Abstract
Introduction
The aim of this study was to investigate the clinical characteristics and practice pattern of patients with dry eye disease (DED) in eye clinics across Japan.
Methods
A multi-center, cross-sectional study was conducted among patients with DED who visited eye clinics in Japan. Subjective symptoms, patient’s background, ocular surface features, and tear function were evaluated. Main outcome measures were tear break-up time (TBUT), Schirmer I value, kerato-conjunctival staining score, and dry eye symptom questionnaire score.
Results
Initially, 463 subjects were enrolled, and 449 cases (63 male and 386 female; mean age, 62.6 ± 15.7 years) were included in the final analysis. Overall, 94.9% of patients had a shortened TBUT (≤5 s), and 54.6% had an aqueous tear deficiency (Schirmer I value ≤5 mm). The most prevalent subtype of dry eye was aqueous-deficient dry eye, which was present in 35.0% of all patients, followed by short-BUT-type dry eye, which was seen in 26.7%.
Conclusion
The two most common DED subtypes were aqueous-deficient and short-BUT-type dry eye. Shortened TBUT is the most common feature of dry eye, regardless of subtype. The current treatment choice mainly consisted of hyaluronic acid, two novel mucin secretagogues, diquafosol and rebamipide, and steroidal eye drops.
Trial Registration: University Hospital Medical Information Network: UMIN (registries no. UMIN 000015890).
Funding: Japan Dry Eye Society, Tokyo, Japan, and Santen Pharmaceutical Co., Ltd., Osaka, Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dry eye disease (DED) is a multifactorial chronic disease of the tears and ocular surface that results in symptoms including ocular discomfort, visual disturbance, and tear film instability [1, 2]. As the disease concept has matured, various conditions that compromise tear secretion, tear evaporation, or tear film stability have been included in DED. Risk factors for dry eye include female gender, aging, desiccated environment, meibomian gland dysfunction (MGD), contact lens (CL) wear, visual display terminal usage, topical or oral medications, and ocular surgery [3,4,5,6,7].
DED is recognized as a common eye disease that affects a wide range of age groups; however, the prevalence of DED varies from 0.4 to 33% according to reports [3,4,5,6,7,8,9,10]. Differences in the prevalence may result from geographic factors such as climate, country, and region [11, 12]. Evaluative methods, diagnostic criteria, and characteristics of the study population, such as age and gender, are other sources of differences. Additionally, differences between population- and clinic-based studies may also be an important source of variation.
There appears to be considerable discrepancy between subjects classified as having DED in population-based studies compared to those who seek medical care. Shimmura et al. conducted a population-based study in Japan and reported that 25% of participants with dry eye symptoms used over-the-counter eye drops daily, whereas only 11% sought professional help [8]. In the USA, when DED patients were classified into three categories according to severity level, 80% of patients with marginal DED and half of those with moderate DED were self-medicated [9]. Data from a large US-managed care database suggest that the overall prevalence of clinically treated DED is 0.4–0.5% [10]. Thus, although the prevalence of DED in a population-based study is generally high, only a limited proportion of patients with DED are receiving medical treatment. There have been, however, only a few reports on clinic-based surveys of dry eye patients [13,14,15].
Medical treatment of DED has traditionally consisted of artificial tears with or without viscous materials, hyaluronic acid, and anti-inflammatory agents. Two novel drugs, diquafosol and rebamipide, were approved for clinical use in December 2010 and in November 2011, respectively, by the Ministry of Health, Labour, and Welfare, Japan. Both agents are classified as mucin secretagogues and have become an important modality for the treatment of dry eye, ahead of other countries worldwide. On the other hand, anti-inflammatory agents such as steroidal eye drops are mainly used, because cyclosporine eye drops are not approved for DED in Japan. Accordingly, the current practice pattern for dry eye patients might be unique. However, at present little is known regarding the actual clinical practice pattern and treatment modalities for DED.
Based on this information, we conducted a clinic-based survey of DED, known as DECS-J (Dry Eye Cross-Sectional Study in Japan). The purpose of the study was to review the clinical characteristics of DED patients and to assess the current clinical practice pattern in eye clinics.
Methods
Ethics
This study protocol was approved by the Institutional Review Board of Clinical Study of Ryogoku Eye Clinic Tokyo, Japan. This study was conducted in accordance with the guidelines of the World Medical Association Declaration of Helsinki and Ethical Guidelines for Medical and Health Research involving Human Subjects in Japan. The subjects received a full explanation of the procedures and provided their written informed consent for participation prior to inclusion in the study. The study was registered in the public registration system [University Hospital Medical Information Network: UMIN (Registries No. UMIN 000015890)].
Study Subjects
DECS-J was a cross-sectional, observational study conducted at ten eye clinics in Japan. The ten study sites covered the four main islands of Japan. All investigators at the study sites had a special interest in ocular surface disorders and DED and were certified members of the Japanese Dry Eye Society. To achieve high standards for the survey, investigators’ meetings were held twice prior to the start of patient enrollment to discuss study protocols and examination procedures. An instructional DVD demonstrated the standard examination procedures including lid margin evaluation, and a sample photograph showing the grading system of each van Bijsterveld grading system and NEI grading system was prepared and distributed to each investigator.
Outpatients who were ≥20 years old and had already been diagnosed as having dry eye as well as those who were newly diagnosed with dry eye were consecutively enrolled. Diagnosis of DED was based on the diagnostic criteria defined by the Japan Dry Eye Society [2]. The diagnostic criteria were as follows: (1) one or more abnormal tear examination results [Schirmer I test ≤5 mm or tear film break-up time (TBUT) ≤5 s], (2) abnormal results in ocular surface vital staining tests (kerato-conjunctival staining score of van Bijsterveld ≥3) and (3) the presence of symptoms of DED. Subjects who met two of the criteria (probable dry eye) and all three criteria (definite dry eye) were included in the study. Up to 50 patients were enrolled at each of the ten study sites from 1 December 2014 to 28 February 2015.
Clinical Assessment
Tear Function Tests and Ocular Surface Evaluation
Ophthalmic examinations included assessment of kerato-conjunctival vital staining with fluorescein sodium, TBUT, and the Schirmer I test.
Test strips containing fluorescein sodium (Fluores Ocular Examination Test Paper, Ayumi Pharmaceutical Co., Tokyo, Japan) were used for measurement of TBUT and kerato-conjunctival vital staining. After applying the tip of a moistened test strip to the inferior temporal tear meniscus, patients were asked to blink several times to ensure adequate mixing of the fluorescein dye with tears. The time interval between the last complete blink and the appearance of the first corneal dark spot was measured using a stopwatch, with the mean of three measurements regarded as the TBUT in this study. Then, kerato-conjunctival damage was investigated. Corneal fluorescein staining was evaluated according to the National Eye Institute (NEI) grading system [16]. Briefly, corneal staining was graded with a score of 0–3 assigned to each of five corneal zones (superior, nasal, central, inferior, and temporal) with a maximum total score of 15. The fluorescein staining score of kerato-conjunctiva was determined according to the grading system of van Bijsterveld [17], where each eye was divided into three sections (temporal conjunctiva, cornea, and nasal conjunctiva) and scored from 0 to 3. The final score ranged from 0 (minimum) to 9 (maximum) points. The Schirmer I test was performed without topical anesthesia, following all other examinations. Schirmer’s Test Strip (Ayumi Pharmaceutical Co., Tokyo, Japan) was placed at the outer one-third of the temporal lower conjunctival fornix for 5 min. The strips were then removed, and the length of filter paper that had been dampened (in mm) was recorded. To avoid the influence of kerato-conjunctival staining on the Schirmer I test, we waited a minimum interval of 15 min between tests.
MGD and friction-related conditions including lid wiper epitheliopathy, conjunctivochalasis, and superior limbic keratoconjunctivitis (SLK) were also evaluated. Evaluation of meibomian gland function was performed on one-third of the central site of the upper eyelid, according to the Japanese MGD criteria, as follows: presence or absence of (1) abnormal findings around the orifice of the meibomian gland such as vascular engorgement, anterior or posterior replacement of the mucocutaneous junction, and irregular lid margin; (2) orifice obstruction including plugging, pouting, and ridge; (3) secretion by compression classified as hyper-, normal, and hypo-secretion [18]. Friction-related conditions were determined as presence or absence of lid wiper epitheliopathy (upper and lower lid), conjunctivochalasis (on the lower temporal, central, and nasal sites), and SLK.
Subjects’ Background Information and Dry Eye Symptoms Questionnaire
Background information was collected from medical records and/or by interviewing the subject. Collected information included sex, age, duration of DED, therapies for dry eye and medical history, history of ocular surgeries, CL wear, hours of visual display terminal (VDT) tasks, and ocular and systemic comorbidities. Investigators also recorded the types of DED treatment at the study date.
The Dry Eye-Related Quality of Life Score (DEQS) questionnaire evaluates the severity of dry eye-associated symptoms and the multifaceted effect of DED on the patient’s daily life [19]. The questionnaire used in this study has been evaluated for its internal consistency, reproducibility, validity, and responsiveness for use in the Japanese population. The score derived from this questionnaire was considered to be a subjective measure of DED symptoms, whereby 0 indicates the best score and 100 the worst.
As described earlier, diagnosis of DED was based on the diagnostic criteria defined by the Japan Dry Eye Society [2]. Subjects who met two of the criteria (probable dry eye) and all three criteria (definite dry eye) were included in the study. In addition, study site investigators defined and recorded the dry eye subtype based on the patient’s background, clinical findings, and subjective symptoms. The criteria for aqueous tear deficient dry eye (Schirmer I test ≤5 mm and subjective symptoms) and those for short-BUT-type dry eye (TBUT ≤5 s, Schirmer I test >5 mm, and kerato-conjunctival score <3) were encouraged. However, the distinct observance of these criteria was not obligatory in this study. Subtype diagnosis such as CL-related DED and MGD-related DED were used when study site investigators determined the presence of an apparent causative mechanism.
Investigators also recorded the prescribed drugs and/or means of treatments for DED immediately after the investigation.
Statistical Analyses
SAS software, version 9.2 (SAS Inc., Cary, NC, USA) was used to calculate the proportion, mean, and standard deviation. Continuous data are expressed as the mean ± standard deviation. The data collected from both eyes of the subjects were included in the study.
Results
Characteristics of the Study Population
In this study, 463 patients were initially enrolled. However, nine cases were excluded because of disqualification, three patients were <20 years of age, and two patients withdrew consent. Therefore, 14 cases in total were excluded, and 449 cases (63 male and 386 female; mean age, 62.6 ± 15.7 years) were included in the final analysis.
The characteristics of the study population are summarized in Table 1. Of these, 377 patients (84.0%) had already received dry eye therapies, and 72 patients (16.0%) were newly diagnosed with dry eye. Eighty patients (17.8%) were CL wearers, and 123 were VDT workers (27.4%). Ocular and systemic comorbidities were present in 135 (30.1%) and 213 patients (47.4%), respectively. Ocular comorbidities comprised cataract (59 cases, 13.1%), glaucoma (43 cases, 9.6%), allergic conjunctivitis (28 cases, 6.2%), retinal diseases (10 cases, 2.2%), and others (24 cases, 5.3%). Systemic comorbidities comprised hypertension (103 cases, 22.9%), sleep disorders (50 cases, 11.1%), diabetes mellitus (16 cases, 3.6%), rheumatoid disease (15 cases, 3.3%), depression (8 cases, 1.8%), and others (113 cases, 25.2%). Oral medications administered for systemic comorbidities included antihypertensive drugs (98 cases, 21.8%), sleep-inducing drugs (55 cases, 12.2%), antidepressants (20 cases, 4.5%), and others (147 cases, 32.7%).
Tear and Ocular Surface Examination
Results of the ocular surface and tear examinations are shown in Table 2. The mean TBUT, Schirmer I test value, kerato-conjunctival score, and cornea staining score (NEI) were 3.0 ± 1.6 s, 9.9 ± 9.3 mm, 2.6 ± 1.9, and 3.5 ± 3.4, respectively (Table 2). According to the Japanese dry eye diagnostic criteria cutoff value, the proportion of positive subjects was 94.9% for TBUT (≤5 s), 54.6% for the Schirmer I test (≤5 mm), and 57.0% for the kerato-conjunctival score (≥3 points).
Results for meibomian gland abnormalities and friction-related conditions are presented in Table 3. Findings suggestive of meibomian gland orifice obstruction such as plugging were observed in 42.3% of patients; hyposecretion of meibum was observed in 37.0%. Regarding friction-related conditions, conjunctivochalasis was the most common, and nasal/temporal chalasis was observed in more than 30% of patients.
Dry Eye Subtypes and their Characteristics
The prevalence of DED subtypes judged by the physician in charge are shown in Table 4. The most prevalent subtype of dry eye was aqueous-deficiency dry eye, which included 35.0% of all patients, followed by short-BUT-type dry eye, which comprised 26.7%, then CL related (7.8%), Sjögren syndrome related (7.6%), MGD related (7.6%), and friction related (6.4%).
The results of the ocular surface and tear examinations of DED subtypes are shown in Table 5. We confirmed that a shortened TBUT of less than 5 s is the most common feature of dry eye, regardless of the subtype. The TBUT in Sjögren syndrome was the shortest, followed by short-BUT-type dry eye.
The mean DEQS score across all participants was 26.8 ± 20.6 (0–98.3). For subscales of DEQS, the Bothersome Ocular Symptoms score was 33.5 ± 22.2 (0–100), and the Impact on Daily Life and quality of life (QOL) was 22.3 ± 22.3 (0–97.2). The results of DEQS in DED subtypes are shown in Table 5. Sjögren syndrome was associated with the worst symptoms. The DEQS scores of the short-BUT-type and aqueous deficiency dry eye were nearly equal (p = 0.91, two-sample t test).
Distribution of Current Treatments
Numbers and percentage of patients treated with each treatment modality are shown in Table 6. The most common treatments used were hyaluronic acid eye drops (296 cases, 65.9%) followed by two novel drugs for the treatment of DED, diquafosol and rebamipide, which were used in 40.1% (180 cases) and 22.7% (102 cases), respectively.
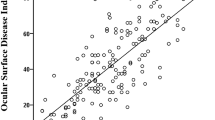
Concerning the combination of treatment modalities, single therapy was chosen in 214 cases (47.7%), whereas 2 drugs were concurrently used in 174 cases (38.8%) and more than 3 drugs in 49 cases (10.9%, Supplemental Table 1). In single therapy, hyaluronic acid eye drops (120 cases), diquafosol (59 cases), and rebamipide (11 cases) were prescribed. A distribution map of the current treatment modalities (diquafosol, rebamipide, hyaluronic acid, artificial tears, and fluorometholone) is shown in Fig. 1. Treatment options other than these five eye drops were used in three cases (0.6%). In total, the most prevalent treatment modalities were first hyaluronic acid eye drops alone (120 cases, 26.7%), second diquafosol plus hyaluronic acid eye drops (69 cases, 15.4%), third diquafosol (59 cases, 13.1%), and fourth rebamipide plus hyaluronic acid eye drops (37 cases, 8.2%).
Distribution map of the current treatment modalities (diquafosol, rebamipide, hyaluronic acid, artificial tears, and fluorometholone). Only three patients (0.6%) were prescribed a different treatment apart from these five eye drops. Hyaluronic acid eye drops, two mucin secretagogues, diquafosol and rebamipide, and artificial tears are the main agents for dry eye treatment in Japan. Several combinations of these four eye drops are prescribed. Fluorometholene is added in combination with these eye drops as necessity. DECS-J Dry Eye Cross-Sectional Study in Japan, DQS 3% diquafosol, MCS 2% rebamipide, HYA hyaluronic acid, AT artificial tears, FLU 0.1% fluorometholone
Discussion
In this cross-sectional, observational study, we assessed clinical characteristics of patients with DED who visited eye clinics in Japan. Regarding the ocular surface and tear examinations, the mean TBUT score across the study was 3.0 ± 1.6 s, the mean value of Schirmer I test was 9.9 ± 9.3 mm, and the mean kerato-conjunctival score was 2.6 ± 1.9 points. When the cutoff value was applied using the Japanese dry eye diagnostic criteria, 94.9% of participants were associated with a shortened TBUT (≤5 s) and the high level of prevalence of shortened TBUT was consistent regardless of dry eye subtype. In the Osaka study, a dry eye survey of VDT workers in Japan, it was reported that 94.6% of participants exhibited a shortened TBUT [20]. These results confirmed that the instability of tear film is involved as a core mechanism of DED. Rege et al. have also reported that TBUT is the test most likely to diagnose mild dry eye and that it has better sensitivity as well as specificity than other tests [14].
Regarding the other objective examinations, 54.6% of subjects had an abnormal Schirmer I test, and 57.0% had an abnormal kerato-conjunctival score in this study. These results are quite different from those of the Osaka study (Schirmer I test ≤5 mm: 19.3%, kerato-conjunctival score ≥3: 24.2%) [20]. Reasons for these differences may relate to the increased age of patients in this study compared to those in the Osaka study as well as differences between the subjects, for example, VDT workers and clinic visitors. As mentioned earlier, only a limited proportion of patients with DED seek medical care. DED patients who visit eye clinics may have more severe subjective symptoms and objective findings. Lienert et al. recently reported that factors associated with the severity of DED in clinic visitors include spending >$20 per month on DED treatments, a history of MGD, and the use of systemic beta-blockers [21]. This observation also suggests a distinction between clinic patients and the general population.
In this study, investigators at each clinical site judged the dry eye subtype based on the patient’s background, clinical findings, and subjective symptoms. There may be a slight locational difference in judgment; the most prevalent subtype was aqueous-deficient dry eye, which accounted for 35.0% of all patients, followed by short-BUT-type dry eye, which comprised 26.7%. The two main subtypes, aqueous tear-deficient and short-BUT type, were associated with different Schirmer I test values and kerato-conjunctival staining scores, although a shortened TBUT was common in both. Interestingly, the DEQS scores for these subtypes were approximately the same; in other words, both subtypes have a similar subjective severity and impact on QOL. This is in agreement with the recent report by Yokoi et al. [20]. It should be noted that the severity of subjective symptoms in short-BUT-type dry eye is similar to that of aqueous-deficient type dry eye, despite no or minor epithelial damage.
The prevalence of MGD-related DED was low (7.6%) in the current study. Previous clinic-based studies have reported that MGD-related dry eye was more common than aqueous-deficient dry eye [13, 15, 22]. Rege et al. also reported a similar prevalence of aqueous-deficient dry eye and lipid anomaly dry eye [14]. Investigators at clinical sites in this study likely chose to assign these to short TBUT or aqueous-deficient dry eye subtypes mainly because the criteria for aqueous tear-deficient dry eye and those for short-BUT-type dry eye were encouraged. In the present study, however, abnormal findings of meibomian glands such as plugging and hypo-secretion of meibum were observed in approximately 40% of cases. Therefore, these results suggest that a common set of patients objectively have had signs of MGD, although these findings were not reflected in the DED subtype diagnosis. A similar situation extends to the friction-related conditions, as there was a higher presence of objective friction-related findings compared to those that were judged as this subtype (6.4%). Yamaguchi et al. reported low rates of MGD and conjunctivochalasis among DED patients (3.4% and 5.5%, respectively) in their subgroup analysis in a prospective observational study in Japan [23, 24]. The influence of MGD and friction-related conditions on the severity of dry eye might be underestimated in Japan, and these issues should be clarified in a further study.
We also investigated treatment modalities in DED patients in Japan. In this study, hyaluronic acid eye drops were prescribed in 296 cases (65.9%), followed by diquafosol and rebamipide, which were used in 40.1% and 22.7% of cases, respectively. In these cases, combinations with mucin secretagogues such as diquafosol or rebamipide were common choices (Supplemental Table 1; Fig. 1). These results were significantly different from our previous hospital-based survey of dry eye patients in 2008 [25]. In the previous report, hyaluronic acid eye drops were used in 73.7%, followed by artificial tears (33.9%), steroidal eye drops (18.6%), and over-the-counter (OTC) eye drops (12.7%). Since diquafosol and rebamipide have become available in Japan, they are now important modalities for the treatment of DED in Japan. On the other hand, artificial tears and OTC eye drops appear to be less commonly used. Regarding anti-inflammatory agents, steroidal eye drops (0.1% fluorometholone) were prescribed in 57 cases (12.7%) in this study. Although cyclosporine eye drops are commonly used in the US, EU countries, and Korea [26], cyclosporine eye drops are not approved for treatment of DED in Japan.
Importantly, only 0.4% were prescribed treatment options apart from the following five agents: hyaluronic acid, diquafosol, rebamipide, artificial tears, and fluorometholone. In other words, almost all of the patients are treated with these five eye drops as a single modality or in combination. Concerning the combination of treatment modalities, single therapy was chosen in 47.7%, whereas combination therapy consisting of two or more agents was used in 51.2% of patients. Patterns of combination therapies are numerous and complex. To help understand current treatment modalities and their combinations (diquafosol, rebamipide, hyaluronic acid, artificial tears, and fluorometholone), we created a distribution map of combination therapies (Fig. 1). Although current treatment is mainly with hyaluronic acid eye drops, the combination with two novel drugs, diquafosol and rebamipide, is also prevalent. Topical anti-inflammatory agents were often prescribed in combination with these mucin secretagogues.
Thus, the emergence of diquafosol and rebamipide may represent a paradigm shift in DED treatment in Japan. In this study, almost all subjects with DED (94.9%) exhibited a shortened TBUT (≤5 s) regardless of dry eye subtype. These results suggest that tear film instability is the most common feature of DED and may be involved as a core mechanism of its pathogenesis. Both diquafosol and rebamipide are recognized as mucin secretagogues, whereas recent studies have shown that they each have different and unique actions. Diquafosol facilitates the secretion of water from the conjunctival epithelium as well as secretion of mucins from goblet cells. Rebamipide has a role in reducing inflammation at the ocular surface. Experimental studies suggest that both diquafosol and rebamipide enhance the expression of membrane-associated mucins in the cornea and conjunctiva. According to these reports, diquafosol and rebamipide may work to improve tear stability, which is very important for dry eye treatment. We have shown that diquafosol and rebamipide have now become important modalities for the treatment of DED in Japan.
This study has several limitations. Although this was a multicenter study performed in various areas in Japan, the number of study sites may have been too small to fully represent the number of Japanese eye clinics. Therefore, the number of cases may be an insufficient representation of patients who visit eye clinics in Japan. Although all the investigators were dry eye specialists educated to the same standards and who followed the same guidelines, there may still be some variation in their evaluations. Judgment of the dry eye subtype depended on the individual investigators, considering the patient’s clinical assessment, background information, and symptom questionnaire. For example, in this study it is possible that the short-BUT-type dry eye may include various subtypes such as MGD-related dry eye and contact lens-related dry eye in addition to the short-BUT-type dry eye [18]. Future studies need to address these limitations to further elucidate the clinical characteristics of patients with DED who visited eye clinics in Japan.
Conclusion
We investigated the clinical features and treatment modalities in this clinic-based survey of dry eye patients in Japan. In total, 94.9% of patients were associated with shortened TBUT (≤5 s), confirming that unstable tear film appears to be a core mechanism of DED. The most common dry eye subtype was aqueous tear-deficient (35.0%) followed by short-BUT type dry eye (26.7%). The current treatment choice mainly consisted of hyaluronic acid, two novel mucin secretagogues, diquafosol and rebamipide, and steroidal eye drops. The emergence of diquafosol and rebamipide has had a significant impact on DED treatment in Japan.
References
The Definition and Classification of Dry Eye Disease: report of the Definition and Classification Subcommittee of the International Dry Eye Work Shop. Ocul Surf. 2007;5:75–92.
Shimazaki J, Tsubota K, Kinoshita S, et al. Definition and diagnosis of dry eye. Atarashii Ganka (in Japanese). 2007;4:181–4.
Uchino M, Yokoi N, Uchino Y, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol. 2013;156:759–66.
Lee AJ, Saw SM, Gazzard G, Koh D, Widjaja D, Tan DT. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol. 2002;86:1347–51.
Moss SE, Klein R, Klein BE. Long-term incidence of dry eye in an older population. Optom Vis Sci. 2008;85:668–74.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26.
Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010–2011. Am J Ophthalmol. 2014;158:1205–14.
Shimmura S, Shimazaki J, Tsubota K. Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eye. Cornea. 1999;18:408–11.
Pflugfelder SC. Prevalence, burden, and pharmacoeconomics of dry eye disease. Am J Managed Care. 2008;14:S102–6.
Yazdani C, McLaughlin T, Smeeding JE, Walt J. Prevalence of treated dry eye disease in a managed care population. Clin Ther. 2001;23:1672–82.
Um SB, Kim NH, Lee HK, Song JS, Kim HC. Spatial epidemiology of dry eye disease: findings from South Korea. Int J Health Geogr. 2014;15(13):31.
Tesón M, López-Miguel A, Neves H, et al. Influence of climate on clinical diagnostic dry eye tests: pilot study. Optom Vis Sci. 2015;92(9):e284–9.
Albietz JM. Prevalence of dry eye subtypes in clinical optometry practice. Optom Vis Sci. 2000;77:357–63.
Rege A, Kulkarni V, Puthran N, Khandgave T. A clinical study of subtype-based prevalence of dry eye. J Clin Diagn Res. 2013;7:2207–10.
Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31:472–8.
Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21:221–32.
van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol. 1969;82:10–4.
Amano S. MGD Working Group. Definition and diagnostic criteria for meibomian gland dysfunction. Atarashii Ganka (in Japanese). 2010;27:627–31.
Sakane Y, Yamaguchi M, Yokoi N, et al. Development and validation of the Dry Eye-Related Quality-of-Life Score questionnaire. JAMA Ophthalmol. 2013;131:1331–8.
Yokoi N, Uchino M, Uchino Y, et al. Importance of tear film instability in dry eye disease in office workers using visual display terminals: the Osaka study. Am J Ophthalmol. 2015;159:748–54.
Lienert JP, Tarko L, Uchino M, et al. Long-term natural history of dry eye disease from the patient’s perspective. Ophthalmology. 2016;123:425–33.
Tong L, Chaurasia SS, Mehta JS, Beuerman RW. Screening for meibomian gland disease: its relation to dry eye subtypes and symptoms in a tertiary referral clinic in Singapore. Invest Ophthalmol Vis Sci. 2010;51:3449–54.
Yamaguchi M, Nishijima T, Shimazaki J, et al. Clinical usefulness of diquafosol for real-world dry eye patients: a prospective, open-label, non-interventional, observational study. Adv Ther. 2014;31:1169–81.
Yamaguchi M, Nishijima T, Shimazaki J, et al. Real-world assessment of diquafosol in dry eye patients with risk factors such as contact lens, meibomian gland dysfunction, and conjunctivochalasis: subgroup analysis from a prospective observational study. Clin Ophthalmol. 2015;9:2251–6.
Mizuno Y, Yamada M, Miyake Y, Dry Eye Survey Group of the National Hospital Organization of Japan. Association between clinical diagnostic tests and health-related quality of life surveys in patients with dry eye syndrome. Jpn J Ophthalmol. 2010;54:259–65.
Song JS, Hyon JY, Lee D, et al. Current practice pattern for dry eye patients in South Korea: a multicenter study. Korean J Ophthalmol. 2014;28:115–21.
Acknowledgements
This study and publication charges were funded by the Japan Dry Eye Society, Tokyo, Japan, and Santen Pharmaceutical Co., Ltd., Osaka, Japan.
The present study was conducted by the joint study organization of the Dry Eye Society and Santen Pharmaceutical Co., Ltd. Both organizations contributed to the creation of documents including the study protocol, management of study progress, and provided information and support to the study sites, evaluation of the data analysis, disclosure of the outcome of the study, and entry/update of the present study in the public registration system.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
The DECS-J Study Group: The following individuals participated in the study. Central Unit: Motoko Kawashima, Masakazu Yamada, Kazuhisa Suwaki, Chika Shigeyasu, Yoshimune Hiratsuka, Norihiko Yokoi, Kazuo Tsubota. Study group investigators and clinical sites: Yoshitsugu Tagawa (Kitaichijo Tagawa Eye Clinic, Sapporo, Hokkaido, Japan), Seika Den (Akasaka Tokyu Shimazaki Eye Clinic, Tokyo, Japan), Miki Iwasaki (Ryogoku Eye Clinic, Tokyo, Japan), Hiroshi Saito (Saito Eye Clinic, Saitama, Japan), Reiko Ishida (Ishida Clinic, Shizuoka, Japan), Aoi Komuro (Shijo-karasuma Komuro Eye Clinic, Kyoto, Japan), Naoki Iwasaki (Iwasaki Eye Clinic, Osaka, Japan), Harue Matsumoto (Matsumoto Eye Clinic, Tokushima, Japan), Tomoko Goto (Hanamizuki Eye Clinic, Ehime, Japan), Atsuko Kiyosawa (Kiyosawa Eye Clinic, Fukuoka, Japan).
Disclosures
Kazuhisa Suwaki: employee of Santen Pharmaceutical Co., Ltd.
Masakazu Yamada: consultant for Otsuka Pharmaceutical Co. Ltd, and Johnson & Johnson Vision Care Co.
Norihiko Yokoi: consultant for Kissei Co., Ltd., and Rohto Co., Ltd.
Kazuo Tsubota: consultant, speaker’s bureau member and grant recipient of Santen Pharmaceutical Co., Ltd.; speaker’s bureau member and grant recipient of Otsuka Pharmaceutical Co., Ltd.
Motoko Kawashima, Chika Shigeyasu, Yoshimune Hiratsuka, and Miki Uchino have nothing to disclose.
Compliance with Ethics Guidelines
This study protocol was approved by the Institutional Review Board of Clinical Study of Ryogoku Eye Clinic Tokyo, Japan. This study was conducted in accordance with the guidelines of the World Medical Association Declaration of Helsinki and Ethical Guidelines for Medical and Health Research involving Human Subjects in Japan. The subjects received a full explanation of the procedures and provided their written informed consent for participation prior to inclusion in the study. The study was registered in the public registration system [University Hospital Medical Information Network: UMIN (Registries No. UMIN 000015890)].
Data Availability
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/E887F0605D6BC454.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kawashima, M., Yamada, M., Suwaki, K. et al. A Clinic-based Survey of Clinical Characteristics and Practice Pattern of Dry Eye in Japan. Adv Ther 34, 732–743 (2017). https://doi.org/10.1007/s12325-017-0487-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0487-x