Abstract
Purpose
Rotator cuff (RC) disease is frequent and represents a common source of shoulder pain. The aim of this study is to analyse geographical differences in RC surgeries from 2001 to 2014 in Italy, a country with universal and free health care for its population.
Methods
An analysis of the Italian National Hospital Discharge records from 2001 to 2014 was performed. These data are anonymous and include patient’s age, sex, domicile, region of hospitalization, length of the hospitalization and type of reimbursement (public or private). National and regional population data were obtained from the National Institute for Statistics (ISTAT) for each year.
Results
During the 14-year study period, 390,001 RC repairs were performed in Italy, which represented a mean incidence of 62.1 RC procedures for every 100,000 Italian inhabitants. Nevertheless, the incidence was very different if every single regional population is considered individually. Lombardy resulted to have the highest number of surgeries during the 14-year study period, with 27.95% (108,954) of the total national procedures performed in the 2001–2014 time span. More than half the surgeries (52.00%) were performed in only 3 regions of the northern part of Italy.
Conclusions
This study shows the existence of geographical disparities in access to RC surgery and patients’ necessity to migrate among regions in order to obtain it. Southern regions of Italy are characterized by a lower number of surgeries compared to the northern part of Italy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotator cuff (RC) disease is frequent and represents a common source of shoulder pain [1, 2]. Each year in the USA, approximately 4.5 million patient visits related to shoulder pain occur, and the majority of them are due to RC problems [3, 4].
Patients with RC pathology may complain of symptoms ranging from minimal discomfort without functional deficits to severe pain, weakness and marked disability [5, 6]. Surgical repair of RC tears is a well-documented therapeutic option in these patients [7,8,9,10,11].
Geographical variation in the number of RC surgical procedures performed in the USA and variations in what surgeons deemed to be indications for RC surgery has been studied [12, 13]. Several reports have highlighted the apparent broadening of indications for RC surgery [12, 14,15,16], showing a considerable variation in the treatment of RC disease and the conditions requiring surgical repair. Incidence of RC surgery is rapidly increasing in selected patient cohorts [17], but nationwide incidence rates have been reported only for Finland [18] and Italy [19].
One of the founding principles of the Italian National Health Service (NHS) is fairness in access to health care, being free to every patient at the point of use.
Data from the Italian registry showed that 68.1% of RC repairs were performed in the North from 2001 to 2014, 19.1% in the Centre and 12.8% in the South. Data on domicile of the patient showed that 63.3% patients undergoing RC repairs came from the North, 20.2% from the Centre and 16.5% from the South and Islands. These data implicated significant differences in incidence of operations. Considering the Italian population of the 3 different regions of Italy (North, Centre and South), from 2001 to 2014, the incidence of operations was 77.7 per 100,000 person-years in the North, 35.5 per 100,000 person-years in the Centre, and 22.2 per 100,000 person-years in the South. [19].
This study aimed to explore geographical variation in equity in access to RC surgery among regions of Italy from 2001 to 2014, based on the official information source of hospitalization records provided by the Italian Ministry of Health.
Materials and Methods
An analysis of the National Hospital Discharge records (SDO) maintained at the Italian Ministry of Health concerning the 14 years of our survey (2001 through 2014) was performed. This archive collects information concerning all hospitalizations occurring in Italian public and private care settings. These data are anonymous and include patient’s age, sex, domicile, region of hospitalization, length of hospitalization and type of reimbursement (public or private). National and regional population data were obtained from the National Institute for Statistics (ISTAT) for each year. RC repair was defined by the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) major diagnosis code: 83.63 (rotator cuff repair).
Epidemiology of RC repairs based on Italian geographical macroregions has already been reported [19]. This article reports details of patients’ domicile, region of hospitalization and region where the surgery was performed. These data aim to highlight potential disparities in access to health care in Italy and patients’ necessity to migrate among regions in order to obtain it.
We distinguished patients by their regional domicile, thus defining them “regional populations”. Moreover, we distinguished for each region the origin of patients who underwent surgery. Procedures performed on patients residing in the same region of hospitalization were defined as “regional surgeries”. Procedures performed on patients not residing in the same region of hospitalization were defined “extra-regional surgeries”.
Descriptive statistics was performed.
Results
Demographics
During the 14-year study period, 390,001 RC repairs were performed in Italy, which represented a mean incidence of 62.1 RC procedures for every 100,000 Italian inhabitants. Nevertheless, the mean incidence is very different if every single regional population is considered individually.
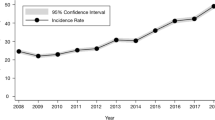
Of 390,001 RC repairs performed in Italy during the study period, patients’ domicile data were not available for 244 RC repairs, thus resulting in a total of 389,757 RC repairs for which patients’ domicile data were available (Table 1). Only 5 over 21 regional populations (Patients from Aosta Valley, Veneto, Lombardy, Autonomous Province of Trento and Emilia Romagna) had an incidence greater than the national one. Seven over 21 regional populations (Patients from Basilicata, Molise, Apulia, Calabria, Sicily, Sardinia, Campania) had less than half the incidence than the national one. Patients from Campania resulted to be the ones with the lowest incidence of RC repair in Italy (13.39 RC procedures for every 100,000 inhabitants). Further details about the incidence of surgeries performed for each regional population are reported in Fig. 1 and Table 2.
Region of hospitalization and domicile of the patients
Regarding regional distribution of surgeries, the majority of patients underwent surgery in their own region of domicile. Lombardy resulted to have the highest number of surgeries during the 14-year study period, with 27.95% (108,954) of the total national procedures performed in the 2001–2014 time span. More than half the surgeries (52.00%) were performed in only 3 regions of northern Italy (Lombardy, Emilia Romagna, Veneto). Lombardy also performed the highest number of extra-regional surgeries (19,791). Umbria resulted instead the region with the highest percentage of extra-regional surgeries (47.7%). Patients from the Autonomous Province of Bolzano resulted to be the only regional population from the Northern part of Italy to have an incidence of RC repair below the national one. Further details about the number of surgeries performed in each region are reported in Fig. 2. A number of regional and extra-regional surgeries are reported in Fig. 2 and Table 2. Specifics on regional migration in the 2001–2014 time span are summarized in Table 1.
Discussion
The most important finding from our registry study is that severe geographical variations in RC repair rates were present among regions of Italy. The majority of RC procedures were performed in the northern part of Italy, with more than half the surgeries (52.00%) performed in only 3 regions (Lombardy, Emilia Romagna, Veneto).
Regions from the southern part of Italy were characterized both by a lower number of regional and extra-regional surgeries. Regional populations of the southern regions of Italy had significantly lower rate of surgeries per 100.000 inhabitants compared to the ones of the northern part of Italy. Patients from Campania resulted to be by far the ones with the lowest incidence in Italy.
Oddly, patients from the Autonomous Province of Bolzano resulted to be the only regional population from the Northern part of Italy to have an incidence of RC repair below the national one: this may reveal an international migration of such patients to the adjoining Austria and Switzerland.
It is not possible to discriminate whether these differences reflect variations in need or in clinical practice because data on prevalence, incidence, severity of RC tears and information regarding clinicians’ and patients’ attitudes to RC surgery are not available [20]. They may also indicate differing amounts of resources available to provide RC surgery.
In view of the Government and the Italian Ministry of Health focus on reducing health inequalities, this massive difference in RC surgeries incidence among regions of Italy highlights a topic that absolutely needs further investigation.
It is possible that these differences reflect real geographical variation in need or patient consent to surgery. However, some studies have suggested that need is greater among the most deprived groups, and that education and income are unrelated to willingness to undergo surgery [21]. If so, this would imply inequity in the provision of RC surgery. A nationwide registry study in Finland showed higher incidence rate (from 44 to 131 per 100,000 adults per year) compared to rates in Italy [18].
This study has some limitations. It relied upon administrative data, and thus, there is the possibility that changes in coding practices could have impacted our results. That said, we are unaware of any systematic changes in the coding of RC repair that would have significantly impacted our findings. Significant regional variations were found in our study, confirming an inequity. This may express unmet needs in the low RC repair rate areas, or else over-indication in the high RC repair rate areas. So, part of this variability may be related to patients and to surgeons, and this cannot be clarified from the database analysis.
Thirdly, a limitation of this registry study is that we are unable to evaluate potential inaccuracies in diagnoses or procedures coding. Fourthly, the diagnosis and procedure coding used during the study period did not allow differentiation between open and arthroscopic procedures, or between partial and full-thickness tears. That said, this does not represent a major issue, since we focused in this article on geographical disparities in access to health care.
Conclusions
In conclusion, this study confirms the existence of a geographical disparity in access to health care and patients’ necessity to migrate among regions in order to obtain it. Regions from the southern part of Italy are characterized by a lower number of surgeries. Patients residing in southern regions of Italy had significantly lower incidence of surgeries compared to the ones of the northern part of Italy.
We found evidence of a concentration of RC procedures in the north of Italy. Our results give pause over whether efforts on regionalization of RC repair should turn towards improving quality in hospitals in the South of Italy. There is evidence of inequity in access to RC surgeries across macroregions of Italy. Today’s levels of RC surgery are below the expected maximum incidence, and we expect a continued annual increase in the total number of RC repair performed. Policy makers should examine factors to understand the determinants of inequitable provision.
References
Longo UG, Berton A, Ahrens PM, Maffulli N, Denaro V (2011) Clinical tests for the diagnosis of rotator cuff disease. Sports Med Arthrosc Rev 19(3):266–278. https://doi.org/10.1097/JSA.0b013e3182250c8b
Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS (2013) The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg 22(12):1628–1632. https://doi.org/10.1016/j.jse.2013.01.006
Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V (2012) Epidemiology, genetics and biological factors of rotator cuff tears. Med Sport Sci 57:1–9. https://doi.org/10.1159/000328868
Maffulli N, Longo UG, Berton A, Loppini M, Denaro V (2011) Biological factors in the pathogenesis of rotator cuff tears. Sports Med Arthrosc Rev 19(3):194–201. https://doi.org/10.1097/JSA.0b013e3182250cad
Longo UG, Vasta S, Maffulli N, Denaro V (2011) Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med Arthrosc Rev 19(3):310–320. https://doi.org/10.1097/JSA.0b013e31820af9b6
Longo UG, Margiotti K, Petrillo S, Rizzello G, Fusilli C, Maffulli N, De Luca A, Denaro V (2018) Genetics of rotator cuff tears: no association of col5a1 gene in a case-control study. BMC Med Genet. https://doi.org/10.1186/s12881-018-0727-1
Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V (2008) Soft tissue tenodesis of the long head of the biceps tendon associated to the Roman Bridge repair. BMC Musculoskelet Disord 9:78. https://doi.org/10.1186/1471-2474-9-78
Longo UG, Franceschi F, Spiezia F, Marinozzi A, Maffulli N, Denaro V (2011) The low-profile Roman bridge technique for knotless double-row repair of the rotator cuff. Arch Orthop Trauma Surg 131(3):357–361. https://doi.org/10.1007/s00402-010-1203-3
Longo UG, Lamberti A, Khan WS, Maffulli N, Denaro V (2011) Synthetic augmentation for massive rotator cuff tears. Sports Med Arthrosc Rev 19(4):360–365. https://doi.org/10.1097/JSA.0b013e318224e359
Franceschi F, Longo GU, Ruzzini L, Rizzello G, Maffulli N, Denaro V (2007) The Roman Bridge: a “double pulley-suture bridges” technique for rotator cuff repair. BMC Musculoskelet Disord. https://doi.org/10.1186/1471-2474-8-123
Longo UG, Berton A, Khan WS, Maffulli N, Denaro V (2011) Histopathology of rotator cuff tears. Sports Med Arthrosc Rev 19(3):227–236. https://doi.org/10.1097/JSA.0b013e318213bccb
Vitale MG, Krant JJ, Gelijns AC, Heitjan DF, Arons RR, Bigliani LU, Flatow EL (1999) Geographic variations in the rates of operative procedures involving the shoulder, including total shoulder replacement, humeral head replacement, and rotator cuff repair. J Bone Joint Surg Am 81(6):763–772
Mall NA, Lee AS, Chahal J, Sherman SL, Romeo AA, Verma NN, Cole BJ (2013) An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy 29(2):366–376. https://doi.org/10.1016/j.arthro.2012.06.024
Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, Marx RG (2005) Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am 87(9):1978–1984. https://doi.org/10.2106/JBJS.D.02944
Mauro CS, Jordan SS, Irrgang JJ, Harner CD (2012) Practice patterns for subacromial decompression and rotator cuff repair: an analysis of the American Board of Orthopaedic Surgery database. J Bone Joint Surg Am 94(16):1492–1499. https://doi.org/10.2106/JBJS.J.01696
Wolf BR, Dunn WR, Wright RW (2007) Indications for repair of full-thickness rotator cuff tears. Am J Sports Med 35(6):1007–1016. https://doi.org/10.1177/0363546506295079
Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ (2014) Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 96-B(1):70–74. https://doi.org/10.1302/0301-620x.96b1.32556
Paloneva J, Lepola V, Äärimaa V, Joukainen A, Ylinen J, Mattila VM (2015) Increasing incidence of rotator cuff repairs—a nationwide registry study in Finland. BMC Musculoskelet Disord 16:189. https://doi.org/10.1186/s12891-015-0639-6
Longo UG, Salvatore G, Rizzello G, Berton A, Ciuffreda M, Candela V, Denaro V (2016) The burden of rotator cuff surgery in Italy: a nationwide registry study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-016-2610-x
Randelli P, Arrigoni P, Cabitza F, Ragone V, Cabitza P (2012) Current practice in shoulder pathology: results of a web-based survey among a community of 1,084 orthopedic surgeons. Knee Surg Sports Traumatol Arthrosc 20(5):803–815. https://doi.org/10.1007/s00167-011-1673-z
Chaturvedi N, Ben-Shlomo Y (1995) From the surgery to the surgeon: does deprivation influence consultation and operation rates? Br J Gen Pract 45(392):127–131
Acknowledgments
We thank the Direzione Generale della Programmazione Sanitaria—Banca Dati SDO of the Italian Ministry of Health for the support in providing data for this research.
Author information
Authors and Affiliations
Contributions
UGL and VD contributed to conceptualization; GS, AB and LRA were involved in data curation; GS was involved in formal analysis; VC and AB helped in methodology; UGL contributed to project administration; FM and SP were involved in software; UGL and VD helped in supervision; GS and UGL were involved in writing—original draft; and GS, UGL and VC were involved in writing—review and editing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salvatore, G., Longo, U.G., Candela, V. et al. Epidemiology of rotator cuff surgery in Italy: regional variation in access to health care. Results from a 14-year nationwide registry. Musculoskelet Surg 104, 329–335 (2020). https://doi.org/10.1007/s12306-019-00625-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-019-00625-y