Abstract
Friedreich ataxia (FRDA) is the most frequent inherited ataxia. Neuropsychological studies suggest that FRDA may be associated with specific cognitive impairment. Very little is known about the relation between cognitive performance, demographics and disease-related parameters, such as GAA repeat size, age of onset and disease duration. The present investigation aimed at assessing cognitive functions in a representative sample of FRDA patients and at identifying the most relevant disease-related parameters. Twenty-nine adult FRDA patients underwent neuropsychological tests assessing executive functions, attention, memory and visual perception. Performance was compared with 28 age- and education-matched controls as well as with standardized norms. The relation between neuropsychological outcome, demographical variables and disease-related parameters was assessed. Cognitive impairment affected only a subgroup of patients and mostly concerned attentional and executive functions. Good cognitive performance was associated with a later disease onset, shorter GAA repeat length and lower burden of disease. Age at disease onset has been found to be a good predictor when a cut-off of 14 years was chosen. No correlation was found between cognitive performance and education, age or disease duration. The present study extends earlier findings in FRDA showing that performance in attentional and executive function tasks is best predicted by the age at disease onset. Moreover, executive functions show a clear relationship to disease severity and repeat size of the shorter GAA allele. These findings therefore have important implications for patient counselling regarding education and career choices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Friedreich ataxia (FRDA) is the most common inherited ataxia with an estimated prevalence of 2–4/100,000 [1]. Though neuropsychological impairments have been described [2–6], evidence about the relation between cognitive performance and disease parameters including the genetic mutation is extremely scarce. The present study investigates the cognitive profile of adult FRDA patients and the impact of disease variables on cognition.
Individuals with FRDA have identifiable mutations in the frataxin gene (FXN) on chromosome 9. The most common mutation accounting for more than 96 % of cases is a homozygous GAA triplet-repeat expansion in intron 1 of FXN [7]. There is an inverse correlation between age of onset and disease severity with the length of the smaller GAA repeat expansion (GAA1) [1, 8]. Expanded GAA repeats lead to triplex DNA formation and/or heterochromatin-mediated silencing. Both result in reduced transcription of FXN and decreased production of the mitochondrial protein frataxin [9, 10]. Frataxin is suggested to be involved in iron-dependent mitochondrial pathways, heme synthesis, iron–sulphur cluster formation and respiratory chain activity [11, 12]. In consequence, frataxin deficiency leads to impairment of mitochondrial oxidative metabolism, increased oxidative stress and cell apoptosis. Neuronal cell degeneration in FRDA in the central nervous system is most pronounced in brainstem, spinal cord and cerebellum with the main neuropathological findings of atrophy in dorsal root ganglia, the dentate nucleus, as well as spinocerebellar and corticospinal tracts [13, 14].
Clinically, FRDA is characterized by slowly progressive ataxia with the clinical hallmarks of gait and limb ataxia, dysarthria, depressed tendon reflexes, as well as loss of position and vibration sense [15]. A number of neuropsychological studies suggest that FRDA is also associated with cognitive changes (for a review see [15]). Most studies converge on the view that speed of information processing is reduced in FRDA and that this slowing cannot be explained by motor difficulties and ataxia alone (e.g., [2, 4, 16–19]). Executive dysfunction has been described repeatedly [2, 20]; for different results, see [16]. Mantovan et al. [21] found a specific intelligence profile with poor concept formation and reduced visuospatial abilities, besides slow processing and deficient performance in an implicit learning task. Nieto et al. [6] reported reduced processing speed, reduced verbal fluency, lower scores in verbal learning, visuo-perceptive and visuo-constructive problems as well difficulties in action naming. Deficits have been attributed to executive problems and parieto-temporal dysfunction caused by the interruption of cerebro-cerebellar loops [6]. In a series of investigations Corben et al. systematically assessed the interplay between cognition and motor behaviour in FRDA. Patients had significant difficulties in inhibiting inappropriate automatic responses associated with stimulus–response incompatibility in an interference task [17]. They did not use advance motor information to improve their performance as healthy controls did [22]. FRDA patients showed a disproportionate increment of movement times in targets with increasing difficulty. Task performance was modified by the time spent in preplanning and in online controlling the accuracy of movement [19]. The authors attributed FRDA patients' specific behaviour to deficient cerebro-ponto-cerebello-thalamo-cerebral loops. As a consequence, patients would have difficulties to access prefrontal regions essential in preplanning and management of movement.
Methodological issues make the comparison between neuropsychological studies difficult. Patient samples were often small and sometimes heterogeneous as regards age and intelligence level. Different test batteries were used in the various studies. Moreover, investigations were mostly based on group comparisons between FRDA patients and healthy controls without reference to standardized norms. Several studies included patients without genetic confirmation which makes the inclusion of non-FRDA ataxias in the patient samples likely. Few studies have assessed the correlation between neuropsychological outcome and parameters of disease severity, such as GAA1 repeat size of FXN, age of disease onset and disease duration. Some neuropsychological investigations were performed prior to the identification of the FRDA mutation (e.g., [4, 23, 24]); in other studies, diagnosis was not supported by genetic analysis (e.g., [2, 16]). Age of onset, but not duration of disease, was found to correlate inversely with performance in an interference task [17] and in a sequential movement task [22]. These findings were taken as evidence for an impact of FRDA on the development of motor cognition [17, 22], independent of the effect of disease duration. However, in a further study of the same group [19] no significant correlation was found between movement kinematics and disease parameters. Klopper et al. [18] reported a correlation of GAA repeat length with working memory performance, but not with measures of volitional sustained attention. Mantovan et al. [21] found correlations between disease duration and two executive function tasks assessing selective attention and planning. Thus, evidence on the relation between disease parameters and cognition is scarce, limited to specific functions and rather inconsistent. Age at disease onset seems to be an important factor [17, 22] which is, however, related to a number of disease parameters, including GAA repeat number and overall disease severity.
The present investigation aimed at assessing cognitive functions in a representative sample of genetically confirmed adult FRDA patients and determining the proportion of patients scoring in the impaired range in the single cognitive domains. Moreover, the study aimed at identifying the most relevant disease-related parameters predicting performance in neuropsychological tasks.
Participants and Background Tasks
Twenty-nine patients with genetically confirmed FRDA were recruited from the Ataxia Clinic of the Department of Neurology, Innsbruck Medical University (for demographical data, clinical data and background tasks see Table 1). All patients underwent neurological assessment, were rated according to the SARA scale [25], and performed an 8-m foot walking test (8 MW) [26–28]. Twelve out of 29 patients could not perform the task due to physical limitations. Manual dexterity was assessed by a 9-hole pegboard task [26–28]. Speed of articulation was measured in a syllable repetition task (PATA) [26–28]. Participants were asked to repeat the syllables ‘PATA’ as often as possible within 10 s. Reading speed was assessed by the International Reading Speed test [29]. A vocabulary task was used to estimate premorbid verbal intelligence [30]. A scale of activities of daily living (ADL) [26, 28] was applied (scores from 0 to 36; 0 = normal/independent, 36 = fully dependent on help). The control group included 28 healthy age- and education-matched participants. Significant differences between patients and controls were found in all tasks assessing motor speed, articulation and dexterity (Table 1), but not in age, education or estimated verbal IQ (Table 1). All participants gave written informed consent to participate in the study. The study was approved by the local ethics committee of the Innsbruck Medical University (approval number: AM 3944, meeting number: 287/4.1).
Neuropsychological Assessment
Patients and controls performed a battery of standardized neuropsychological tasks assessing attentional functions [31], executive functions, visual perception, as well as verbal learning and memory. Table 2 shows the cognitive domains and the test battery used in the present study. In the TAP alertness task, subjects have to react as fast as possible to a cross presented on the computer screen by pressing a response key. In two blocks, the cross is presented without warning (intrinsic alertness); in two blocks, the cross is presented after a warning tone in varying time intervals (600–1,500 msec; phasic alertness). In all blocks, the stimulus is presented for a max 2,000 msec (until reaction), the interstimulus interval (from reaction to next stimulus or warning) varies between 1,800 and 2,700 msec. In the present investigation, we are particularly interested in anticipations of reactions and in omissions, but not in reaction times which are influenced by motor processing. In the divided attention task, two dimensions (geometrical symbols and different tones) have to be attended simultaneously. Whenever a target appears (one out of four geometrical symbols or two identical tones in a row), subjects have to answer by key press. Tones are presented for 110 msec, the interstimulus interval is 825–1,650 msec, visual stimuli are presented for 500 msec, the interstimulus interval is 2,000 msec. Important outcome measures are errors and omissions. Executive functions (see Table 2) were assessed by standardized tests including semantic word fluency (animals/minute [32]) and phonemic word fluency (s-words/minute [32]), a computerized adaptation of the Tower of London task (Planungstest [33], eight problems of increasing difficulty requiring three to eight moves), a Stroop task (colour word interference task [34]), and a digit span task (digit span forwards, digit span backwards [35]). Visual perception was screened by two subtests of VOSP [36], one requiring the identification of incomplete letters, the other requiring the discrimination of the spatial position of single dots. Learning and memory was assessed by a word list learning task (VLMT [37]; word list presented five times, short-delay free recall, long-delay free recall, recognition trial).
Test duration was approximately 90 minutes. Patients performed the tests in a single session though they were informed that they could split the session. Age-adjusted norms were used when available [32, 34–37].
Statistical Analysis
Age, education and performance in neuropsychological tasks were assessed by Student's independent samples two-tailed t testsFootnote 1, memory recall by repeated measures ANOVA (short/long delay). Gender distribution was assessed by χ 2 test. The number of participants who had omissions, errors or anticipations in attention tasks was compared by χ 2 tests between groups. In a further analysis, test performance of each single patient was classified as either impaired (performance below the tenth percentile of standardized norms; including mild to severe impairment) or intact (performance equal or above the tenth percentile of standardized norms). For the patient group, a correlation analysis (Pearson) was performed between tasks that require a verbal response and performance in the syllable repetition task as well as between tasks that require a manual response and performance in the pegboard task (dominant hand).
A selective summary score was calculated taking into account attentional and executive functions (executive score). Note that in this score we include only accuracy measures and scores which are not significantly correlated with articulation or manual dexterity in the patient group. One point each was credited when no anticipation (one point) or omission (one point) occurred in the two alertness tasks (without warning, with warning), when no error (one point) or omission (one point) occurred in the divided attention task, when performance was equal or above the tenth percentile in verbal fluency tasks (semantic fluency, one point; phonemic fluency, one point), in the Stroop task (interference condition; one point) in the Tower of London (one points; overall sum 10).Footnote 2
A Spearman rank-order correlation analysis was carried out between the executive score and demographic variables as well as between executive score and disease-related variables (age at the time of the investigation, age at disease onset, disease duration, education, GAA repeat number of the shorter allele of the FXN gene, SARA score). In order to evaluate the joint effect of demographical and clinical variables on neuropsychological performance (executive score) a hierarchical regression analysis was performed. Demographical variables (age, education) and clinical variables (age at disease onset, education, GAA repeat number, SARA score) were entered as possible predictors, using the stepwise forward method for variable selection. Finally, a ROC analysis was performed to assess whether clinical variables would predict a good neuropsychological performance (executive score equal or above the controls' median).
Results
Group Comparisons
Significant group differences were found in the verbal fluency tasks, semantic and phonemic task condition. Scores in the fluency tasks did not significantly correlate with articulation speed. In the Stroop task, patients differed from controls in interference naming. Notably, also the difference between interference and colour naming condition (indicating inhibition processes) differed between groups (Table 3). Performance in the interference condition was not significantly correlated with articulation speed in the patient group, ruling out articulation difficulties as a main source of prolonged interference naming. In executive function tasks, the proportion of patients scoring in the impaired range varied between 10 and 31 %.
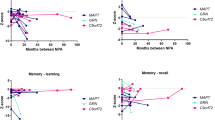
No group differences appeared in the digit span task and in the Tower of London task. Visual perception was intact in patients and controls. Verbal learning, memory recall and recognition memory were comparable between groups. In the analysis of memory recall repeated measures, ANOVA showed no effect of delay (short/long delay), group or interaction between group and delay (Table 3).
In all attention tasks (TAP) significant group differences were found (Table 4). Frequency analysis showed that more patients than controls had omissions in the alertness task without warning, anticipations in the alertness task with warning and omissions in the divided attention task (Table 4). RTs were significantly slower in patients than in controls in the alertness task, in the divided attention task for visual stimuli, but not for auditory stimuli.Footnote 3 Since the answer was given by key press and RTs correlated with manual dexterity measured in the pegboard task these differences are not further interpreted (Spearman correlation: alertness without warning R = .701, alertness with warning R = .761, divided attention tones R = .548, divided attention visual stimuli R = .654). Oculomotor problems may also contribute to slow reaction times in response to visually presented stimuli.
Correlation Analysis and Disease-Related Variables
A Spearman rank-order correlation analysis between clinical variables and the executive score was computed for the patient group (executive score: patients median 7, minimum 2, maximum 9; controls median 8, minimum 6, maximum 10; Mann–Whitney U; Z = −3.56; p < .0001). Age at disease onset (R = .512; p = .005), GAA1 repeat length (R = −.404; p = .033) and SARA score (R = −.427; p = .021) were significantly correlated with the executive score. Age at the time of the investigation, education and disease duration were not significantly correlated with the executive score. No significant correlations were found between memory scores, visuoperception, verbal span and disease-related variables.
Regression Analysis
In a stepwise regression analysis with the predictors age, education, age at disease onset, duration of disease, GAA1 repeat length and SARA score and the dependent variable executive score, age at onset had a significant effect. Higher age at onset predicted better performance (R 2 = .21; β = .072; SE = .027; T = 2.63; p = .014). Age at disease onset is highly correlated with GAA1 repeat length (Spearman rank-order correlation; R = .738; p < .0001) and SARA score (R = .635; p < .0001). The variable GAA1 repeat length results as a significant predictor when correlating variables are removed from the analysis.
ROC Analysis
A ROC analysis was performed to assess whether disease-related variables (age of disease onset, GAA1 repeat length, SARA score) would predict a good neuropsychological performance. The cut-off was defined as the median score of controls (score of 8 or better in the executive score). By this analysis, we predict good performance, but cannot draw any conclusions on possible impairments. Age at disease onset proved to be a good predictor (area under the curve, AUC = .80), while SARA score (AUC = .725) and GAA1 repeat length were fair predictors (AUC = .717). When a cut-off of 14 years was chosen (disease onset ≤ age 14 vs. disease onset > age 14), sensitivity for a favourable outcome was 70 %, specificity was 73.6 %.
Discussion
This study assessed a range of neuropsychological domains in a sample of genetically confirmed adult FRDA patients. In the present study, we focus on cognitive group differences which are not explainable by slow output modalities. We will first consider differences between FRDA patients and controls and summarize possible neurological explanations. Then we discuss the relation between neuropsychological outcome and disease-related parameters.
Group differences were evident in alertness, in divided attention, selective attention and inhibition as well as in verbal fluency tasks. In contrast, no group differences were detected in working memory, planning, visual perception, verbal learning and memory. These results confirm earlier studies reporting lower scores of FRDA patients in tasks assessing specific executive functions, attentional control and processing speed [6, 17, 18]. In the Stroop task FRDA patients had significantly longer naming times than controls in the interference condition. They also showed significantly larger differences between interference and colour naming indicating difficulties in inhibiting automatic stimulus response associationsFootnote 4. Previous studies have shown that FRDA patients also have difficulties in inhibiting inappropriate automatic motor responses in situations of stimulus–response incompatibility [17]. The present study suggests that FRDA patients may show premature, inappropriate motor responses even in a simple alertness task when there is no conflict between stimulus and appropriate response. Since anticipations were more frequent in the condition with warning tone than in the condition without warning, anticipations may be attributed to a failure in inhibition rather than to problems related to motor planning and movement execution. FRDA patients also had omissions in the divided attention task, reflecting difficulties in sharing attention between two relevant dimensions. These findings are in line with a previous study [18] describing reduced performance in various tests of volitional sustained attention using auditory stimuli.Footnote 5
In verbal fluency tasks FRDA patients produced a lower number of items in both semantic and phonemic categories. Low scores in verbal fluency are a common finding in FRDA pointing to deficits in lexical and/or semantic search and monitoring [20]. Low verbal fluency scores cannot be explained by articulation difficulties alone, as the number of words produced in 1 min in the verbal fluency tasks (mean 12 and 22, respectively) was considerably lower than the number of words read in 1 min (113; Table 1). Moreover, verbal fluency was not correlated with articulation speed.
There is increasing evidence that the cerebellum is not solely responsible for motor control, but also contributes to cognitive and emotional processing [38, 39]. Cerebral cognitive association areas are linked with the cerebellar hemispheres via feedback loops involving the thalamus, as well as the nuclei of the pons and cerebellum [39]. Cerebellar degeneration itself however is usually mild in FRDA and typically occurs in more advanced disease stages. FRDA primarily affects the spinocerebellar tracts, the posterior columns and corticospinal tracts. Atrophy of the cerebellar grey matter of the dentate nuclei and efferent fibres is reported in FRDA [13]. There is increasing evidence for motor function associated with the dorsal part of the dentate nucleus whereas cognitive functions are associated with the ventral [34]. The ventrocaudal part of the nucleus dentatus has been shown to be involved in working memory, verb generation and visuospatial tasks by functional MRI in healthy humans [40, 41]. Projections of the dentate nuclei link the cerebellum to the thalamus, primary motor and premotor areas, as well as to prefrontal and parietal areas of the cerebral cortex via the cerebellar peduncles [42, 43]. As several MRI studies show, neurodegeneration in FRDA affects also the cerebellar peduncles, in particular the superior cerebellar peduncle [44, 45]. Thus, not only degeneration of the dentate nuclei themselves, but also degenerating neuronal projections to the cortex may account for the observed cognitive deficits in FRDA.
In order to assess the impact of disease-related variables on cognitive outcome, a summary score was computed taking into account only those measures of executive functions and attention which are not based on fast motor responses and do not correlate with articulation. Age at disease onset, GAA1 repeat length and disease severity as assessed with the SARA scale were associated with the executive score, while no correlation was found with age at the time of the investigation, education or disease duration. In a regression analysis, higher age at disease onset predicted better cognitive performance. Finally, age of onset was also identified as a good predictor for a very favourable outcome in a ROC analysis. Results of the present investigation are in line with earlier studies showing that age of onset is a critical factor. These studies suggest that FRDA has a negative impact on the development of motor cognition [17, 22], independent of the effect of disease duration. Results of the present study extend these findings showing that performance in tasks tapping attentional and executive functions is best predicted by the age at disease onset. Note, however, that age of onset is highly correlated with repeat length of the shorter allele and SARA score which are also important disease variables.
Results of the present study suggest that patients with FRDA generally have a good cognitive outcome when disease onset is later than 14 years. This finding may have important implications for patient counselling regarding education and career choices. Further studies with larger patient samples are needed in order to draw firm conclusions on the cognitive resources and on the risk of neuropsychological impairments in FRDA patients. Furthermore, follow-up studies could shed light on the development of cognitive abilities over time and differentiate between problems in the development of specific abilities due to FRDA and the deleterious effect of FRDA over longer time periods.
Notes
As not all outcome measures were normally distributed an additional analysis using nonparametric methods (Mann–Whitney U test) was performed and confirmed significant results.
A second summary score was calculated where each task contributed one point (alertness, divided attention, verbal fluency, Stroop, Tower of London). This second score (where all domains had the same weight) yielded exactly the same results in correlation and regression analyses.
The medians of patients’ RTs were 321 msec in alertness without warning, 320 msec in alertness with warning, 601 msec in divided attention (tones) and 577 msec in divided attention (visual stimuli).
No correlation was found between differences in naming time and measures of articulation speed (syllable repetition, reading test).
Note that deficits in auditory or visual perception cannot account for failures in the attention tasks as patients were able to discriminate the stimuli in the practise items of attention tasks.
References
Pandolfo M. Friedreich's ataxia: clinical aspects and pathogenesis. Semin Neurol. 1999;19:311–21.
Wollmann T, Barroso J, Monton F, Nieto A. Neuropsychological test performance of patients with Friedreich's ataxia. J Clin Exp Neuropsychol. 2002;24:677–86.
Botez MI, Leveille J, Lambert R, Botez T. Single photon emission computed tomography (SPECT) in cerebellar disease: cerebello-cerebral diaschisis. Eur Neurol. 1991;31:405–12.
Botez-Marquard T, Botez MI. Cognitive behavior in heredodegenerative ataxias. Eur Neurol. 1993;33:351–7.
Ciancarelli I, Cofini V, Carolei A. Evaluation of neuropsychological functions in patients with Friedreich ataxia before and after cognitive therapy. Funct Neurol. 2010;25:81–5.
Nieto A, Correia R, De NE, Monton F, Hess S, Barroso J. Cognition in Friedreich ataxia. Cerebellum. 2012;11:834–44.
Campuzano V, Montermini L, Molto MD, Pianese L, Cossee M, Cavalcanti F, et al. Friedreich's ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–7.
Schöls L, Amoiridis G, Przuntek H, Frank G, Epplen JT, Epplen C. Friedreich's ataxia. Revision of the phenotype according to molecular genetics. Brain. 1997;120(Pt 12):2131–40.
Bidichandani SI, Ashizawa T, Patel PI. The GAA triplet-repeat expansion in Friedreich ataxia interferes with transcription and may be associated with an unusual DNA structure. Am J Hum Genet. 1998;62:111–21.
Patel PI, Isaya G. Friedreich ataxia: from GAA triplet-repeat expansion to frataxin deficiency. Am J Hum Genet. 2001;69:15–24.
Bradley JL, Blake JC, Chamberlain S, Thomas PK, Cooper JM, Schapira AH. Clinical, biochemical and molecular genetic correlations in Friedreich's ataxia. Hum Mol Genet. 2000;9:275–82.
Schmucker S, Puccio H. Understanding the molecular mechanisms of Friedreich's ataxia to develop therapeutic approaches. Hum Mol Genet. 2010;19:R103–10.
Koeppen AH. Friedreich's ataxia: pathology, pathogenesis, and molecular genetics. J Neurol Sci. 2011;303:1–12.
Koeppen AH, Morral JA, Davis AN, Qian J, Petrocine SV, Knutson MD, et al. The dorsal root ganglion in Friedreich's ataxia. Acta Neuropathol. 2009;118:763–76.
Corben LA, Georgiou-Karistianis N, Fahey MC, Storey E, Churchyard A, Horne M, et al. Towards an understanding of cognitive function in Friedreich ataxia. Brain Res Bull. 2006;70:197–202.
White M, Lalonde R, Botez-Marquard T. Neuropsychologic and neuropsychiatric characteristics of patients with Friedreich's ataxia. Acta Neurol Scand. 2000;102:222–6.
Corben LA, Akhlaghi H, Georgiou-Karistianis N, Bradshaw JL, Egan GF, Storey E, et al. Impaired inhibition of prepotent motor tendencies in Friedreich ataxia demonstrated by the Simon interference task. Brain Cogn. 2011;76:140–5.
Klopper F, Delatycki MB, Corben LA, Bradshaw JL, Rance G, Georgiou-Karistianis N. The test of everyday attention reveals significant sustained volitional attention and working memory deficits in Friedreich ataxia. J Int Neuropsychol Soc. 2011;17:196–200.
Corben LA, Georgiou-Karistianis N, Bradshaw JL, Hocking DR, Churchyard AJ, Delatycki MB. The Fitts task reveals impairments in planning and online control of movement in Friedreich ataxia: reduced cerebellar-cortico connectivity? Neuroscience. 2011;192:382–90.
De Nobrega E, Nieto A, Barroso J, Monton F. Differential impairment in semantic, phonemic, and action fluency performance in Friedreich's ataxia: possible evidence of prefrontal dysfunction. J Int Neuropsychol Soc. 2007;13:944–52.
Mantovan MC, Martinuzzi A, Squarzanti F, Bolla A, Silvestri I, Liessi G, et al. Exploring mental status in Friedreich's ataxia: a combined neuropsychological, behavioral and neuroimaging study. Eur J Neurol. 2006;13:827–35.
Corben LA, Delatycki MB, Bradshaw JL, Churchyard AJ, Georgiou-Karistianis N. Utilisation of advance motor information is impaired in Friedreich ataxia. Cerebellum. 2011;10:793–803.
Hart RP, Kwentus JA, Leshner RT, Frazier R. Information processing speed in Friedreich's ataxia. Ann Neurol. 1985;17:612–4.
Fehrenbach RA, Wallesch CW, Claus D. Neuropsychologic findings in Friedreich's ataxia. Arch Neurol. 1984;41:306–8.
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–20.
Lynch DR, Farmer JM, Tsou AY, Perlman S, Subramony SH, Gomez CM, et al. Measuring Friedreich ataxia: complementary features of examination and performance measures. Neurology. 2006;66:1711–6.
Schmitz-Hübsch T, Giunti P, Stephenson DA, Globas C, Baliko L, Sacca F, et al. SCA Functional Index: a useful compound performance measure for spinocerebellar ataxia. Neurology. 2008;71:486–92.
Subramony SH, May W, Lynch D, Gomez C, Fischbeck K, Hallett M, et al. Measuring Friedreich ataxia: interrater reliability of a neurologic rating scale. Neurology. 2005;64:1261–2.
Trauzettel-Klosinski S, Dietz K. Standardized assessment of reading performance: the New International Reading Speed Texts IReST. Invest Ophthalmol Vis Sci. 2012;53:5452–61.
Lehrl S, Merz J, Burkard G, Fischer B. Mehrfachwahl-Wortschatz Intelligenz Test. Erlangen: Peri-Med Fachbuch; 1991.
Zimmermann P, Fimm B. Testbatterie zur Aufmerksamkeitsprüfung. Version 2.1. Psytest: Herzogenath; 2007.
Aschenbrenner S, Tucha O, Lange KW. Regensburger Wortflüssigkeits-Test. Göttingen: Hogrefe; 2001.
Kohler J&BU. Der Planungstest - Softwareprogramm zur Diagnostik von Planungsstörungen. In: EnJoiME Software (Beck & Kohler GbR), 78467 Konstanz: 2004.
Bäumler G. Farbe-Wort-Interferenztest (FWIT). Göttingen Toronto Zürich: Hogrefe; 1985.
Härting C, Markowitsch HJ, Neufeld H, et al. Wechsler Gedächtnis-Test - Revidierte Fassung. Bern: Verlag Hans Huber; 2000.
Warrington EK, James M. The visual object and space perception battery VOSP. Bury St. Edmunds: Thames Valley Test Company; 1991.
Helmstaedter C, Durwen HF. The verbal learning and retention test. A useful and differentiated tool in evaluating verbal memory performance. Schweiz Arch Neurol Psychiatr. 1990;141:21–30.
E KH, Chen SH, Ho MH, Desmond JE. A meta-analysis of cerebellar contributions to higher cognition from PET and fMRI studies. Hum Brain Mapp. 2012. doi:10.1002/hbm.22194.
Schmahmann JD, Caplan D. Cognition, emotion and the cerebellum. Brain. 2006;129:290–2.
Kuper M, Dimitrova A, Thurling M, Maderwald S, Roths J, Elles HG, et al. Evidence for a motor and a non-motor domain in the human dentate nucleus—an fMRI study. Neuroimage. 2011;54:2612–22.
Thurling M, Kuper M, Stefanescu R, Maderwald S, Gizewski ER, Ladd ME, et al. Activation of the dentate nucleus in a verb generation task: a 7T MRI study. Neuroimage. 2011;57:1184–91.
Dum RP, Strick PL. An unfolded map of the cerebellar dentate nucleus and its projections to the cerebral cortex. J Neurophysiol. 2003;89:634–9.
Granziera C, Schmahmann JD, Hadjikhani N, Meyer H, Meuli R, Wedeen V, et al. Diffusion spectrum imaging shows the structural basis of functional cerebellar circuits in the human cerebellum in vivo. PLoS One. 2009;4:e5101.
Akhlaghi H, Corben L, Georgiou-Karistianis N, Bradshaw J, Storey E, Delatycki MB, et al. Superior cerebellar peduncle atrophy in Friedreich's ataxia correlates with disease symptoms. Cerebellum. 2011;10:81–7.
Della NR, Ginestroni A, Diciotti S, Salvatore E, Soricelli A, Mascalchi M. Axial diffusivity is increased in the degenerating superior cerebellar peduncles of Friedreich's ataxia. Neuroradiology. 2011;53:367–72.
Conflicts of Interest
The authors have no conflicts of interest to disclose. WN, AE and SB are part of the European Friedreich's Ataxia Consortium for Translational Studies (EFACTS) which is funded by an FP7 Grant from the European Commission (HEALTH-F2-2010-242193).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nachbauer, W., Bodner, T., Boesch, S. et al. Friedreich Ataxia: Executive Control Is Related to Disease Onset and GAA Repeat Length. Cerebellum 13, 9–16 (2014). https://doi.org/10.1007/s12311-013-0513-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-013-0513-8