Abstract
Sleep disorders are common complaints in patients with neurodegenerative diseases such as spinocerebellar ataxia type 3 (SCA3) or Machado–Joseph disease (MJD)—SCA3/MJD. We evaluated the frequency of sleep disorders in SCA3/MJD patients against controls matched by age and gender, and correlated data with demographic and clinical variables. The main sleep disorders evaluated were rapid eye movement (REM) sleep behavior disorder (RBD), restless leg syndrome (RLS), and excessive daytime sleepiness (EDS). We recruited 40 patients with clinical and molecular-proven SCA3/MJD and 38 controls. We used the following clinical scales to evaluate our primary outcome measures: RBD Screening Questionnaire, International RLS Rating Scale, and Epworth Sleepiness Scale. To evaluate ataxia-related motor and non-motor features, we applied the International Cooperative Ataxia Rating Scale, the Scale for the Assessment and Rating of Ataxia, and the Unified Parkinson’s Disease Rating Scale part III. Psychiatric manifestations were tested with the Hamilton Anxiety Scale, and Beck Depression Inventory. The frequency of RBD and RLS were significantly higher in the SCA3/MJD group than in the control group (p < 0.001). There was no difference between both groups with regard to EDS. The accuracy of RDBSQ to discriminate between cases and controls was considered the best area under the ROC curve (0.86). Within-SCA3/MJD group analysis showed that anxiety and depression were significantly correlated with RDB, but not with RLS. Additionally, depression was considered the best predictive clinical feature for RDB and EDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinocerebellar ataxia type 3 (SCA3) or Machado–Joseph disease (MJD)—SCA3/MJD is the most common autosomal dominant subtype of ataxia worldwide [1]. Its clinical spectrum has a large variability, and recent clinical data has demonstrated high incidence of non-motor symptoms in SCA3/MJD, which include cognitive and psychiatry disturbances, olfactory dysfunction, and sleep disorders [2]. Few studies, however, have evaluated the frequency of these sleep disorders in larger series of molecular-proven SCA3/MJD patients [3–5], and even fewer studies compared these data with healthy controls [6]. The available evidence shows a greater frequency of sleep complaints in SCAs than in other neurodegenerative diseases [7–11]. Also, they have been considered an important modifier of health-related quality of life in SCA [6]. The frequently reported sleep complaints in SCA3/MJD include restless legs syndrome (RLS) [3], rapid eye movement (REM) sleep behavior disorder (RBD) [12], excessive daytime sleepiness (EDS) [12], sleep apnea [6], and insomnia [6]. Interestingly, not only these sleep disorders might be a frequent non-motor symptom in SCA3/MJD, but may also precede the onset of motor symptoms [5, 9, 13].
The present study aimed to re-test the hypothesis of whether or not a subset of sleep disorders are more frequent in a group of molecular-proven SCA3/MJD patients compared to age- and gender-matched controls. Additionally, we evaluated the discriminative threshold of these sleep disorders to differentiate between controls and cases, and their possible predictive values.
Patients and Methods
Subjects and Clinical Protocol
We evaluated 40 patients with clinical and molecular-proven SCA3/MJD. The control group was matched by age and gender, and consisted of 38 healthy subjects (HCS) with no family members with SCA3/MJD. Controls shared the same social background and had no significant medical history. Medications known to induce any sleep effect, such as tricyclic antidepressants, selective serotonine reuptake inhibitors, antidepressants, benzodiazepines, other sleep-induced medications, and anticholinergic drugs were all discontinued at least 1 month before clinical evaluation. Therefore, medications influencing sleep quality were taken. The study was approved by our Institutional Review Board and all subjects who agreed to participate signed a written informed consent. All subjects underwent thorough clinical and neurological examinations. The demographic variables studied included: gender, age at disease onset, age at disease evaluation, and disease duration. We also used the following clinical scales to assess the SCA3/MJD group: International Cooperative Ataxia Rating Scale, Brazilian-translated and -validated Scale for the Assessment and Rating of Ataxia [14, 15], Unified Parkinson's Disease Rating Scale part III, Hamilton Anxiety Scale (HAM-A), and Beck Depression Inventory (BDI). The number of CAG(n) expansions was also recorded.
Primary Outcome Measures
To evaluate the frequency and severity of sleep disorders in the SCA3/MJD group (primary outcome measures) compared to age- and gender-matched HCS, the following clinical scales were applied: RBD Screening Questionnaire (RBDSQ) [16], International RLS Rating Scale (IRLSRS) [17], and Epworth Sleepiness Scale (ESS). The diagnosis and severity of RBD was based on the RBDSQ using a five-point scale. Those who fulfilled the criteria of the five questions were considered to have clinically defined RBD [16]. We applied the ESS evaluating the previous 30 days. Three patients of the HCS group were excluded due to sleep deprivation (night shift work). The presence or not of RLS was based on a clinical face-to-face interview following recommended procedures [18]. The severity of RLS was measured using the IRLSRS, which was translated and validated into Brazilian Portuguese.
Statistical Analysis
Normal distribution of data was confirmed using the Kolmogorov–Smirnov test. Comparisons between groups were carried out using a two-tailed unpaired Student's t test for parametric data and the Mann–Whitney test for non-parametric data. The chi-square test or Fisher's exact test was used to evaluate categorical variables. The Receiver Operating Characteristic (ROC) test was performed to determine the best discrimination thresholds (accuracy) between controls and cases of the primary outcome measures in the study. Multiple regression analysis models were used to determine predictive values associated to the primary outcome measures. A corrected p value of 0.05 was set for the statistical analysis.
Results
Between-Group Analysis
There were no differences between the SCA3/MJD and HCS groups with regard to age at evaluation (p = 0.086) and gender (p = 0.816; 50% of males in the control group vs. 47.4% in the SCA3/MJD group). Based on the primary outcome measures there were no significant differences regarding EDS (p = 0.976), although a significantly greater frequency of RLS (p < 0.001) and RBD (p < 0.001) was found in the SCA3/MJD group as shown in Table 1.
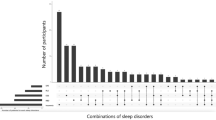
ROC analysis between case-controls showed that the area under the curve (AUC) was greater in RBD (0.86; standard error [SE] = 0.04; p < 0.001) as compared to RLS (0.70; SE = 0.06; p = 0.003) and EDS (0.50; SE = 0.07; p = 0.976). Hence, RBD was the best variable to accurately discriminate between patients with SCA3/MJD and controls. The AUC for RLS also showed asymptotic significance (Fig. 1).
Within-Group Analysis
Since we did not find any significant differences with regard to EDS between SCA3/MJD and HCS groups, within-group SCA correlation analysis was performed taking into account RLS and RBD as the main outcome variables.
With regard to RBD we found significant correlations between patients with greater RDB frequency and RLS (p = 0.011), EDS (p = 0.026), BDI (p = 0.038), and HAM-A (p = 0.012). As for RLS, we only found significant correlations between patients with greater RLS frequency and disease duration (p = 0.025) and RBD (p < 0.001; Table 2).
The multiple linear regression analysis showed that BDI was the best predictor for EDS (r 2 = 0.47; p = 0.02). Significant predictive variables (r 2 = 0.51) for RLS were RBD (p = 0.009) along with Unified Parkinson’s Disease Rating Scale (UPDRS)-III (p = 0.025). The only significant predictive variable for RBD was BDI (r 2 = 0.53; p = 0.001).
Discussion
Our study confirms a clear significant greater frequency of a subset of sleep disorders in a group of clinical and molecular-proven SCA3/MJD patients as compared to age- and gender-matched HCS. However, we did not find a significantly higher frequency of EDS. Additionally, anxiety and depression were significantly correlated with the frequency of RBD suggesting that sleep disorders in these patients might be influenced much more by non-motor, psychiatric manifestations than ataxia-related motor features.
The available evidence shows that the frequency of RLS in SCAs is significantly greater than in the general population ranging from 20% to 30% [4]. When SCA3/MJD patients are considered, the frequency rates of RLS are even greater, reaching up to 55% [3, 19]. In our series, we found a significant higher frequency of RLS in SCA3/MJD patients as compared to controls (p < 0.001), which is consistent with the literature data. In view of the “dopaminergic hypothesis” that proposes that RLS could reflect basal ganglia dysfunction [4], we tested whether or not Parkinsonian symptoms could correlate to RLS, but this correlation was not significant. On the other hand, the severity of RLS had a significant positive correlation with disease duration, suggesting that the longer the disease the more severe RLS symptoms are.
Similarly to RLS, RBD is also more common in SCA3/MJD patients than in the general population [6]. Indeed our data is consistent with the literature showing a significantly greater frequency of RBD in the SCA3/MJD group (p < 0.01). The underlying involvement of midbrain cholinergic and pontine noradrenergic systems seen in SCA3/MJD patients could in part explain these higher rates of RBD [2]. Sleep-related movement disorders, particularly RBD, are traditionally and frequently seen in synucleinopathies such as Parkinson's disease and multiple system atrophy [20]. Additionally, the pathophysiology of either Parkinsonian features or RBD is known to be closely related to a “dopaminergic system dysfunction” [5, 20]. However, we did not find any correlation in our study. When ROC analysis was performed RBD was found to be the best clinical variable to accurately discriminate between patients with SCA3/MJD and controls in our study.
EDS have been documented not only in SCA3 patients, but also in other SCA-subtypes such as SCA1 [6, 12, 21]. A recent case-control study in SCA3 patients using the ESS to assess EDS also reported a very similar result to ours. The ESS score was 8.71 ± 5.2 in the SCA3/MJD vs. 7.48 ± 4.15 in controls without significant differences. However, 45% of these patients had scores > 10 vs. 29.2% of controls (p = 0.05) [6].
A large body of evidence has shown higher rates of neuropsychiatric symptoms such as depression and anxiety in SCA3/MJD patients than in the general population [13, 22, 23]. However, it is not yet clearly understood the exact frequency of these psychiatric manifestations, their differences among SCA-subtypes [24], and whether or not they could influence sleep disorder outcome. A large series involving 76 subjects with different SCA-subtypes (SCA 1,2, 3, and 6) found that depressive symptoms were significantly greater in SCA3 patients as compared to other SCA-subtypes, accounting for 60% of cases [24]. Additionally, a significant positive correlation has also been found between BDI scores and motor incapacitation in SCA3/MJD patients (r p = 0.51; p < 0.0001) [22]. Although several data have demonstrated a clear positive relationship between BDI scores and disease severity [25], their correlation with sleep disorders remains unclear. We speculate that depression in SCA3/MJD is likely multifactorial with complex pathophysiology. Functional neuroimaging studies might help understand the exact correlation between high scores of depression and RBD in some SCA3/MJD patients since they have been shown to have a dopaminergic dysfunction [26]. In other diseases with dopaminergic dysfunction, like Parkinson's disease, PET studies have demonstrated reduction of 5-HT1A receptor binding in the limbic cortex and frontal and temporal cortical areas in depressed patients, suggesting that depression might be associated with a specific loss of dopamine and noradrenalin innervation in the limbic system [27].
There are several limitations that should be noted in our study. First, although the IRLSRS has been validated to Portuguese, some SCA3/MJD patients have peripheral neuropathy whose symptoms, together with those of RLS, may yield greater severity scores. Therefore, there may have been an overestimation of RLS frequency rates. Second, we used the UPDRS part III to grade Parkinsonian signs, but we are aware that this scale was not originally developed to evaluate Parkinsonian signs in SCA patients. We also used a questionnaire to evaluate RBD but this approach may increase false-positive diagnostic rates. Finally, an electrophysiological analysis of peripheral nerves was not performed in the SCA3/MJD group. Since neuropathy is a common clinical feature in these patients, we might have misdiagnosed some cases of RLS who were actually patients suffering from neuropathy.
In conclusion, our study confirms a significantly greater frequency of sleep disorders in patients with SCA3/MJD, notably RLS and RBD, and points out that ataxia-related non-motor features such as depression and anxiety may be important variables and should be carefully evaluated in these patients.
References
Schols L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004;3:291–304.
Rüb U, Brunt ER, Deller T. New Insights into the pathoanatomy of spinocerebellar ataxia type 3 (Machado Joseph disease). Curr Opin Neurol. 2008;21:111–16.
Schols L, Haan J, Riess O, Amoiridis G, Przuntek H. Sleep disturbance in spinocerebellar ataxias—is the SCA 3 mutation a cause of restless legs syndrome? Neurology. 1998;51:1603–07.
Reimold M et al. Spinocerebellar ataxia type 1, 2 and 3 and restless legs syndrome: striatal dopamine D2 receptor status investigated by [11C]raclopride positron emission tomography. Mov Disord. 2006;21:1667–73.
D'Abreu A, Friedman J, Coskun J. Non-movement disorder heralds symptoms of Machado Joseph disease years before ataxia. Mov Disord. 2005;20:739–41.
D'Abreu A, França Jr M, Conz L, et al. Sleep symptoms and their clinical correlates in Machado–Joseph disease. Acta Neurol Scand. 2009;119:277–80.
Iranzo A, Munoz E, Santamaria J, et al. REM sleep behavior disorder and vocal cord paralysis in Machado–Joseph disease. Mov Disord. 2003;18:1179–83.
Iranzo A. Sleep and breathing in multiple system atrophy. Curr Treat Options Neurol. 2007;9:347–53.
Schols L, Linnermann C, Globas C. Electrophysiology in spinocerebellar ataxias: spread of disease and characteristic findings. Cerebellum. 2008;7:198–03.
Vecchierini MF. Sleep disturbances in Alzheimer's disease and other dementias. Psychol Neuropsychiatr Vieil. 2010;8:15–23.
Videnovic A, Leurgans S, Fan W, Jaglin J, Shannon KM. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15:471–74.
Friedman JH, Fernandez HH, Sudarsky LR. REM behavior disorder and excessive daytime somnolence in Machado–Joseph disease (SCA-3). Mov Disord. 2003;18:1520–22.
D'Abreu A, França Jr MC, Paulson HL, Lopes-Cendes I. Caring for Machado Joseph disease: current understanding and how to help patients. Parkinsonism Relat Disord. 2010;16:2–7.
Braga-Neto P, Godeiro-Junior C, Dutra LA, Pedroso JL, Barsottini OGP. Translation and validation into Brazilian version of the Scale of the Assessment and Rating of Ataxia (SARA). Arq Neuropsiquiatr. 2010;68:228–30.
Schmitz-Hubsch T et al. Scale for the assessment and rating of ataxia—development of a new clinical scale. Neurology. 2006;66:1717–20.
Stiasny-Kolster K, Mayer G, Schafer S, et al. The REM sleep behavior disorder screening questionnaire – a new diagnostic instrument. Mov Disord. 2007;22:2386–93.
Masuko AH, Carvalho LB, Machado MA, et al. Translation and validation into the Brazilian Portuguese of the restless legs syndrome rating scale of the International Restless Legs Syndrome Study group. Arq Neuropsiquiatr. 2008;66:832–36.
Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome diagnosis and epidemiology workshop at the national institutes of health; international restless legs syndrome study group. restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19.
Iranzo A, Comella CL, Santamaria J, Oertel W. Restless legs syndrome in Parkinson's disease and other neurodegenerative diseases of the central nervous system. Mov Disord. 2007;22:424–30.
Frenette E. REM Sleep Behavior Disorder. Med Clin North Am. 2010;94:593–14.
Dang D, Cunnington D. Excessive daytime somnolence in spinocerebellar ataxia type 1. J Neurol Sci. 2010;290:146–47.
Cecchin CR, Pires AP, Rieder CR, et al. Depressive symptoms in Machado Joseph Disease (SCA3) patients and their relatives. Community Genet. 2007;10:19–26.
Kawai Y, Takeda A, Abe Y, et al. Cognitive impairments in Machado–Joseph disease. Arch Neurol. 2004;61:1757–60.
McMurtray AM, Clark DG, Flood MK, Perlman S, Mendez MF. Depressive and memory symptoms as presenting features of spinocerebellar ataxia. J Neuropsychiatry Clin Neurosci. 2006;18:420–22.
Saute JAM, Silva ACF, Donis KC, et al. Depressive mood is associated with ataxic and non-ataxic neurological dysfunction in SCA3 patients. Cerebellum. 2010;9(4):603–5. doi:10.1007/s12311-010-0205-6.
Yen T, Lu C, Tzen K, et al. Decreased dopamine transporter binding in Machado–Joseph disease. J Nucl Med. 2000;41:994–8.
Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain. 2005;128:1314–22.
Acknowledgments
Dr Andre C. Felicio is supported by a doctorate fellowship grant from the “Fundação de Amparo à Pesquisa de São Paulo” (FAPESP). Dr. Gilmar F. Prado is partially supported by the “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq).
Conflict of interest
We have no conflicts of interest.
Protection of Human Research Subjects and Human Subject Informed Consent
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national). All subjects were provided with the approved informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedroso, J.L., Braga-Neto, P., Felício, A.C. et al. Sleep Disorders in Machado–Joseph Disease: Frequency, Discriminative Thresholds, Predictive Values, and Correlation with Ataxia-Related Motor and Non-Motor Features. Cerebellum 10, 291–295 (2011). https://doi.org/10.1007/s12311-011-0252-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-011-0252-7