Abstract
Gastroesophageal reflux disease (GERD), especially reflux esophagitis (RE), is characterized by excessive esophageal acid exposure. Transient lower esophageal sphincter (LES) relaxation is the major mechanism of acid reflux episodes in both healthy subjects (HS) and patients with GERD. In the sitting position, where acid reflux episodes often occur, there is no difference in the frequency of transient LES relaxations between these two groups; however, in patients with GERD, at 5 cm above the LES, the proportion of acid reflux episodes during transient LES relaxations is significantly greater than in the HS group. This difference is considered to be one of the causes of excessive esophageal acid exposure in patients with GERD, but its cause is still unclear. A recent study, which investigated the proportion of acid reflux episodes during transient LES relaxations at 2 and 7 cm above the LES, showed that there was no difference at 2 cm above the LES between HS and patients with RE, but at 7 cm they were significantly greater in patients with RE than in HS. Evaluation of acid reflux at 2 cm above the LES is difficult to measure, but the proximal extent of refluxate could be one of the important factors of excessive acid esophageal exposure in patients with RE. Ineffective esophageal motility, found in patients with moderate to severe RE, impairs esophageal bolus clearance of acid, therefore both the proximal extent of refluxate and the delay of esophageal bolus clearance of acid could be major causes of excessive esophageal acid exposure. Hiatus hernia also causes acid reflux, due to its association with hypotensive LES, and also impairs esophageal bolus clearance of acid.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acid gastroesophageal reflux is a physiological event and even healthy subjects have several acid reflux episodes per day, but they do not have reflux esophagitis (RE). Several 24-h pH monitoring studies have shown that most patients with RE have more esophageal acid exposure than healthy subjects; therefore, it has been suggested that excessive esophageal acid exposure plays an important etiologic role in RE [1–5]. The two factors that influence esophageal acid exposure are (i) the frequency of acid reflux episodes and (ii) the length of time it takes to restore esophageal pH to normal after they occur. In addition, it has been reported that esophageal acid exposure is greater in gastroesophageal reflux disease (GERD) patients with hiatus hernia than in those without [6]; therefore, it has become evident that presence of hiatus hernia can contribute to excessive esophageal acid exposure. This review summarizes the role of excessive esophageal acid exposure in patients with GERD, including the effect of hiatus hernia on esophageal acid exposure.
Mechanisms of acid reflux episodes
Transient lower esophageal sphincter (LES) relaxation, i.e., LES relaxation not induced by swallowing, is the major mechanism underlying acid reflux episodes in both healthy subjects and patients with GERD [1–9]. In healthy subjects, the proportion of acid reflux episodes attributed to transient LES relaxations ranges between 80% and 100% [1–5, 7–9]. In patients with GERD, however, transient LES relaxation accounts for approximately 70% of acid reflux episodes [1–5, 7–9]. The remaining 30% occur during swallow-induced LES relaxation, persistently absent basal LES pressure, and straining from deep inspiration or increased intra-abdominal pressure in patients with GERD.
Approximately 90% of RE in eastern Asia, including Japan, is mild [10, 11]; however, very little has been reported on the mechanism of acid reflux episodes in patients with mild RE [1, 5]. Reports have shown that the main mechanism underlying an acid reflux episode in patients with mild RE is a transient LES relaxation and that very few acid reflux episodes occur during persistently absent LES pressure or straining. Therefore, acid reflux episodes that occur during persistently absent LES pressure and straining are the only mechanisms which can be observed in severe RE.
Transient LES relaxations
Transient LES relaxation (Fig. 1) is the single most common mechanism underlying acid reflux episodes and it is also the mechanism underlying the reflux of gas from the stomach [12], which is presumably a normal physiological mechanism for venting swallowed air from the stomach. Transient LES relaxation causes an abrupt decrease in LES pressure to the level of intragastric pressure, but it is not triggered by swallowing. A transient LES relaxation is typically of longer duration (lasting 10–45 s) than a swallow-induced LES relaxation (5–8 seconds), but the occurrence of transient LES relaxation is not related to basal LES pressure [13]. The criteria that have proved optimal for the definition of transient LES relaxation are (i) absence of a pharyngeal swallow signal for 4 s before, to 2 s after, the onset of an LES relaxation, (ii) LES pressure decrease of ≥1 mmHg/s, (iii) time from onset to complete relaxation ≤10 s, and (iv) nadir pressure of ≤2 mmHg. Excluding LES relaxation, which is associated with multiple swallows, a decrease in LES pressure of ≤2 mmHg lasting for >10 s can also be classified as a transient LES relaxation, irrespective of the time taken from LES relaxation to swallowing.
High-resolution 21-channel perfused manometric and pH recordings at 5 cm above the lower esophageal sphincter (LES) in an individual with severe reflux esophagitis. Time is on the x-axis and distance from nares is on the y-axis. A computer program was used to code and record pressures over time for each channel, as outlined in vertical color coding on the right-hand side of the figure. Anatomical landmarks, motor events, and acid reflux are labeled on the figure; an LES relaxation of approximately 30 s can be seen. There is no pharyngeal swallow signal from 4 s before, to 2 s after, the onset of LES relaxation; therefore, this LES relaxation is a transient LES relaxation. During a transient LES relaxation, regular increases of diaphragmatic hiatal pressure, due to diaphragmatic contractions during inspiration, cannot be seen and acid reflux can be seen approximately 10 s after a transient LES relaxation
The most important associated event that occurs during a transient LES relaxation is inhibition of the crural diaphragm [14], as this is essential for acid reflux to occur. While isolated LES relaxation is induced by pharyngeal stimulation, it is characteristically not associated with diaphragmatic inhibition and consequently not usually accompanied by an acid reflux episode [15].
Factors influencing the frequency of transient LES relaxations
The frequency of transient LES relaxations is influenced by a number of factors. The most important stimulus appears to be gastric distention [2, 11, 16, 17], and the most sensitive region of the stomach for initiating this response is adjacent to the gastric cardia [18]. Food is also a major stimulus for transient LES relaxation, but despite the clinical observation that high-fat food provokes reflux symptoms, its effect on patterns of acid reflux episodes has yielded conflicting results, and no significant effect that relates to the frequency of transient LES relaxations has been shown [19, 20]. Although other food and beverages such as chocolate, onions, wine, beer, and coffee have been reported to increase esophageal acid exposure, their effect on the frequency of transient LES relaxations has not been studied, and besides, it is also possible that hiatus hernia may have an effect on the frequency of transient LES relaxations. With regard to the frequency of transient LES relaxations in patients with hiatus hernia, preliminary data suggest that hiatus hernia may be responsible for increased triggering of transient LES relaxation during gastric insufflation with gas [21]; however, another study, which looked at spontaneous acid reflux episodes in patients with hiatus hernia, showed that there is no difference in the frequency of transient LES relaxations in patients with GERD, irrespective of whether or not hiatus hernia is present [6]. In that study, however, the percentage of patients with mild RE or nonerosive reflux disease was different for each group; therefore, no adequately powered single study has yet been specifically designed to evaluate the difference in the frequency of transient LES relaxations. In order to determine whether or not presence of hiatus hernia does have an effect on the frequency of transient LES relaxations, a study should be carried out according to the presence or absence of RE. When evaluating this issue, patients with RE should be of the same grade if they are included in the study.
Transient LES relaxations can also be inhibited by several factors: (i) they are substantially suppressed while in the supine position [12, 22] and (ii) they do not occur during stable sleep [9]. Acid reflux episodes that occur during nighttime sleep periods are totally confined to periods of arousal, which may last for up to 10 s [9, 23]. Stress from cold has also been shown to reduce the frequency of transient LES relaxations [24] and it has been found that, in dogs, spontaneous transient LES relaxation is completely suppressed by general anesthesia [25].
Frequency of transient LES relaxations in patients with GERD
GERD, especially RE, is characterized by excessive esophageal acid exposure. Considering the fact that transient LES relaxation is the major mechanism underlying acid reflux episodes, it is thought that either the frequency of transient LES relaxations is higher or that the proportion of acid reflux episodes during transient LES relaxations is greater; however, whether or not the former is the case in GERD is still unclear. To date, few studies that included more than 10 healthy subjects and 10 patients with GERD have directly compared the frequency of transient LES relaxations in GERD patients with that of healthy subjects, and some studies have shown a higher frequency [2, 7, 19], whereas others have not [4, 5, 8, 26–29] (Table 1). The reason for the apparent discrepancy between studies is not entirely clear, but a likely factor influencing the frequency of transient LES relaxations is posture, because as mentioned above, transient LES relaxation is substantially suppressed while in the supine position. The right lateral position is associated with more frequent transient LES relaxations and therefore there is increased likelihood of acid reflux episodes occurring while in this position than in the left lateral position. Studies that have shown a significant difference in the frequency of transient LES relaxations have been carried out with subjects in the right lateral position [2, 7, 19], but the studies which found no difference were carried out with subjects either in the sitting [4, 5, 28, 29] or supine position [26, 27]. Patients with GERD appear to have a subtle defect in postural suppression, which may be more apparent in the right lateral position than in the supine position [30]. With regard to the frequency of transient LES relaxations in the sitting position, all studies showed the same result; therefore, the frequency of transient LES relaxations in both patients with GERD and healthy subjects would appear to be similar. Considering that acid reflux episodes occur often during the postprandial period in the sitting or upright position, the frequency of transient LES relaxations seems not to have an effect on excessive esophageal acid exposure. Another factor involved in the frequency of transient LES relaxations is obesity. It has been reported that patients with GERD who are also obese have a relatively greater number of transient LES relaxations than healthy subjects [31].
Proportion of acid reflux episodes during transient LES relaxations in patients with GERD
Transient LES relaxations are not always accompanied by acid reflux episodes. In almost all studies [2, 7, 8, 19, 26, 28, 29], the proportion of acid reflux episodes during transient LES relaxations at 5 cm above the LES has been shown to be significantly greater in patients with GERD than in healthy subjects (Table 2).
A study carried out in Japan showed that the proportion of acid reflux episodes during transient LES relaxations at 5 cm above the LES was around 10% in healthy subjects and around 40% in patients with severe RE [29]. Compared with the values of other studies from mainly Western countries, these are very low. In Japan, the prevalence of Helicobacter pylori infection increases with age, reaching 70–80% in those born before 1950 [32], but as a result of Helicobacter pylori infection, gastric acid secretion decreases with age. In addition, it has been reported that the maximum gastric acid output levels in the Japanese population have increased over the past 20 years [33]; however, the levels in the Japanese population are still low compared with levels in Western populations [34]. Helicobacter pylori infection and the subsequent lower level of gastric acid output in the Japanese population may be the reason that the frequency of acid reflux episodes during transient LES relaxations is very low in the Japanese population compared with in Western populations.
Possible causes of the difference in the proportion of acid reflux episodes during transient LES relaxations between patients with GERD and healthy subjects
The proportion of acid reflux episodes during transient LES relaxations, at 5 cm above the LES, in patients with GERD, is significantly greater than that in healthy subjects, and it is clear that this difference is one of the factors responsible for excessive esophageal acid exposure in patients with GERD. However, the mechanism underlying the difference between the groups is still not clear.
In a recent study [4], which investigated the proportion of acid reflux episodes during transient LES relaxations in the sitting position, in patients with severe RE and healthy subjects, at 2 and 7 cm above the LES, it was reported that there was no difference between the groups in the frequency of transient LES relaxations or in the proportion of acid reflux episodes during transient LES relaxations, at 2 cm above the LES. At 7 cm above the LES, however, in patients with severe RE, this was significantly greater than that in healthy subjects. These findings suggest, therefore, that the difference between the groups is not the proportion of acid reflux episodes during transient LES relaxations but rather that it is the proximal extent of refluxate that is of importance. Therefore, in patients with severe RE, refluxate comes up more easily to the proximal esophagus compared with in healthy subjects.
In a subsequent study using the same protocol, the proximal extent of acid refluxate in healthy subjects and patients with both mild and severe RE was investigated [5]. The frequency of transient LES relaxations was similar in the 3 groups and the proportion of acid reflux episodes during transient LES relaxations at 2 cm above the LES was also similar in these groups. This is in line with the previous study (Fig. 2). At 7 cm above the LES, however, the proximal extent of acid refluxate was greater in patients with RE than in healthy subjects, and this difference was related to the severity of RE (Fig. 2). Considering these results, the reason for the difference in the proportion of acid reflux episodes during transient LES relaxations at 5 cm above the LES in healthy subjects and patients with mild and severe RE was not the proportion of acid reflux episodes during transient LES relaxations but rather whether or not refluxate comes up to the proximal esophagus. To date, the amount of acid reflux and esophageal bolus clearance of acid were thought to be the major factors causing excessive esophageal acid exposure in GERD. These results suggest that the proximal extent of acid refluxate might also be a very important factor in excessive acid esophageal exposure in patients with GERD. The factors responsible for the proximal extent of acid refluxate have not yet been identified.
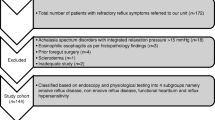
Proportion of acid reflux episodes during transient lower esophageal sphincter relaxations (TLESR) in healthy subjects (HS) and patients with both mild and severe reflux esophagitis (RE). Data are presented as median (interquartile range, IQR). Cited from Ref. [5]
The focal point of these studies is the position of the pH electrode, because there is the possibility that, if the pH electrode is placed just above the LES, it will drop into the stomach as a result of esophageal shortening after a transient LES relaxation. In these studies [4, 5] the pH electrode was placed at 2 cm above the proximal margin of the LES, which meant that it was located 50–70 mm above the bottom of the LES, because the length of the LES is about 30–40 mm. It has been reported that median esophageal shortening after a transient LES relaxation is 1.67 cm (IQR 1.0–2.4 cm) [35]. Even if the 75 percentile esophageal shortening occurs after a transient LES relaxation, the position of the pH electrode would still be at 2.4–4.6 cm above the bottom of the LES, which would be correctly positioned within the LES. In addition, the relationship between the position of the pH electrode and the LES was checked during the study using high-resolution manometry. In these studies, therefore, it would be less of a possibility that the upward motion of the LES that occurs during transient LES relaxations would carry the pH electrode down into the stomach.
Persistently absent basal LES pressure
Even though transient LES relaxation is the major mechanism of an acid reflux episode, low LES pressure is also an important mechanism. In the presence of low LES pressure, an acid reflux episode is thought to occur either freely from the stomach into the esophagus or during periods of abdominal strain. Prolonged monitoring of patterns of LES pressure in both stationary and ambulatory patients has shown that persistently absent basal LES pressure is responsible for only a small proportion of acid reflux episodes. This mechanism appears to be confined mainly to patients with severe RE and rarely occurs in patients with mild RE and nonerosive reflux disease [1, 5]. In fact, it has been reported that basal LES pressure in patients with mild RE and nonerosive reflux disease is similar to that in healthy subjects [5, 36].
The reason for low LES pressure is not entirely clear. It is possible, however, that it is due to primary myogenic or neurogenic failure of the LES muscle, but even though there are no definitive data to prove this, it is entirely possible that low LES pressure is secondary to acid-induced damage to the LES muscle. Animal experiments have shown that instillation of acid into the esophagus of a cat results in a decrease in LES pressure [37]. However, treating esophagitis with proton pump inhibitor does not improve LES pressure in patients with RE; the reason may be that acid-induced damage causes permanent and irreversible alteration to the contractile apparatus of the LES muscle.
Esophageal peristalsis in patients with GERD
Esophageal peristalsis plays a key role in the clearance of refluxed acid from the esophagus. Esophageal bolus clearance of acid is a two-step process of bolus clearance and acid neutralization [38, 39]. If a 15-ml, or smaller, bolus of acid is instilled into the esophagus, the majority of the acid can be cleared from the esophagus into the stomach by a peristaltic contraction of the esophagus; the remainder of the acid, lining the esophagus mucosa, is neutralized by saliva traversing the esophagus during subsequent swallow-induced peristaltic contractions. It takes seven to ten swallows, following esophageal acidification, to restore the esophageal pH to normal—between 5 and 7. Hypotensive and failed peristalsis are ineffective in clearing acid from the esophagus [40, 41].
In a recent study [42], which measured esophageal contractions at 3, 8, 13, and 18 cm above the LES in healthy subjects and patients with RE of grades A or B and grades C or D Los Angeles (LA) classification, the amplitude of the esophageal contraction at 8 and 3 cm above the LES in patients with grade C or D was significantly lower than that of healthy subjects and patients with grades A or B (Fig. 3). This study also showed that the amplitude of an esophageal contraction in patients with grade B was significantly lower than that of patients with grade A (Fig. 3). The frequency of primary peristalsis in patients with grade C or D was significantly lower than that of healthy subjects and patients with grades A or B. It is therefore suggested that bolus clearance of acid from the esophagus in patients with grade C or D is worse than that of healthy subjects and patients with grades A or B. Delayed esophageal bolus clearance of acid in patients with grade C or D is one of the causes of excessive acid esophageal exposure. The difference in the definition of the LA classification between grades A or B is the length of the mucosal break: less than 5 mm (grade A) and more than 5 mm (grade B). In this study, the sole difference between grades A or B was the mean esophageal contraction amplitude at 3 cm above the LES; therefore, a longer mucosal break may reflect the amplitude of the esophageal contraction.
Amplitude of esophageal contraction at 18, 13, 8, and 3 cm above the lower esophageal sphincter (LES) in healthy subjects (HS) and patients with reflux esophagitis (RE). RE was classified according to the Los Angeles classification. Data are presented as means ± SD. *P < 0.05; **P < 0.01. Cited from Ref. [42]
In patients with GERD, secondary peristalsis is also impaired; therefore, it is considered that dysfunction of secondary peristalsis also has an effect on excessive esophageal acid exposure [36, 43].
Whether or not esophageal peristaltic dysfunction is a primary defect or a secondary result of acid-induced esophagitis is not clear, but in animal experiments, acid injury to the esophagus can impair esophageal contractions [37]. The successful treatment of esophagitis, however, is not accompanied by an increase in low contraction amplitude.
Hiatus hernia
Hiatus hernia is seen more frequently in patients with RE than in those without [44–48], and several studies have shown a correlation between hiatus hernia and severity of RE [49–51]. Furthermore, it has been reported that esophageal acid exposure is higher in those with RE than in those without; therefore, these findings suggest that presence of hiatus hernia can contribute to excessive esophageal acid exposure. As mentioned above, whether or not the frequency of transient LES relaxations increases in patients with hiatus hernia is still not clear. In a study looking at spontaneous acid reflux episodes in patients with hiatus hernia who also had GERD it was reported that an increased number of acid reflux episodes were associated with low LES pressure, swallow-associated normal LES relaxations, and straining during periods of low LES pressure [6], which suggests that low LES pressure contributes to acid reflux episodes in patients with hiatus hernia who also have GERD. It is evident that basal LES pressure is reduced when hiatus hernia develops because the LES is displaced from the diaphragmatic hiatus into the chest, and it has been reported that the likelihood of acid reflux occurring increases when basal LES pressure decreases and that this effect is amplified according to the increase in size of the hiatus hernia [52]. A decrease in LES pressure, however, does not necessarily cause an acid reflux episode. Even if the LES pressure is hypotensive, in order for acid reflux to occur, it is necessary for the LES to open. A physiologic study exploring the role of compliance in GERD has shown that, in patients with GERD who also have hiatus hernia, there is an increase of several parameters in the esophagogastric junction (EGJ) compliance compared with normal subjects and patients with GERD who do not have hiatus hernia: (i) the EGJ opens at lower distention pressure, (ii) the relaxed EGJ opens at distention pressure that is at or near resting intragastric pressure, and (iii) for a given distention pressure, the EGJ opens more widely by approximately 0.5 cm [53]. These alterations of the EGJ in GERD patients with hiatus hernia may cause an increase in acid reflux episodes, which is associated with low LES pressure, swallow-associated normal LES relaxation, and straining during periods of low LES pressure.
Hiatus hernia also impairs esophageal bolus clearance of acid. Concurrent pH recording and scintigraphy above the EGJ show that impaired clearance is caused by refluxate from the hernia sac during swallowing [54].
The process by which a hiatus hernia develops remains unclear, but it is possible that there is an inherent weakness of the phreno-esophageal ligament and a familial clustering of GERD, which may be related to such an inherent process [55]. On the other hand, there is also a possibility that esophagitis itself could contribute to the development of hiatus hernia by inducing esophageal shortening through acid-induced contraction of the longitudinal muscles [56].
References
Dent J, Holloway RH, Toouli J, Dodds WJ. Mechanisms of lower oesophageal sphincter incompetence in patients with symptomatic gastroesophageal reflux. Gut. 1988;29:1020–8.
Holloway RH, Kocyan P, Dent J. Provocation of transient lower esophageal sphincter relaxations by meals in patients with symptomatic gastroesophageal reflux. Dig Dis Sci. 1991;36:1034–9.
Dodds WJ, Kahrilas PJ, Dent J, Hogan WJ, Kern MK, Arndorfer RC. Analysis of spontaneous gastroesophageal reflux and esophageal acid clearance in patients with reflux esophagitis. J Gastrointest Motil. 1990;2:79–89.
Iwakiri K, Hayashi Y, Kotoyori M, Tanaka Y, Kawakami A, Sakamoto C, et al. Transient lower esophageal sphincter relaxations (TLESRs) are major mechanism of gastroesophageal reflux but are not the cause of reflux disease. Dig Dis Sci. 2005;50:1072–7.
Iwakiri K, Kawami N, Sano H, Tnanaka Y, Umezawa M, Kotoyori M, et al. Mechanisms of excessive esophageal acid exposure in patients with reflux esophagitis. Dig Dis Sci. 2009;54:1686–92.
Herwaarden MAV, Samson M, Smout AJPM. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology. 2000;119:1439–46.
Dodds WJ, Dent J, Hogan WJ, Helm JF, Hauser R, Patel GK, et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med. 1982;307:1547–52.
Mittal RK, McCallum RW. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology. 1988;95:593–9.
Dent J, Dodds WJ, Friedman RH, Sekiguchi T, Hogan WJ, Arndorfer RC, et al. Mechanism of gastroesophageal reflux in recumbent asymptomatic human subjects. J Clin Invest. 1980;65:256–67.
Iwakiri K, Tanaka Y, Hayashi N, Kotoyori M, Kawami N, Kawakami A, et al. Association between reflux esophagitis and/or hiatus hernia and gastric mucosal atrophy level in Japan. J Gastroenterol Hepatol. 2007;22:2212–6.
Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol. 2009;44:518–34.
Wyman JB, Dent J, Heddle R, Dodds WJ, Tooull J, Downton J. Control of belching by the lower oesophageal sphincters. Gut. 1990;31:639–46.
Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent J. Transient lower esophageal sphincter relaxation. Gastroenterology. 1995;109:601–10.
Mittal RK, Fisher MJ. Electrical and mechanical inhibition of the crural diaphragm during transient relaxation of the lower esophageal sphincter. Gatroenterology. 1990;99:1265–8.
Mittal RK, Chiarell C, Liu J, Shaker R. Characteristics of lower esophageal sphincter relaxation induced by pharyngeal stimulation with minute amounts of water. Gastroenterology. 1996;111:378–84.
Holloway RK, Hongo M, Berger K, McCallum RW. Gastric distention: a mechanism for postprandial gastroesophageal reflux. Gastroenterology. 1985;89:779–84.
Penagini R, Bartesaghi B, Conte D, Bianchi PA. Rate of transient lower oesophageal sphincter relaxations of healthy humans after eating a mixed nutrient meal: time course and comparison with fasting. Eur J Gastroenterol Hepatol. 1992;4:35–8.
Franzi SJ, Martin CJ, Cox MR, Dent J. Response of canine lower esophageal sphincter to gastric distension. Am J Physiol. 1990;259:G380–5.
Holloway RH, Lyrenas E, Ireland A, Dent J. Effect of intraduodenal fat on lower oesophageal sphincter function and gastroesophageal reflux. Gut. 1997;40:449–53.
Penagini R, Mangano M, Bianchi PA. Effect of increasing the fat content but not the energy load of a meal on gastro-oesophageal reflux and lower oesophageal sphincter motor function. Gut. 1998;42:330–3.
Kahrilas PJ, Shi G, Manka M, Joehl RJ. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gastroenterology. 2000;118:688–95.
Freidin N, Mittal RK, McCallum RW. Does body posture affect the incidence and mechanism of gastro-oesophageal reflux? Gut. 1991;32:133–6.
Freidin N, Fisher MJ, Taylor W, Boyd D, Surratt P, McCallum RW, et al. Sleep and nocturnal acid reflux in normal subjects and patients with reflux oesophagitis. Gut. 1991;32:1275–9.
Penagini R, Bartesaghi B, Bianchi PA. Effect of cold stress on postprandial lower esophageal sphincter competence and gastroesophageal reflux in healthy subjects. Dig Dis Sci. 1992;37:1200–5.
Cox MR, Martin CJ, Dent J, Westmore M. Effect of general anaesthesia on transient lower oesophageal sphincter relaxations in the dog. Aust NZ J Surg. 1988;58:825–30.
Trudgill NJ, Riley SA. Transient lower esophageal sphincter relaxations are no more frequent in patients with gastroesophageal reflux disease than in asymptomatic volunteers. Am J Gastroenterol. 2001;96:2569–74.
Wong WM, Lai KC, Hui WM, Hu WH, Huang JQ, Wong NY, et al. Pathophysiology of gastroesophageal reflux diseases in Chinese-role of transient lower esophageal relaxation and esophageal motor dysfunction. Am J Gastroenterol. 2004;99:2088–93.
Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J. Composition of the postprandial refluxate in patients with gastroesophageal disease. Am J Gastroenterol. 2001;96:647–55.
Hayashi Y, Iwakiri K, Kotoyori M, Sakamoto C. Mechanisms of acid gastroesophageal reflux in the Japanese population. Dig Dis Sci. 2008;53:1–6.
Sifrim D, Holloway RH. Transient lower esophageal sphincter relaxations: How many or how harmful? Am J Gastroenterol. 2001;96:2529–32.
Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ. Obesity is associated with increased transient lower esophageal sphincter relaxation. Gastroenterology. 2007;132:883–9.
Asaka M, Kimura T, Kudo M, Takeda H, Mitani S, Miyazaki T, et al. Relationship of Helicobacter pylori to serum pepsinogens in an asymptomatic Japanese population. Gastroenterology. 1992;102:760–6.
Kinoshita Y, Kawanami C, Kishi K, Nakata H, Seino Y, Chiba T. Helicobacter pylori independent chronological change in gastric acid secretion in the Japanese. Gut. 1997;41:452–8.
Feldman M, Cryer B, McArthur KE, Huet BA, Lee E. Effects of aging and gastritis on gastric acid and pepsin secretion in humans: a prospective study. Gastroenterology. 1996;110:1043–52.
Sifrim D, Tack J, Zhang X, Huysmans W, Janssens J. Continuous monitoring of esophageal shortening in man during swallowing, transient LES relaxations and intraesophageal acid perfusion. Gastroenterology. 2002;122:A-188.
Iwakiri K, Hayashi Y, Kotoyori M, Tanaka Y, Kawami N, Sano H, et al. Defective triggering of secondary peristalsis in patients with non-erosive reflux disease. J Gastroenterol Hepatol. 2007;22:2208–11.
Eastwood GL, Castell DO, Higgs RH. Experimental esophagitis in cats impairs lower esophageal sphincter pressure. Gastroenterology. 1975;69:146–53.
Helm JF, Dodds WJ, Riedel DR, Teeter BC, Hogan WJ, Arndorfer RC. Determinants of esophageal acid clearance in normal subjects. Gastroenterology. 1983;85:607–12.
Helm JF, Dodds WJ, Pelc LR, Palmer DW, Hogan WJ, Teeter BC. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med. 1984;310:284–8.
Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A. Esophageal peristaltic dysfunction in peptic esophagistis. Gastroenterology. 1986;91:897–904.
Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988;94:73–80.
Sugiura T, Iwakiri K, Kotoyori M, Kobayashi M. Relationship between severity of reflux esophagitis according to the Los Angeles classification and esophageal motility. J Gastroenterol. 2001;36:226–30.
Holloway RH, Penagini R, Schoeman MN, Dent J. Effect of cisapride on secondary peristalsis in patients with gastroesophageal reflux disease. Am J Gastroenterol. 1999;94:799–803.
Wright RA, Hurwitz AL. Relationship of hiatal hernia to endoscopically proved reflux esophagitis. Dig Dis Sci. 1979;24:311–3.
Berstad A, Weberg R, Frøvshov LI, Hoel B, Hauser-Jensen M. Relationship of hiatus hernia to reflux oesophagitis. A prospective study of coincidence, using endoscopy. Scand J Gastroenterol. 1986;21:55–8.
Sontag SJ, Schnell TG, Miller TQ, Nemchausky S, Serlovsky R, O’Connell S, et al. The importance of hiatal hernia in reflux esophagitis compared with lower esophageal sphincter pressure or smoking. J Clin Gastroenterol. 1991;13:628–43.
Zhu H, Pace F, Trape E, Sangaletti O, Porro GB. Prevalence of hiatal hernia and its influence on gastro-oesophageal reflux. Eur J Gastroenterol Hepatol. 1994;6:393–8.
Ott DJ, Gelfand DW, Chen YM, Wu WC, Munitz HA. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10:317–20.
Ott DJ, Glauser SJ, Ledbetter MS, Chen MY, Koufman JA, Gelfand DW. Association of hiatal hernia and gastroesophageal reflux: correlation between presence and size of hiatal hernia and 24-hour pH monitoring of the esophagus. AJR Am Roentgenol. 1995;165:557–9.
Patti MG, Goldberg HI, Arcerito M, Bortolasl L, Tong J, Way LW. Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg. 1996;171:182–6.
Cameron AJ. Barrett’s esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol. 1999;94:2054–9.
Sloan S, Rademaker AW, Kahrilas PJ. Determinants of gastroesophageal junction incompetence: hiatal hernia, lower esophageal sphincter, or both? Ann Intern Med. 1992;117:977–82.
Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology. 2003;125:1018–24.
Mittal RK, Lange RC, McCallum RW. Identification and mechanism of delayed esophageal acid clearance in subjects with hiatus hernia. Gastroenterology. 1987;92:130–5.
Trudgill NJ, Kapur KC, Riley SA. Familial clustering of reflux symptoms. Am J Gastroenterol. 1999;94:1172–8.
Paterson WG, Kolyn DM. Esophageal shortening induced by short-term intraluminal acid perfusion in opossum: a cause for hiatus hernia? Gastroenterolgy. 1994;107:1736–40.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwakiri, K. The role of excessive esophageal acid exposure in patients with gastroesophageal reflux disease. Clin J Gastroenterol 2, 371–379 (2009). https://doi.org/10.1007/s12328-009-0125-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-009-0125-5