Abstract
Introduction
Recent approval of novel agents has changed the treatment landscape for post menopausal women with hormone receptor-positive (HR+) and human epidermal growth factor receptor-2 negative (HER2−) metastatic breast cancer (mBC). The objective of this study was to describe contemporary treatment patterns among postmenopausal women with HR+/HER2− mBC in the real-world setting.
Methods
Data were collected from 64 community oncologists in the US between February and June 2017 using an online medical records extraction tool. Physicians reviewed medical records and provided information on patient demographics and disease characteristics, and treatment regimens. Treatment patterns were described overall and separately by line of therapy and type of treatment received. Discontinuation rates were estimated using Kaplan–Meier analyses to account for censoring.
Results
Data were collected on 401 patients. Mean age at the time of mBC diagnosis was 67 years. In the first-line setting, 52.4% of patients received a cyclin-dependent kinase 4/6 (CDK4/6) inhibitor-based regimen, most commonly with an aromatase inhibitor (AI) (39.2%) or fulvestrant (10.0%); 30.2% received endocrine therapy, most commonly an AI (21.4%) or fulvestrant (5.2%) in monotherapy, while 12.7% received a chemotherapy-based regimen. In the second-line setting, 42.9% of patients received a CDK4/6 inhibitor-based regimen, 18.4% received endocrine therapy, and 22.4% received a chemotherapy-based regimen. The 18-month discontinuation rate was 34.5% for patients receiving a CDK4/6 inhibitor-based regimen and 45.8% for patients receiving endocrine monotherapy.
Conclusion
CDK4/6 inhibitor-based regimens were the most commonly prescribed treatment in both first- and second-line settings. A wide variety of treatment sequences were observed which suggests an absence of a standard of care for postmenopausal women with HR+/HER2− mBC in real-world practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is a leading cause of cancer-related deaths among women [1]. In 2017, an estimated 252,710 new cases of invasive BC were expected to be diagnosed in women in the United States (US) [1]. Although as many as 90% of women with early stage localized BC achieve long-term disease-free survival, women diagnosed with metastatic BC (mBC) have substantially lower survival rates [1, 2].
Although often referred to as a single disease, mBC has distinct histological and molecular subtypes that differ in terms of risk factors, response to treatments and outcomes. Hormone receptor-positive (HR+) and human epidermal growth factor receptor-2-negative (HER2−) are the most common histological subtypes diagnosed in approximately 70% of patients, and account for most of the deaths from the disease [3]. Other important prognostic factors include age and menopausal status which impact disease characteristics and outcomes, as well as choice of treatment [4].
Endocrine therapy has long been the recommended first-line treatment for HR+/HER2− mBC. Following disease progression, patients may receive an alternative single-agent endocrine therapy followed by chemotherapy. Chemotherapy is typically recommended when there is clear evidence of resistance to endocrine therapy or when there is a need for rapid disease control [4].
Recently, novel agents, notably cyclin-dependent kinase 4/6 (CDK4/6) inhibitors, have changed the treatment landscape of the disease [5]. CDK4/6 inhibitor therapies have shown improved progression-free survival compared to endocrine therapy alone. Palbociclib was the first CDK4/6 inhibitor to be approved by the Food and Drug Administration (FDA) in the US, in February 2015, for use in combination with letrozole as first-line treatment for advanced HR+/HER2− BC in postmenopausal women [6, 7]. It was later approved in combination with fulvestrant for use in second or further lines of therapy for women with HR+/HER2− advanced or mBC who relapsed or progressed during prior endocrine therapy [8]. In 2017, two new CDK4/6 inhibitors, ribociclib and abemaciclib, were also approved for the treatment of postmenopausal women with HR+/HER2− advanced or mBC [9, 10]. The updated 2017 National Comprehensive Cancer Network (NCCN) guidelines include recommendations for palbociclib or ribociclib, in combination with an aromatase inhibitor (AI), as first-line treatment options for postmenopausal women with recurrent or stage IV HR+/HER2− BC. In addition, abemaciclib (alone or with fulvestrant) is recommended as a second-line therapy for these patients [4].
Given the changing landscape of treatments for HR+/HER2− mBC among postmenopausal women, it is important to understand the treatments used in current clinical practice and the drivers of different treatment choices. The objective of this study was to describe contemporary treatment patterns in US clinical practice for postmenopausal women with HR+/HER2− mBC.
Methods
Data Source
This observational, retrospective study was based on data collected from community oncologists using an online survey and patient medical chart review. Oncologists in the US were invited by email to participate in the study. Participating oncologists were asked to provide clinical information on a maximum of 10 patients from their practice. The data collection period spanned February to June 2017, and was conducted using an online medical record extraction tool that was developed for this study. Data collected from physicians did not include any patient-identifying information and the study was exempted from full review by the New England Institutional Review Board. This study is based on retrospective data and does not include any interaction with human participants or animals performed by any of the authors.
Study Sample
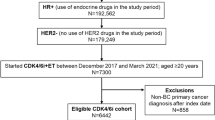
Patients were eligible if they: (1) were women diagnosed with HR+ and HER2− or HER2-equivocal de novo or recurrent mBC between March 2015 and January 2016 (allowing for a potential follow-up of 12 months); (2) were postmenopausal at the time of initiation of first-line therapy for HR+/HER2− mBC; (3) had never been enrolled in a clinical trial for the treatment of BC; and (4) had complete medical and treatment-related information from the date of HR+/HER2− mBC diagnosis available to the participating physician.
Data Collection and Study Measures
Physicians provided information on their practice, including size, setting, location, specialty, and treatment preferences. For each selected patient, physicians reviewed medical records and provided detailed information on patient demographics, BC history (e.g., diagnosis date, tumor stage at diagnosis), comorbidities, and treatment patterns, including information on first- and second-lines of therapy for mBC such as treatment regimens, treatment changes, and reasons for treatment changes.
Physician characteristics and treatment preferences were summarized. Patient treatment patterns and treatment sequences were also described for all patients. After exploring reported treatment patterns, patients were categorized into four groups based on the first-line treatment received: (1) CDK4/6 inhibitor-based regimen (only palbociclib was approved at the time of the data collection), (2) endocrine monotherapy, (3) chemotherapy-based regimen, or (4) other treatment regimen. Patient characteristics were summarized overall and separately by treatment group. Discontinuation rates were estimated using Kaplan–Meier analyses to account for censoring of patients who were still on treatment at the time of the data collection.
Results
Physician Characteristics
A total of 64 US oncologists participated in the study. Nearly all physicians (95.3%) worked at community-based practices with most practice sizes of 2–9 oncologists/subspecialists (54.7%) or 10 or more oncologists/subspecialists (40.6%). All four US census regions were represented, with the majority of practices in a suburban (45.3%) or urban (42.2%) setting. Almost all physicians (90.6%) reported having practiced oncology for more than 10 years.
Table 1 describes the treatment preferences for first-line therapy for mBC of the responding physicians in their current practice. The majority (67.2%) of physicians ranked CDK4/6 inhibitors + endocrine therapy as their top treatment option in their current practice, citing good efficacy profile (93.0%) and good tolerability profile (60.5%) as reasons for this treatment choice. Endocrine monotherapy was the preferred first-line treatment option for mBC for 26.6% of physicians who cited good tolerability profile (100%), good efficacy profile (88.2%), and their familiarity with this regimen (52.9%) as reasons for this treatment choice. Chemotherapy as monotherapy was preferred by 6.3% of physicians with the majority (75%) citing good efficacy profile as the main reason for choosing this treatment option as a first-line therapy for treatment of mBC (Table 1).
Patient Characteristics
A total of 401 women met the inclusion criteria and were included in the analyses. The average age of patients at the time of mBC diagnosis was 67 years; patients receiving endocrine monotherapy were older (71.6 years). The majority of patients were Caucasian (70.6%) and 55.1% had Medicare, while 41.1% were covered by commercial or private insurance. Patients who received endocrine monotherapy in the first-line were more likely to be Medicare-insured (65.3%)—which is highly correlated with age, while those receiving chemotherapy were more likely to be covered by commercial or private insurance (62.7%). Prior to first-line therapy, the majority of patients (80.8%) had Karnofsky performance status (KPS) ≥ 70%. Patients who used endocrine monotherapy in the first-line tended to have poorer KPS scores, with 14.9% reporting KPS ≤ 50%. The most common sites of metastases at first-line initiation were bone (72.8%; 40.4% of patients had bone-only metastases), followed by lungs (39.2%) and lymph nodes (28.7%). Patients receiving endocrine monotherapy were most likely to have bone-only metastases (56.2%), while patients receiving chemotherapy or other regimens were most likely to have metastases in visceral organs (68.6% and 73.7%, respectively) (Table 2).
Treatment Characteristics
In first-line therapy, 52.4% of the patients received a CDK4/6-based regimen, most commonly with an AI (39.2%) or fulvestrant (10.0%), 30.2% received endocrine therapy, most commonly an AI (21.4%) or fulvestrant (5.2%) in monotherapy, while 12.7% received a chemotherapy-based regimen. In second-line therapy, 42.9% of patients received a CDK4/6 inhibitor-based regimen, 18.4% received endocrine therapy, 22.4% received a chemotherapy-based regimen, and 16.3% received other treatment regimens (everolimus + endocrine therapy). The most common regimens were palbociclib with fulvestrant (23.1%) or with an AI (17.7%) (Table 3).
Among the 147 patients with at least two lines of therapy, the most common treatment sequences observed were an AI followed by CDK4/6 inhibitor with fulvestrant (13.6%), chemotherapy followed by CDK4/6 inhibitor with an AI (10.3%), and CDK4/6 inhibitor with an AI, followed by chemotherapy (8.8%) or by everolimus with an AI (8.8%) (Table 4).
Slightly over half of all patients (53.1%) were still receiving first-line therapy at the time of data collection, 65.7% of patients were receiving a CDK4/6 inhibitor-based regimen, 53.7% were receiving endocrine monotherapy, and 5.9% were receiving chemotherapy. Overall, the median time to discontinuation for first-line therapy was 19.4 months. Among patients using endocrine monotherapy in the first line, the median duration was 18.7 months, while, for patients receiving chemotherapy, it was 5.6 months (consistent with 4–6 cycles of 28 days). For patients who received a CDK4/6 inhibitor in first line, median duration was not reached because the majority of patients were censored (still on treatment at the time of data collection).
The 18-month discontinuation rate for patients receiving a CDK4/6 inhibitor-based regimen was 34.5%, 45.8% for patients receiving endocrine monotherapy, and 92.9% for patients receiving chemotherapy in first-line therapy. The most common reason for discontinuing first-line therapy was disease progression or sub-optimal response, given for 72.3% of patients overall, 80.6% of patients receiving CDK4/6 inhibitors and 89.3% of patients receiving endocrine therapy. Among patients receiving chemotherapy in the first line, the majority (56.3%) discontinued because they had completed the planned duration of therapy (Table 5).
Discussion
This study evaluated real-world treatment patterns among postmenopausal women with HR+/HER2− mBC. The results showed that, in both first-line and second-line settings, CDK4/6 inhibitor-based regimens were the most commonly prescribed treatment with just over half of patients receiving CDK4/6 inhibitors, mostly with AI or fulvestrant in the first line. However, endocrine therapy and chemotherapy were also used for a considerable proportion of patients as first-line therapies.
Several clinical trials have demonstrated the effectiveness of CDK4/6 inhibitors in the treatment of postmenopausal women with HR+/HER2− mBC. These studies have shown significantly longer progression-free survival in patients treated with CDK4/6 inhibitors compared to those treated with endocrine therapy alone [11,12,13]. However, despite improved outcomes demonstrated for patients using CDK4/6 inhibitor therapies, 30% of patients in the present study were observed to receive endocrine monotherapy and 13% chemotherapy-based regimens in the first line for HR+/HER2− mBC; however, the results of the physician survey indicated that treatment patterns may already be changing. Approximately two-thirds of physicians reported CDK4/6 inhibitors to be the most commonly prescribed first-line therapy for the treatment of mBC in their current practice. The difference between the physician survey results and the patient-level data, where approximately 50% of patients were treated with CDK4/6 inhibitors in the first line, may be partly explained by the lag between the time patients started therapy (up to 2 years before the data collection) and the time physicians answered the survey. It is likely that the proportion of patients receiving CDK4/6 inhibitors will increase over time as physicians become more familiar with these agents and their benefits, particularly since two additional CDK4/6 inhibitors, ribociclib and abemaciclib, have recently been approved.
For postmenopausal women with HR +/HER2- mBC, the NCCN guidelines recommend a number of options for first-line therapy, including a CDK4/6 inhibitor—palbociclib or ribociclib—in combination with AI, or single-agent therapy with an AI, a selective estrogen receptor (ER) modulators (i.e., tamoxifen or toremifene), or a selective ER down-regulator (i.e., fulvestrant). Patients who had prior endocrine therapy within 1 year are recommended to consider a different endocrine therapy, possibly with a CDK4/6 inhibitor, or mTOR inhibitor, and those in visceral crises are recommended chemotherapy. Patients are recommended to continue first-line therapy until progression or unacceptable toxicity, at which time they may consider another line of endocrine therapy (if not endocrine refractory). Chemotherapy is only recommended for women with a need for rapid response, symptomatic visceral disease, or suspected endocrine resistance [4]. Several of the treatment regimens observed in this study were not consistent with these guideline recommendations. For example, 30% of patients received endocrine therapy, 12% received chemotherapy-based regimens in the first line, and some received palbociclib in combination with chemotherapy.
Previous studies on treatment patterns among women with HR+/HER2− mBC have also reported inconsistencies with guideline recommendations. For example, despite NCCN recommendations that endocrine therapy should be used as first-line therapy in women with HR+/HER2− mBC, a US study based on commercial health plan data from 2008 to 2013 found that more than 50% of women with HR+/HER2− mBC were treated with first-line chemotherapy [14]. In another US study based on claims data from 2002 to 2012, 40% of postmenopausal women with HR+/HER2− mBC received chemotherapy as first-line therapy; among those who used endocrine therapy in the first line, most received only one line of endocrine therapy before discontinuation or transition to chemotherapy [15]. Similarly, in a European chart review study from 2014, 30% of patients used chemotherapy in first line, a higher proportion than expected considering the HR+ tumor molecular profile and chemotherapy-related toxicities [16]. Moreover, it was reported that 22% of patients in that study would have been recommended by treatment guidelines to continue hormonal therapy for their second line of therapy, but instead received chemotherapy [16].
The present study uses more recent data that include novel CDK4/6 inhibitors as current treatment options. Results suggest considerable deviation from guideline recommendations and significant heterogeneity in the treatment of postmenopausal women with HR+/HER2− mBC. In this study, a variety of treatment sequences, including 35 different treatment regimens in the first line, were observed. Some treatment regimens, such as the combination of palbociclib with chemotherapeutic agents, may be unconventional.
The inconsistencies between guideline recommendations and real-world practice may be partly attributed to the considerable heterogeneity in metastatic disease characteristics as well as the lack of clarity in some components of guideline recommendations (e.g., definition of treatment response or disease progression) that may leave treatment options open to physicians’ interpretation. While there may be individual patient-specific reasons for these inconsistencies, the absence of a standard of care that is consistently implemented in clinical practice points to an unmet need for treatment options in this patient population.
This study has some limitations. First, although physicians were instructed to randomly select patients who met the inclusion criteria, selection bias may exist if physicians were biased towards selecting patients they had seen more recently or who had better or worse outcomes. In addition, due to the non-randomized nature of the sample, the choice of treatment could be endogenous to patient characteristics or physician preferences. Second, since patients were observed over a relatively short time period, the information on treatment duration was limited. Third, the study did not consider prior use of antineoplastic therapy in the adjuvant or neo-adjuvant setting, which may impact the treatments considered for mBC. Finally, given the relatively small number of physicians who participated in the study, the results may not be fully representative of community oncology practices in the US.
Conclusion
The treatment landscape for postmenopausal women with HR+/HER2− mBC is rapidly changing. Half of postmenopausal women with HR+/HER2− mBC were treated with CDK4/6 inhibitors in this study, a proportion that is likely to increase given the recent approval of two new CDK4/6 inhibitor agents. Further studies are needed to evaluate the uptake of these novel agents into real-world practice, as well as their outcomes in the real world.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30.
Weide R, Feiten S, Friesenhahn V, Heymanns J, Kleboth K, Thomalla J, et al. Metastatic breast cancer: prolongation of survival in routine care is restricted to hormone-receptor- and Her2-positive tumors. SpringerPlus. 2014;3:535.
American Cancer Society. Cancer facts & figures 2017. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html.
National Comprehensive Cancer Network (NCCN). Clinical practice guidelines in oncology (NCCN guidelines). Breast cancer. Version 1.2017: Fort Washington, PA. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
Shah AN, Cristofanilli M. The Growing role of CDK4/6 inhibitors in treating hormone receptor-positive advanced breast cancer. Curr Treat Options Oncol. 2017;18(1):6.
Turner NC, Ro J, Andre F, Loi S, Verma S, Iwata H, et al. Palbociclib in hormone-receptor-positive advanced breast cancer. N Engl J Med. 2015;373(3):209–19.
Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16(1):25–35.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–39.
U.S. Food and Drug Administration. Ribociclib (Kisqali) 2017. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm546438.html.
US Food and Drug Administration. FDA approves abemaciclib for HR-positive, HER2-negative breast cancer 2017. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm578081.htm.
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–36.
Goetz MP, Toi M, Campone M, Sohn J, Paluch-Shimon S, Huober J, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–46.
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Ribociclib as first-line therapy for hr-positive, advanced breast cancer. N Engl J Med. 2016;375(18):1738–48.
Burton T, Byfield SD, Smith GL, Zanotti G, Bell TJ, Perkins JJ, et al. Clinical and economic outcomes by first-line treatment among women with HR+/HER2− metastatic breast cancer in a large US health plan database. Curr Med Res Opin. 2016;32(8):1417–23.
Swallow E, Zhang J, Thomason D, Tan RD, Kageleiry A, Signorovitch J. Real-world patterns of endocrine therapy for metastatic hormone-receptor-positive (HR+)/human epidermal growth factor receptor-2-negative (HER2−) breast cancer patients in the United States: 2002-2012. Curr Med Res Opin. 2014;30(8):1537–45.
Andre F, Neven P, Marinsek N, Zhang J, Baladi JF, Degun R, et al. Disease management patterns for postmenopausal women in Europe with hormone-receptor-positive, human epidermal growth factor receptor-2 negative advanced breast cancer. Curr Med Res Opin. 2014;30(6):1007–16.
Acknowledgements
We thank the participants of the study.
Funding
Funding for this research, including the journal’s article processing charges, was provided by Novartis Pharmaceuticals Corporation.
Author contributions
The study sponsor was involved in all stages of the study research and manuscript preparation. All authors participated in the design and analytical approach of the study and contributed to the manuscript development. Results were summarized and interpreted in collaboration with all authors. Manuscript was prepared by the authors with the assistance from a professional medical writer ultimately paid by the sponsor. All authors had full access to all the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis
Medical Writing Assistance
Medical writing assistance was provided by Sara Kaffashian, an employee of Analysis Group, Inc. Analysis Group received consulting fees from Novartis for the conduct of this study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Anand A. Dalal is a current employee of Novartis Pharmaceuticals Corporation and may own stock/stock options. Tania Small is a former employee of Novartis Pharmaceuticals Corporation and may own stock/stock options. Deborah Goldschmidt is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Hela Romdhani is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Sneha Kelkar is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Annie Guerin is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Genevieve Gauthier is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Eric Q. Wu is an employee of Analysis Group Inc., which has received consultancy fees from Novartis Pharmaceuticals Corporation. Polly Niravath received honoraria from Novartis as a consultant.
Compliance with Ethics Guidelines
This study is based on retrospective data and does not include any interaction with human participants or animals performed by any of the authors.
Data Availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request. Please note that institutional review board confirmation will be needed before the data can be shared with additional parties.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to https://doi.org/10.6084/m9.figshare.5882380.
Rights and permissions
About this article
Cite this article
Goldschmidt, D., Dalal, A.A., Romdhani, H. et al. Current Treatment Patterns Among Postmenopausal Women with HR+/HER2− Metastatic Breast Cancer in US Community Oncology Practices: An Observational Study. Adv Ther 35, 482–493 (2018). https://doi.org/10.1007/s12325-018-0676-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-018-0676-2