Abstract
Introduction
Chronic periodontitis is a common disorder in adults causing periodontal destruction and loss of teeth. These clinical presentations may lead to temporomandibular joint disorders (TMDs). This study aimed to examine the anatomic structures of the temporomandibular joints (TMJs) using cone-beam computed tomography (CBCT) in patients with chronic periodontitis.
Methods
Fifty patients with chronic periodontitis were enrolled in the study. Based on the severity of chronic periodontitis, these patients were divided into the mild, moderate, and severe groups. CBCT images of TMJs were acquired and reconstructed. Several indices on the reconstructed CBCT images were collected and analyzed, such as the oblique joint space parallel to the long axis of the condyle, the long axis diameter of the condyle, the vertical angle of the condyle, the inclination of the articular eminence vertical to the long axis of condyle at the oblique and sagittal positions, the depth of the fossa, and the horizontal angle of the cross-sections. The measurements between right and left sides of each patient were compared. Statistical analysis (paired samples t test) was performed.
Results
The differences of the joint space vertical to the bilateral condyles were statistically significant (P < 0.05). Additionally, in the severe periodontitis group, the distances between the inner and outer poles of the condyles were statistically different (P < 0.05).
Conclusion
In patients with chronic periodontitis, TMJ space vertical to the condyles and the distances between the outer and inner poles of the condyle may change over time. These two indices can potentially be used as indicators for diagnosis and further comparative analyses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Chronic periodontitis is associated with alterations of TMJ structures. |
TMJs examination of patients with chronic periodontitis has clinical significance. |
TMJs, the masticatory muscles, and periodontium are closely interconnected. |
Digital Features
This article is published with digital features to facilitate understanding of the article. You can access the digital features on the article’s associated Figshare page. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12957926.
Introduction
Periodontal diseases, broadly categorized as gingivitis and periodontitis, are an inflammatory disorder of the periodontium (i.e., the gingiva, periodontal ligament, and alveolar bone) [1]. Chronic periodontitis is the most common periodontal disease caused by multiple etiologies or predisposing factors, such as subgingival dental plaques, inflammatory cytokines, genetics, and anatomic structures [1]. Clinically, chronic periodontitis is characterized by erythema and/or bleeding of the gingiva, increased periodontal pockets, attachment loss, alveolar bone loss, and tooth mobility/drifting [2]. Alveolar bone destruction due to severe periodontitis remains the primary cause of tooth loss in adults [2, 3]. The oromaxillofacial complex consists of many anatomic structures (e.g., the masseter muscle, tongue, temporomandibular joint [TMJ], mandible, teeth, periodontium, and nerves and vessels) that precisely coordinate the entire masticatory sequence [4]. Periodontal destruction and tooth loss may eventually lead to a series of adverse events in the oromaxillofacial region, such as TMJ disorders (TMDs) [5]. Studies have shown an association between tooth loss and TMJ malfunction [6, 7]. However, changes in the structures of TMJs are still unclear in patients with chronic periodontitis.
Multiple imaging modalities, such as cone-beam computed tomography (CBCT) and magnetic resonance imaging (MRI), are available for TMJ examinations and diagnoses [8]. MRI does not involve radiation or any invasive procedures. Moreover, MRI can display extremely clear soft-tissue images, though at a higher cost [8]. CBCT, on the other hand, allows precise 3D image superimposition with a low radiation dosage. The reconstructed CBCT images allow accurate and reliable linear measurements of bone structures and are hence particularly useful for assessing craniofacial structures, such as the TMJ and mandible [9]. Due to improved imaging accuracy and a significantly lower cost than conventional CT and MRI, CBCT is widely used in dental treatment planning and diagnosis [8, 9]. In this study, we aimed to investigate the differences of bilateral TMJs in patients with chronic periodontitis using CBCT. The information may shed light on how chronic periodontitis influences TMJ structures.
Methods
Patient Selection
Patients who were seen and diagnosed with chronic periodontitis in the Stomatological Hospital of Ningxia Medical University between January 2016 and December 2017 were screened. We excluded individuals with a past medical history of rheumatoid arthritis, TMJ trauma, and TMDs as well as those who were not compliant with the research protocol. Sample size was determined by N = Z2 × (P × (1 − P))/E2, Z = 1.64 when the confidence level was 90%, with 5% margins of error (E), and P = 0.05. The minimal number of enrolled patients required was 52. Fifty patients (22 males and 28 females) were selected and enrolled in the current study. The study protocol was approved by the Ethics Committee of the Fourth Medical Center, Chinese PLA General Hospital. Written informed consent was obtained from all the study subjects before enrollment. This study was conducted in accordance with the Declaration of Helsinki 1964 and its later amendments.
The severity of chronic periodontitis is based on the amount of clinical attachment loss (CAL) and alveolar bone destruction and is further designated as mild, moderate, and severe. In our research protocol, we defined (1) mild chronic periodontitis as gingivitis and bleeding on probing, periodontal pocket ≤ 4 mm, and alveolar bone destruction < 1/3 of the root on the radiograph (1–2 mm CAL); (2) moderate chronic periodontitis as gingivitis and bleeding on probing, periodontal pocket > 4 mm and ≤ 6 mm, and alveolar bone destruction ≥ 1/3 but < 1/2 of the root on the radiograph (3–4 mm CAL); (3) severe chronic periodontitis as prominent gingivitis, periodontal pocket > 6 mm, and alveolar bone destruction ≥ 1/2 of the root on the radiograph (≥ 5 mm CAL) [10, 11].
CBCT
The bone structures of the TMJs were scanned using CBCT (NewTom VGi, Imola, Italy). Patients were positioned, and images were taken under the large field with the setting of 110 kV, 8.36 mA, exposure time 5.4 s, and resolution 0.15 mm. The images were then reconstructed and measured using the NewTom image processing software. The images of the condyles were positioned in the center, and the interface was locked after adjusting the horizontal line to be parallel to the sigmoid notch. The major anatomic landmarks of TMJs were marked for the following 3D reconstruction. Multiple indices of bilateral TMJs were measured, including cross-sections, sagittal-sections, oblique position paralleled to the long axis of condyles, and the curve surfaces of oblique position vertical to the long axis of the condyles.
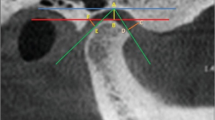
Axial measurement (Fig. 1): one section exhibiting the largest surface areas of bilateral condyles was selected. Draw sagittal line a along the nasal septum and foramen magnum and then draw line b perpendicular to line a through the center of the condyles. Draw line c parallel to the long axes of bilateral condyles. The angle between lines b and c is angle α.
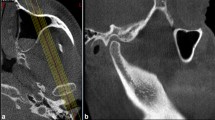
Sagittal measurement (Fig. 2): draw line a along the center of the external acoustic foramen and the anterior articular tubercle of the TMJ fossa and then draw line b perpendicular to line a through the center of condyle. The measurements between each line (at 30°, 60°, 90°, 120°, and 150°) and joint space were recorded. The depth of the TMJ fossa, sagittal inclination of articular eminence (α), and the distance between the inner and outer poles of the condyles are also measured.
Horizontal measurement (Fig. 3): draw a horizontal base line between the top of the bilateral TMJ fossae and then move the horizontal base line downward to the center of the condyles as line a. Draw line b perpendicular to line a through the center of the bilateral condyles. The measurements between each line (at 60°, 90°, and 120°) and joint space were recorded. The vertical inclination of articular eminence is also measured.
Statistical Analysis
All measurements were completed by clinical researchers in the Department of Oral Radiology at Ningxia Medical University Hospital. Each measurement was made three times independently, and a mean value was calculated and recorded as x ± s. Statistical analyses were performed by SPSS19.0 software. The measurements between the right and left sides of each patient were compared using paired samples t-test, and the data were statistically significant at P < 0.05.
Results
The cohort included 50 patients consisting of 22 males and 28 females with age ranging between 18 and 83 years with a mean age of 40.8 years. Ten patients had mild chronic periodontitis, 11 had moderate chronic periodontitis, and 29 had severe chronic periodontitis. The measurements between bilateral TMJs were compared using paired samples t test.
According to our analysis, the measurements of the sagittal 90° joint space demonstrated a statistical significance in the entire patient cohort (P < 0.05) (Table 1). In the severe chronic periodontitis group, the distance between the inner and outer poles of the condyles was statistically significantly different (P < 0.05) (Table 2). The measurements in the mild and moderate chronic periodontitis groups did not show any statistically significant differences (Tables 3 and 4).
Discussion
Periodontal disease is a prevalent inflammatory disorder that affects > 90% of adults worldwide [3]. Chronic periodontitis is the most common periodontal disease induced by dental plaques at the tooth-gingival junction. The inflammation then extends to the subgingival tissues and destroys the gingiva, alveolar bone, periodontal ligament, and cementum. Clinically, chronic periodontitis may present as gingivitis, alveolar bone loss, and tooth mobility/drifting. Chronic periodontitis impacts both oral and systemic health and causes significant healthcare and socioeconomic burdens [3].
The oromaxillofacial complex consists of the teeth, periodontium, tongue, masticatory muscles, and temporomandibular joints (TMJs). These vital structures collectively play an essential role in many physiologic functions, such as chewing, swallowing, and speaking. It has been shown that the well-being of the periodontium and TMJs both intertwine many aspects of occlusion and mastication [12]. When chronic periodontitis progresses, inflammation-induced discomfort may prompt patients to perform unilateral mastication, which causes an abnormal occlusal relationship or even occlusal trauma [13]. Occlusal trauma and malocclusion affect TMJ functions, leading to back-shift of the condyle, midline deviation, and TMDs [13]. Patients with TMDs may exhibit symptoms such as limited mouth opening, joint pain or clicking, unilateral myofascial pain, and structural alterations of TMJs [12, 14].
However, it is still unclear how chronic periodontitis contributes to the occurrence of TMDs. In the present study, we investigated the effects of periodontal inflammation on structural changes of TMJs using CBCT. This imaging modality was introduced in Europe in the late 1990s and is now widely utilized in oromaxillofacial diagnosis and dental treatment planning [15]. CBCT allows for accurate image reconstruction and 3D visualization. It has been shown in the literature that CBCT serves as a reliable imaging reference in oromaxillofacial examinations, in particular, TMJs [9]. With 3D images, it is feasible to directly monitor the relationship between the condyle and mandibular fossa and precisely measure the anatomic landmarks of TMJs from sagittal, coronal, and axial views.
In this cohort, 50 patients with chronic periodontitis were enrolled in the study. Multiple indices of the anatomic structures of TMJs were measured using the reconstructed CBCT images. Paired samples t test was performed to evaluate the differences between bilateral TMJs in each patient. According to our data, only the measurements of joint space 90° to the sagittal view exhibited a statistical significance in the entire cohort (P < 0.05). The results indicated that in patients with chronic periodontitis, the superior joint space of TMJs was asymmetric bilaterally. The abnormal joint space 90° to the sagittal view might be a consequence of chronic periodontitis. Multiple factors contribute to the asymmetrical positioning of condyles in the mandibular fossa, such as imbalanced occlusion, teeth drifting, unilateral or bilateral posterior teeth loss, and posterior shift of the condyles. When the patient cohort was subdivided into different groups based on the severity of chronic periodontitis (i.e., mild, moderate, and severe groups), we only detected meaningful differences between the inner and outer poles of the condyles in the severe group. The occlusal imbalance from severe chronic periodontitis altered the relationships among all the compartments of the TMJs and created abnormal forces pressing or stretching the soft tissues in the area. The occlusal imbalance may cause additional stress on the lateral pterygoid muscle and dislocate the joint discs, leading to abnormal and asymmetric positioning of the condyles. In the moderate and mild groups, this altered positioning was not statistically evident. Our finding suggested that not all chronic periodontitis leads to malocclusion or TMDs. The TMJs are constantly remodeling and adapting to the occlusion changes and should be able to functionally adapt to the new occlusal relationship within a certain range. Once the alteration is beyond physiologic tolerance, TMDs may occur [5, 14].
In summary, our results revealed that chronic periodontitis is associated with alterations of TMJ structures that may eventually lead to insufficient compensatory effects of the TMJs. The TMJs, masticatory muscles, and periodontium are closely interconnected and influence occlusion and mastication collectively. As a pilot study, we suggest controlling periodontal inflammation and reducing alveolar bone loss and tooth shifting/drifting to avoid TMDs. It may be clinically beneficial to examine the TMJs in patients with chronic periodontitis. Due to the small sample size, we were not able to further explore the correlation between symptoms (e.g., the number and location of tooth loss, duration of edentulism, and presence of pain) and the alterations of TMJ structures. Furthermore, long-term follow-up will provide additional information to elucidate the occurrence and resolution of TMDs.
Conclusion
Based on our pilot study, in patients with chronic periodontitis, the TMJ space vertical to the condyles and the distances between the outer and inner poles of the condyle may change over time. These two indices can potentially be used as indicators for diagnosis and further comparative analyses.
References
Williams RC. Periodontal disease. N Engl J Med. 1990;322(6):373–82.
Van der Velden U, Abbas F, Armand S, et al. Java project on periodontal diseases. The natural development of periodontitis: risk factors, risk predictors and risk determinants. J Clin Periodontol. 2006;33(8):540–8.
Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis. 2016;22(7):609–19.
Hori K, Ono T, Nokubi T. Coordination of tongue pressure and jaw movement in mastication. J Dent Res. 2006;85(2):187–91.
Lamster IB, Asadourian L, Del Carmen T, Friedman PK. The aging mouth: differentiating normal aging from disease. Periodontol 2000. 2016;72(1):96–107.
Kirveskari P, Alanen P. Association between tooth loss and TMJ dysfunction. J Oral Rehabil. 1985;12(3):189–94.
Garib BT, Qaradaxi SS. Temporomandibular joint problems and periodontal condition in rheumatoid arthritis patients in relation to their rheumatologic status. J Oral Maxillofac Surg. 2011;69(12):2971–8.
Al-Saleh MA, Alsufyani NA, Saltaji H, Jaremko JL, Major PW. MRI and CBCT image registration of temporomandibular joint: a systematic review. J Otolaryngol Head Neck Surg. 2016;45(1):30.
Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44(1):20140235.
Wiebe CB, Putnins EE. The periodontal disease classification system of the American Academy of Periodontology—an update. J Can Dent Assoc. 2000;66(11):594–7.
Chatzistavrianou D, Blair F. Diagnosis and management of chronic and aggressive periodontitis part 1: periodontal assessment and diagnosis. Dent Update. 2017;44(4):306–8.
Steinhardt G. The reciprocal dependence of the periodontium and temporomandibular joint in mastication. Dtsch Zahnarztl Z. 1950;5(21):1157–73.
Kroese JM, Volgenant CMC, van Schaardenburg D, Loos BG, Crielaard W, Lobbezoo F. Temporomandibular joint function, periodontal health, and oral microbiome in early rheumatoid arthritis and at-risk individuals: a prospective cohort study protocol. BDJ Open. 2020;6:7.
Jeon HM, Ahn YW, Jeong SH, et al. Pattern analysis of patients with temporomandibular disorders resulting from unilateral mastication due to chronic periodontitis. J Periodontal Implant Sci. 2017;47(4):211–8.
Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8(9):1558–644.
Acknowledgements
Funding
This research and the journal’s rapid service fee were supported by University-level Fund of Ningxia Medical University of China (no. XM2016086), Capital Clinical Application Research and Results Promotion Project (no. Z171100001017154), General Hospital Transformation Project (2017TM-030), General Hospital Clinical Research Supporting Fund (2018FC-304M-TSYS-05), and the Natural Science Foundation of Ningxia (2020AAC03355).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Xiaoqian Guo, Ziyan Guo, Changyi Yang, Jingjiao Wang, Min Zhao, Yanfeng Li, and Li Wang have nothing to disclose.
Compliance with Ethics Guidelines
The study protocol was approved by the Ethics Committee of the Fourth Medical Center, Chinese PLA General Hospital. Written informed consent was obtained from all the study subjects before enrollment. The study was conducted in accordance with the Declaration of Helsinki 1964 and its later amendments.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12957926.
Rights and permissions
About this article
Cite this article
Guo, X., Yang, C., Wang, J. et al. Comparative Analysis of the Temporomandibular Joints in Patients with Chronic Periodontitis Using Cone-Beam Computed Tomography (CBCT). Adv Ther 38, 541–549 (2021). https://doi.org/10.1007/s12325-020-01508-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01508-6