Surg. 2005;190:891–4.
Fisichella PM, Jalilvand A, Dobrowolsky A. Achalasia and epiphrenic diverticulum. World J Surg. 2015;39:1614–9.
Guerra JM, Zuil M, Garcia I, et al. Epiphrenic diverticula, esophageal carcinoma and esophagopleural fistula. Hepatogastroenterology. 2001;48:718–9.
Hung JJ, Hsieh CC, Lin SC, et al. Squamous cell carcinoma in a large epiphrenic esophageal diverticulum. Dig Dis Sci. 2009;54:1365–8.
Benacci JC, Deschamps C, Trastek VF, et al. Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg. 1993;55:1109–13 (discussion 14).
Philippakis M, Karkanias GG, Sakorafas GH. Carcinoma within an epiphrenic esophageal diverticulum. Case report. Eur J Surg Suppl. 1991;157:617–8.
Song YC, Zhang YD, Wang QZ, et al. Carcinoma in the esophageal diverticulum. Chin Med J. 1985;98:895–8.
Pierce WS, Johnson J. Squamous cell carcinoma arising in a pharyngoesophageal diverticulum. Cancer. 1969;24:1068–70.
Hoghooghi D, Coakley FV, Breiman RS, et al. Frequency and etiology of midesophageal diverticula at barium esophagography. Clin Imaging. 2006;30:245–7.
Watanabe S, Matsuda K, Arima K, et al. Detection of subclinical disorders of the hypopharynx and larynx by gastrointestinal endoscopy. Endoscopy. 1996;28:295–8.
Soares R, Herbella FA, Prachand VN, et al. Epiphrenic diverticulum of the esophagus. From pathophysiology to treatment. J Gastrointest Surg. 2010;14:2009–155.
Gawande AS, Batiuchok W, Barman AA, et al. Carcinoma within lower esophageal (epiphrenic) diverticulum. NY State J Med. 1972;72:1749–51.
Fujita H, Kakegawa T, Shima S, et al. Carcinoma within a middle esophageal (parabronchial) diverticulum: a case report and the review of the literature. Jpn J Surg. 1980;10:142–8.
Honda H, Kume K, Tashiro M, et al. Early stage esophageal carcinoma in an epiphrenic diverticulum. Gastrointest Endosc. 2003;57:980–2.
Eluvathingal Muttikkal TJ, Shami VM, et al. FDG positron emission tomography and computed tomography demonstration of carcinoma arising in an epiphrenic diverticulum. J Radiol Case Rep. 2014;8:42–6.
Yoshinaga S, Oda I, Nonaka S, et al. Endoscopic ultrasound using ultrasound probes for the diagnosis of early esophageal and gastric cancers. World J Gastrointest Endosc. 2012;4:218–26.
Zinner E. Carcinoma within an epiphrenic diverticulum. Bull Gastrointest Endosc. 1963;10:14–6.
Plous E, Freedman J, Wolf PL. Carcinoma within a lower esophageal (epiphrenic) diverticulum. J Thorac Cardiovasc Surg. 1964;47:129–32.
Thomas RC. Carcinoma in epiphrenic diverticula. Ann Thorac Surg. 1968;6:85–7.
Shin MS. Primary carcinoma arising in the epiphrenic esophageal diverticulum. South Med J. 1971;64:1022–4.
Saldana JA, Cone RO, Hopens TA, et al. Carcinoma arising in an epiphrenic esophageal diverticulum. Gastrointest Radiol. 1982;7:15–8.
Schultz SC, Byrne DM, De Cunzo P, et al. Carcinoma arising within epiphrenic diverticula. A report of two cases and review of the literature. J Thorac Cardiovasc Surg. 1996;37:649–51.
Lai ST, Hsu CP. Carcinoma arising from an epiphrenic diverticulum: a frequently misdiagnosed disease. Ann Thorac Cardiovasc Surg. 2007;13:110–3.
Conklin JH, Singh D, Katlic MR. Epiphrenic esophageal diverticula: spectrum of symptoms and consequences. J Am Osteopath Assoc. 2009;109:543–5.
Choi AR, Chon NR, Youn YH, et al. Esophageal cancer in esophageal diverticula associated with achalasia. Clin Endosc. 2015;48:70–3.
Fu K, Jin P, He Y, et al. A superficial esophageal cancer in an epiphrenic diverticulum treated by endoscopic submucosal dissection. BMC Gastroenterol. 2017;17:94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tomoaki Yoshida, Satoru Hashimoto, Ken-ichi Mizuno, Hiroshi Ichikawa, Junji Yokoyama, Hajime Umezu and Shuji Terai declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from the patient for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoshida, T., Hashimoto, S., Mizuno, Ki. et al. Advanced squamous cell carcinoma in an asymptomatic, large, epiphrenic esophageal diverticulum. Clin J Gastroenterol 13, 477–482 (2020). https://doi.org/10.1007/s12328-020-01098-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-020-01098-4