Abstract
Background
Most of the information available about Legg–Calve–Perthes disease (LCPD) at present is gained through imaging modalities including plain radiographs and magnetic resonance imaging (MRI). But the accuracy of MRI in this disease and its predictive value to reveal various intra-articular pathologies is not known. We correlated the findings of MRI with those seen on hip arthroscopy in children with active stage of LCPD.
Methods
We conducted a prospective observational study in which MRI findings were correlated with corresponding findings on hip arthroscopy in a cohort of 25 patients of active LCPD below 12 years of age. The parameters noted on MRI included status of ligamentum teres, status of the labrum, synovial effusion if any, condition of the femoral and acetabular articular cartilage including chondral flaps, chondral indentation and intra-articular loose bodies. The indication of performing hip arthroscopy was persistent severe hip pain (Wong–Baker FACES pain scale ≥ 3) after 6 months of conservative management. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated for MRI considering arthroscopy as a gold standard.
Results
Synovial effusion was seen in a large number of patients on both MRI (17) and hip arthroscopy (24). The sensitivity (95% confidence interval) of MRI was found to be low, especially with respect to labral tears [25% (0.63–80.6)] and intra-articular loose bodies [20% (0.51–71.6)]. NPV for synovial effusion was also found to be low [12.5% (0.32–52.7)], although specificity and PPV of MRI were found to be good for all the parameters.
Conclusions
MRI cannot be completely relied upon for identifying all the intra-articular pathologies in children with LCPD, although it has a good complimentary role. In patients with severe persistent pain with suspicion for joint changes, hip arthroscopy can provide a safe and efficient procedure (better than MRI) for eliciting the associated joint pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Legg–Calve–Perthes disease (LCPD) is a disabling disease of the hip in childhood affecting approximately 10.8 of every 100,000 children [1]. It is more common in males than in females in a ratio 5:1 [2]. The radiological changes in LCPD lag behind the symptoms, and X-ray is often normal in the early stages of the disease. To diagnose LCPD in such children, radionuclide bone scan and magnetic resonance imaging (MRI) have been described as useful entities [3, 4]. MRI has been propounded to have a particular value in identifying the early stages of LCPD in the absence of changes on plain films, as well as in cases where the differential diagnosis would otherwise be difficult. MRI is also said to be helpful in assessing revascularization, healing and multiple complications [5].
However, there is a shortage of data about the actual pathological changes in the hip joint during the active stage of the disease. As LCPD does not result in mortality, there is paucity of histopathological data as well. Most of the information available about LCPD at present is gained through imaging modalities including plain radiographs, MRI and magnetic resonance arthrography (MRA). But the accuracy of these radiological findings and their predictive value to reveal various intra-articular pathologies is not known. The correlation between investigative imaging and the actual pathology in the joint is a matter of debate. There are limited studies in the literature to test the accuracy and predictive values of various imaging modalities with respect to the true pathology in cases of LCPD. There is a need to validate the imaging modalities for LCPD by comparing their findings with the actual disease process. We tried to correlate the findings of hip arthroscopy in patients with active LCPD, which is supposed to tell the actual pathological changes in the joint, with the corresponding findings on MRI.
Materials and methods
We conducted a prospective observational study in which 25 consecutive patients with active LCPD were enrolled. In the study, a cohort of symptomatic children with diagnosed LCPD and age less than 12 years (any radiological stage), who were undergoing hip arthroscopy, was evaluated. The indication of performing hip arthroscopy was persistent severe hip pain (Wong–Baker FACES pain scale ≥ 3 [6]) after 6 months of conservative management. Hip arthroscopy was performed to look for any intra-articular pathology (in addition to the bony changes in LCPD) contributing to the resilient symptoms, as these patients had severe global restriction of hip joint movements suggesting intra-articular changes. At the time of performing hip arthroscopy, none of the studied patients were candidates for surgical management. Children who had already received any form of treatment for LCPD outside the institute or in whom there were contra-indications for taking MRI were excluded from the study.
After obtaining informed parental consent, detailed history was elicited and complete examination including general physical examination and local examination was done. Plain radiographs of the hip—both antero-posterior and frog-leg lateral views—were done for all the patients to aid in diagnosing the disease. All the patients underwent MRI under 3T MR scanner before hip arthroscopy. T1-weighted and T2-weighted sequences with fat saturation were obtained in coronal and sagittal planes using 3-mm slice thickness, 256 × 256 matrix. Image analysis was performed by a single dedicated musculoskeletal radiologist for each patient. The parameters noted on MRI included status of ligamentum teres [7], status of the labrum, synovial effusion if any, condition of the femoral and acetabular articular cartilage including chondral flaps, chondral indentation and intra-articular loose bodies. The diagnosis of LCPD was based on clinical findings, plain radiographs and MRI.
In all patients, pre-anaesthetic check-up was done and after obtaining anaesthetic fitness, arthroscopy of the hip was done in supine position under general anaesthesia on a fracture table, with the help of an image intensifier. All the hip arthroscopies were performed by the same surgeon. Traction was used to distract the joint by 10–15 mm for visualization. Anterolateral portal was established at the level of the tip of the greater trochanter and was directed through the gluteus medius musculature, entering the lateral part of the capsule. The central compartment was first seen with the hip joint in traction followed by visualizing the peripheral compartment after loosening the traction on the joint. During arthroscopy, a note was made of synovial proliferation, status of ligamentum teres, integrity of the acetabular labrum, loose bodies in the joint, chondral flaps, groove defects of the femoral head and status of the articular cartilage of both the femoral head and the acetabulum. The various therapeutic procedures performed included synovial biopsy and debridement, loose body removal, micro-fracture and joint lavage.
Data including name, age, sex, side involved, Catterall class, Herring group, de Sanctis class, MRI findings and corresponding arthroscopic findings were recorded on a prefixed proforma. Statistical analysis was then carried out using SPSS 20.0 software (IBM, Inc.). Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were then calculated for the various MRI findings considering the corresponding arthroscopic findings as the gold standard.
Results
Twenty-five consecutive patients were enrolled in the study. There were 21 boys and 4 girls. The mean age of the patients was 9.08 years with a range of 4–12 years. By Catterall classification [8], three patients were in Catterall stage 2, 16 patients were in Catterall stage 3 and six patients were in Catterall stage 4. Similarly, as per Herring lateral pillar classification [9], nine patients were in Herring group B and 16 patients were in Herring group C. On MRI of the hip, labral tear was visualized in one patient. Ligamentum teres pathology was not seen in any of the patients. Synovial effusion was seen in 17 patients. Loose body was seen in one patient, and there was no patient detected with a chondral flap or chondral indentation of the femoral head.
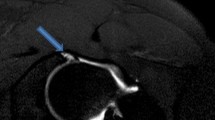
During arthroscopy of the hip, synovial proliferation was seen in all the patients except one. Labral tear was visualized in four patients. There were 11 patients with changes seen in the femoral head articular cartilage which included chondral flaps, chondral loose bodies and groove defects of the femoral head. One patient had 2 chondral flaps, and 4 other patients had one chondral flap each. Three patients had relatively severe defect of the femoral articular cartilage (Beck grade 2 [10]). Chondral loose bodies were seen in five patients. Ten patients had groove defects of the femoral head with indentation upon probing the cartilage. Acetabular cartilage changes were seen in two patients one of whom had pulvinar hyperaemia in the acetabulum. Three patients had degenerative ligamentum teres, and in one patient, the latter was not visualized. None of the patients had any complication after hip arthroscopy. Figure 1 shows the X-ray, MRI and arthroscopic picture in a 12-year-old child suffering from LCPD.
a Plain radiograph. X-ray pelvis with both hips—antero-posterior view of a 12-year-old child with Legg–Calve–Perthes disease of the right hip showing fragmentation and sclerosis in the right femoral capital epiphysis with Catterall stage 3 and Herring group B. b Magnetic resonance imaging. MRI of the same patient showing synovial effusion in the right hip joint with cystic metaphyseal changes. c Arthroscopic picture. Hip arthroscopic picture of the same patient showing chondral loose body with inflamed synovium with groove defect of the femoral head with non-visualization of the ligamentum teres
In our study, considering arthroscopy as the gold standard for visualizing the intra-articular pathologies, the sensitivity of MRI was found to be quite low (Fig. 2). Similarly, NPV for detecting synovial effusion was quite low. The specificity and PPV, however, were very good. The sensitivity, specificity, PPV and NPV values for the various findings are illustrated in Table 1. Sensitivity and PPV could not be evaluated for detecting ligamentum teres pathology, chondral flaps and groove defects of the femoral head (chondral indentation) due to lack of any patient with these MRI findings.
Discussion
MRI is a very useful modality to visualize the early changes in the hip joint in cases of LCPD and also to differentiate it from other pathologies of the hip [5]. It has also been reported to help in staging and prognostication of the disease. However, whether MRI depicts the actual pathological process in the hip joint is not known with certainty. There is a shortage of data on comparison between MRI and the actual disease process in LCPD, which can be visualized well with arthroscopy.
Various studies published in the literature have mentioned about the comparison of magnetic resonance arthrography (MRA) with arthroscopy, mostly in adult patients with various pathologies of the hip [11,12,13,14]. Articular cartilage, acetabular labrum, ligamentum teres and chondral loose bodies are reported to be seen adequately with precision on MRA in such studies. However, there is no definite conclusion about the accuracy and predictive value of plain MRI with respect to arthroscopy. Moreover, there is no such study in children with LCPD. We resorted to conventional MRI in our study as synovial effusion was found to be present in most of our patients which provided with an arthrogram effect without actual instillation of the dye in the joint. Thus, the possible complications of the intra-articular contrast agent, for which the safety and efficacy have not been established in children, were bypassed.
In the study by Toomayan et al. [11] regarding acetabular labral tears, considering hip arthroscopy as the gold standard, sensitivity of conventional MRI with a small field of view to detect labral tears was 25%, that of conventional MRI with large field of view was 8% and that of MRA was 92%. The specificity was 100% for all three. In another study by Czerny et al. [12], the sensitivity of conventional MR imaging for detecting acetabular labral tears was 30% and its accuracy was 36%, whereas the sensitivity of MRA was 90% and its accuracy was 91%, compared with surgical findings. Our study also found low sensitivity for MRI, although the specificity was found to be good.
In another study by Mitchell et al. [13], sensitivity of MRA for detecting labral tears was 24% and specificity was 100%. Similarly, with respect to cartilage abnormalities, sensitivity was found to be 6% and specificity was 100%. In a study by Keeney et al. [14], with respect to labral pathology, MRA had a sensitivity of 71%, PPV of 93%, NPV of 12.9% and accuracy of 69%; the specificity, however, could not be accurately determined. With respect to articular cartilage abnormality, MRA showed a sensitivity of 47%, a specificity of 89%, a PPV of 84%, a NPV of 59% and an accuracy of 67%. These studies support the low sensitivity and high specificity for magnetic resonance studies of the hip. However, to the best of our knowledge, there are no studies in the literature to compare the MRI findings in children suffering from LCPD with hip arthroscopy.
Thus, we propose that MRI cannot be completely relied upon for identifying all the intra-articular pathologies in children with LCPD, although it has a good complimentary role in such circumstances. We feel one should have a low threshold for resorting to hip arthroscopy as a diagnostic procedure in cases of doubt regarding the pathology and in cases of persistence of pain, although its invasiveness is one factor not allowing for its routine use in such circumstances. Moreover, arthroscopy only reveals intra-articular and surface pathologies and little is revealed about what goes on inside the femoral head. Since LCPD is primarily a non-articular disease, plain radiographs and MRI are clearly superior to arthroscopy for the diagnosis and follow-up of the cases. However, in patients with severe persistent pain with suspicion for joint changes, arthroscopy can provide a safe procedure for eliciting the associated joint pathology. The main limitations in our study were relatively small sample size and a probable selection bias. Use of conventional MRI as compared to MRA, which is reported to have a better resolution for identifying intra-articular pathologies, was also a limiting factor. Definite conclusions regarding the role of hip arthroscopy in active stage of LCPD need to be established in future with follow-up studies.
References
Nelitz M, Lippacher S, Krauspe R, Reichel H (2009) Perthes disease: current principles of diagnosis and treatment. Dtsch Arztebl Int 106(31–32):517–523
Barker DJ, Hall AJ (1986) The epidemiology of Perthes’ disease. Clin Orthop Relat Res 209:89–94
Paterson D, Savage JP (1986) The nuclide bone scan in the diagnosis of Perthes’ disease. Clin Orthop Relat Res 209:23–29
de Sanctis N, Rega AN, Rondinella F (2000) Prognostic evaluation of Legg–Calvé–Perthes disease by MRI part I: the role of physeal involvement. J Pediatr Orthop 20(4):463–470
Dillman JR, Hernandez RJ (2009) MRI of Legg–Calve–Perthes disease. Am J Roentgenol 193(5):1394–1407
Garra G, Singer AJ, Taira BR, Chohan J, Cardoz H, Chisena E, Thode HC Jr (2010) Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med 17(1):50–54
Kamegaya M, Moriya H, Tsuchiya K, Akita T, Ogata S, Someya M (1989) Arthrography of early Perthes’ disease. Swelling of the ligamentum teres as a cause of subluxation. J Bone Joint Surg Br 71(3):413–417
Catterall A (1971) The natural history of Perthes disease. J Bone Joint Surg Br 53:37–53
Herring JA, Kim HT, Browne R (2004) Legg–Calve–Perthes disease. Part I: classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am 86-A(10):2103–2120
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87(7):1012–1018
Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP (2006) Sensitivity of MR arthrography in the evaluation of acetabular labral tears. Am J Roentgenol 186(2):449–453
Czerny C, Hofmann S, Neuhold A, Tschauner C, Engel A, Recht MP et al (1996) Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 200(1):225–230
Mitchell B, McCrory P, Brukner P, O’Donnell J, Colson E, Howells R (2003) Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sport Med 13(3):152–156
Keeney JA, Peelle MW, Jackson J, Rubin D, Maloney WJ, Clohisy JC (2004) Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res 429:163–169
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tiwari, V., Gamanagatti, S., Mittal, R. et al. Correlation between MRI and hip arthroscopy in children with Legg–Calve–Perthes disease. Musculoskelet Surg 102, 153–157 (2018). https://doi.org/10.1007/s12306-017-0513-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-017-0513-9