Abstract
Radial head prostheses (RHP) have been developed to decrease the complications rate following a radial head resection surgery. The aim of the RHP is to replicate the physiological radiocapitellar tracking, reproducing the mechanical function of the native radial head: to stabilize the elbow and to shear the forces passing through the elbow along with the other stabilizers. The currently used RHP models try to achieve this target with three different prosthesis’ strategies: (a) loose fit stem, (b) bipolar radial head or (c) anatomical radial head. Even if the radial head fixation is the preferred technique in every possible case and the resection can be still considered a possible option, in the last years there has been a growing worldwide consensus in using the radial head replacement in patients with unfixable radial head fractures, especially if associated with complex elbow instability. However, complications after a RHP are not uncommon, and their rate is raising as long as the implants number are increasing. The main difficulties are due to the implantation technique that needs to be performed with the same attention and precision used for the replacement of all the other joints, and to the concurrent treatment of the associated lesions. A personalized postoperative rehabilitation program is essential for obtaining good results and decreasing the complications rate. Concern exists for the young age of the patients that often require a RHP: personal experience and literature analysis suggest that if the clinical and radiographic results are positive after a 6–12-month follow-up, good outcomes can be also expected at a medium- or long-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radial head prostheses (RHP) have been developed to decrease the potential complications following radial head resection surgery. The role of the radial head in the elbow stability has been illustrated by Hammacher, according to the “Greek Temple” model [1]. Mainly, if it is associated with other lesions, the resection of the radial head (a secondary stabilizer, resisting valgus and posterolateral instability of the elbow and preventing proximal migration of the radius) alters the physiological elbow kinematics and biomechanics (Fig. 1a–c) and can cause several complications.

Modified from Hammacher and van der Werken [1]
The Greek temple model. a The radial head is not a main elbow stabilizer: In case of isolated fracture, radial head removal does not cause instability of the construct. b If the radial head fracture is associated with medial collateral ligament or interosseous membrane lesion, the construct is unstable. c The radial head fixation or replacement, possibly associated with interosseous membrane repair, restores the stability of the construct.
The complications associated with a radial head resection can be classified in early (instability) or delayed (chronic instability, arthritis, grip weakness, stiffness, ulnar nerve problems). Early complications can be: (1) valgus recurrent instability in case of the associated medial collateral ligament (MCL) lesion; (2) a recurrent posterolateral rotatory instability (PLRI) in case of associated lateral collateral ligament (LCL) lesion; (3) a persistent instability in case of associated coronoid and LCL lesion; (4) Essex-Lopresti lesion in case of associated interosseous membrane and distal radioulnar joint (DRUJ) injuries. Delayed possible complications are: (1) progressive cubitus valgus, caused by a tardy MCL elongation; (2) medial and posterior drift of the proximal radial stump; (3) progressive radiographic arthritic changes, due to the over-axial load that, in the absence of the radial head, is completely transferred to the ulno-humeral joint; (4) decreased grip strength and weak forearm rotation; (5) secondary ulnar nerve complaints are also possible; (6) stiffness, due to long cast treatment applied after RH resection to prevent instability, persistent joint incongruences, ulno-humeral arthritis or heterotopic ossification (HO) formation.
Curiously, the first RHP models consisted of ferrule caps applied over the radial neck, implanted with the aim to prevent heterotopic bone formation [2] (Fig. 2).
Only many years later, the important role of the radial head to improve stability and to contribute to load distribution has been understood. Even if the radial head resection can be still considered a possible option, and there are several studies reporting good results in long-term follow-up studies after radial head resection [3,4,5], in the last years there has been a growing worldwide consensus in using radial head replacement in patients with unfixable radial head fractures, especially if associated with complex elbow instability. In particular in these cases, RHP are strongly suggested nowadays.
The goals of radial head replacement can be divided on a temporary basis:
-
Short term: during the first 2–3 weeks the radial head prosthesis role is to maintain the elbow reduced and stable, leading the soft tissue stabilizers (medial and LCL, possibly interosseous membrane and distal radioulnar joint) to heal correctly. During this period, the stability provided by the RHP usually allows to mobilize the elbow, reducing the risk of stiffness
-
Medium/long term: over subsequent months and years the radial head prosthesis contributes to load absorption, avoiding mechanical overload on the ulno-humeral joint and MCL during the valgus stress, preventing ulno-humeral arthrosis, valgus deformity, and tardy ulnar nerve symptoms.
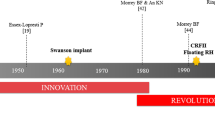
Over the last decades, radial head implants have undergone significant evolution: all the current radial head implants are modular, allowing to match different sizes of heads and stems to find the best conformity between patient’s anatomy and prosthesis. The many possible combinations permit to reproduce as closely as possible the size and the shape of the native radial head.
The materials have improved, passing from acrylic, glass and silicone rubber used in the past, to modern materials like vitallium, cobalt–chromium, titanium, and pyrocarbon. Also shapes and surfaces are evolved, seeking for a better relationship “implant-capitellum” and a better stem fixation.
In particular:
-
For the head: development of bipolar models and anatomical shapes (Table 1), use of materials with a minor cartilage wear, models designed to allow head–stem assembly in situ
Table 1 Unipolar and bipolar heads: advantages and disadvantages -
For the stem: development of materials, shapes, finished surface, lengths and expansion mechanism to obtain a better fixation (Table 2).
Table 2 Different types of stem fixation: advantages and disadvantages
Three are the different philosophies inspiring all the RHP available on the market in the last 10 years: loose fit models, bipolar implants, and anatomical RHP.
-
Loose fit: the stem is circular and smooth; it is intentionally inserted undersized, so that the stem presents some degrees of freedom in floating inside the canal. The loose fit, during the elbow movements in flexion extension and prono-supination, helps to accommodate the inevitable incongruences among the prosthesis and the capitellum and the lesser sigmoid notch, with a mechanism of self-centering similar to a bipolar prosthesis.
On the contrary, the models composed by a monopolar head and a press-fit or cemented stem rely on their position and their approximation of the native anatomy to achieve a physiological tracking with the capitellum and the lesser sigmoid notch.
-
Bipolar: prostheses present an articulation in the head–neck junction of the implant. They exist in smooth-stemmed and fixed stem varieties (press fit or cemented). Bipolar prosthesis, thanks to its self-alignment to the capitellum and to the proximal ulna, can adapt the tracking, even if not perfectly seated. The theoretical disadvantages using this type of prosthesis are the possible wear debris formation and an inferior mechanical stabilization in severe elbow instabilities.
-
Anatomical: the anatomical RHP have been developed to replicate as closely as possible the radial head anatomy, reproducing the physiological radiocapitellar kinematics and biomechanics. The anatomy of the radial head is scarcely consistent, and, until now, only one model (Acumed Anatomical Radial Head; Acumed, Hillsboro, OR) followed this philosophy.
The most important features of each radial head prosthesis we used in our Institution since 2000 are resumed in Table 3. As shown in Table 3, the many available models allow to the surgeon a wide choice of different shapes, materials, and fixation. Our preference is for uncemented implants, considering the frequent young age of the patients, and the possibility of future prostheses removal. For the same reason, we do not routinely use the stem expansion models that are difficult to remove. Instead, this kind of implant, composed of titanium (stem) and pyrocarbon (head), is suggested to treat patients with nickel allergy.
Some implants allow insertion of the stem first, followed by placement of the head onto the stem, with coupling in situ. This feature is useful in cases presenting an intact LCL and with an insufficient lateral translation of the proximal radius, preventing insertion of an assembled prosthesis.
Indications/contraindications
Main indications and contraindications of radial head replacement, with possible alternative surgical treatments, are shown in Table 4.
Surgical technique: tips and tricks
The patient is placed in a supine decubitus on the operating table. A non-sterile tourniquet is commonly used.
-
1.
Exposure
-
(a)
Superficial layer The skin incision is usually lateral. It can be posterior, if associated lesions, like olecranon fracture, anteromedial coronoid fracture or a MCL tear, have to be addressed. In the last two cases, it is possible—based on the surgeon preference—to perform a combined (lateral and medial) approach.
-
(b)
Deep layer Two are the suggested surgical approaches to perform a RH prosthesis: Transtendon approach and Kocher approach, based on the LCL evaluation. Based on the preoperative imaging and examination obtained in operative room after anesthesia, the presence of an injured LCL is evaluated. If the LCL is not considered torn, our preference goes to the transtendon approach, splitting the common extensor tendon. This approach permits a good exposure of the proximal radius, facilitating the stem preparation and the implantation phases. More anterior approaches, like Kaplan approach, between common extensor and extensor carpi radialis brevis and longus, poses at major risk the posterior interosseous nerve (PIN) from possible intra-operative injuries: it is a good exposure to perform radial head fixation, but we do not recommend it if a RHP can be anticipated. If the LCL is torn or its lesion is suspected, a Kocher approach is performed. This approach lies between the anconeus and the extensor carpi ulnaris and follows the lateral ulnar collateral ligament long its course from the condyle to the ulnar insertion remaining just anterior to it. For this reason, this approach permits an optimal exposure for its evaluation and treatment. In many circumstances, incising and divaricating the subcutaneous tissue, a radial head fragment, usually of conspicuous size, can be easily visualized, due to the avulsion of the common extensor muscles, capsule and LCL from the lateral epicondyle. In these cases, the approach goes through the injured tissues. In other cases, since the injury to the lateral complex proceeds from the inside-out, the extensor origin is intact, while the capsule containing the LUCL (lateral ulnar collateral ligament) fibers is avulsed deeplier. In both the situations, the Kocher approach, which lies directly over the LUCL, is the preferred approach to address the lateral ligament complex. Exploiting both approaches (transtendon or Kocher) if the joint capsule and the annular ligament are intact, they are incised, exposing the radial head and removing the intra-articular hematoma. The anterior capsule and the origins of the extensors are elevated off the anterior aspect of the humerus.
-
(c)
Proximal extension To improve the exposure, the dissection can be extended proximally, detaching the origin of the brachio-radialis from its humeral insertion.
-
2.
Fragments removal If the fracture is not amenable to be fixed, all the bony fragments are removed and, if it is present, the residual part of the radial neck is resected by a micro-sagittal saw with a cut perpendicular to the shaft; the stability is tested. Bain [6] was the first to report that applying a valgus stress force with the forearm in pronation and the elbow at 30° of flexion, a narrowing > 2 mm between radial neck and capitellum is indicative of disruption of the anterior band of the MCL. Moreover, he stated that if the same narrowing is possible with the elbow extended, it indicates that the anterior and posterior capsule is also torn. Putting a clamp on the radial neck and applying a longitudinal traction, pulling proximal, on the proximal part of the radius, a change > 2 mm in the distance between the radial neck and the capitellum is abnormal [6]. Both of these stress tests can be performed under fluoroscopic control.
Confirmed the necessity of replacing the RH, all the bony fragments removed are put together on the back table to recreate the native shape. This is useful to confirm that all the fragments have been excised and to evaluate the size of the implant. The joint is irrigated to remove loose bodies and it is inspected, to evaluate the presence of associated chondral injury or osteochondral fracture of the capitellum or of the coronoid.
-
3.
Stem preparation Placing a Hohmann retractor over the posterior part of the radial neck, it is possible to deliver anteriorly and laterally the proximal radius, facilitating reaming and insertion of the prosthesis. If the LCL is torn a varus and supinating stress maneuver allows an even better exposure. At the opposite, applying an Hohmann retractor anteriorly can damage the posterior interosseous nerve (PIN) and for this reason it is usually discouraged.
The medullary canal of the proximal radius is then prepared with a starter awl and a neck planer, if available, is used. Specific serial-sized broaches are used, removing the cancellous bone, and reaching a cortical bone contact.
-
4.
Radial head sizing Next step is the implantation of the trial components, paying great attention to the correct sizing of the radial head. In fact, it has been proven that lengthening and shortening of as little as 2.5 mm affect the ulno-humeral kinematics and radiocapitellar pressures [7]. An overstuffing can lead to premature radiocapitellar wear and restrict the elbow flexion; undersizing the head may result in residual valgus instability and, not contributing to the load sharing, increases stress at the ulno-humeral joint. Recent studies have underlined the difficulties to evaluate the radial head size with anteroposterior radiograph of the ulno-humeral joint [8,9,10]. A comparative radiograph, at the same flexion-extension and prono-supination, of the injured and contralateral elbow can be an option [11]. On AP fluoroscopic image, a widening of the lateral ulno-humeral joint can be an anatomical variant [8]; therefore, it is not a reliable indicator of radiocapitellar joint overstuffing. Instead, any loosening of the normal parallelism of the opposing joint surfaces of the medial ulno-humeral joint is highly suggestive of implant overlenghtening, even if this incongruity becomes radiographically apparent only when the overlenghtening of the radius is equal or superior to 6 mm [10].
To select the right head size, it is possible to follow 5 tips (Table 5).
The tips and tricks to correctly implant the stem are resumed in Table 6.
-
5.
RHP trial insertion The appropriate trial head is secured to the appropriate trial stem. The trial prosthesis is inserted, with the collar of the prosthesis flush with the resected stem: for a correct seating, at least two-thirds of the diameter of the radial neck should be in contact and should support the implant. The elbow and forearm are placed through a full arc of motion and the diameter, the height, the tracking and congruency of the prosthesis is evaluated visually and with the aid of an image intensifier.
If an acceptable alignment and tracking are confirmed, the trial components are removed and the final prosthesis is inserted. Implanted the definitive prosthesis, a final assessment of motion and stability of the elbow and forearm is again performed. At the end of the procedure, if necessary, LUCL and common extensor origin are carefully repaired to the bone, with drill holes or with suture anchors. If the LUCL (representing the posterior portion of the lateral ligament complex) remains attached to the lateral epicondyle, the anterior half of the lateral ligament complex (annular ligament and radial collateral ligament) is repaired to the posterior half. This repair is followed by closure of the muscle-splitting interval that was used for initial exposure.
-
6.
Definitive RHP insertion Based on the trial evaluation, the definitive prosthesis is chosen and implanted. The range of motion and the elbow stability are checked. The annular ligament is repaired and, in case of torn muscles or LCL lesion, they are repaired with transosseous sutures or suture anchors.
Postoperative management
The postoperative phase must be tailored to the injury, considering elbow stability and the associated injuries treatment. If at the end of the procedure, the elbow is stable, a protective brace can be applied for 2–3 weeks and an early mobilization can be allowed. If a slight PLRI is still present, the elbow is protected in a 90° brace with the wrist placed in pronation, an active over-head mobilization allowed only after 7–10 days, avoiding elbow varus stresses for at least 4 weeks. A closer clinical and X-rays follow-up are also recommended.
Results
A recent systematic study about metallic modular prosthesis, including more than 700 patients, highlights good results in a short and medium follow-up, without evidence that an implant is superior to another [15]. In our experience, as well, we have not found any significant difference between monopolar and bipolar prosthesis.
Even if there are few studies about RHP long-term follow-up, they suggest that good results achieved in the short-term follow-up are usually maintained over time [17].
In the literature, the percentage of implant failure is reported to be between 0 and 29% [15]. In our experience [16], the revision percentage was 6% at 2 years f.u. (2/31). These results are confirmed at 5-year follow-up (unpublished data).
Radial head replacement complications
The most common complications are:
Loosening
Asymptomatic radiolucent lines around the stem, not presenting any evolution at the following X-rays, are frequently seen in loose fit prostheses and, less often, with press-fit stems. Bone reabsorption of the proximal radial neck caused by stress shielding is not uncommon using press-fit stems; also these initially worrisome images remain stable during the time. At the opposite, stem loosening is generally painful [18] and presents evolutive progression of bone reabsorption and stem loosening signs (Fig. 3).
We noticed and described [16] that in some cases of press-fit stem a periosteal bone reaction on the anterolateral neck cortical is observed. This radiographic sign, appearing within 3–6 months from the implant, later described also by other authors [19], represents in our experience a positive factor, being associated with good bone/stem integration, lasting in the time.
Overstuffing
It is one of the most frequently seen complications after radial head replacement. On the anteroposterior X-ray, it can be found as asymmetric ulno-humeral joint space, wider on the radial side (Delta river sign) [20] (Fig. 4a, b).
With the CT scan, it is possible to compare the prosthesis length to the lesser sigmoid notch. In the sagittal view, a loss of symmetry between the humeral center of rotation and the olecranon and coronoid can confirm the over-lengthening of the radial head (Fig. 4c, d).
Capitellar erosion
It is usually due to prosthesis overstuffing or due to longitudinal instability, as in Essex-Lopresti syndrome. It is favored by the articular cartilage damage caused by the initial injury. The arthritic changes may involve also the ulno-humeral articulation.
Nerve lesions
The most frequently damaged nerve is the Posterior Interosseous Nerve. To prevent these iatrogenic lesions, we suggest:
-
do not use Hohmann retractor posteriorly on the radial neck
-
place the forearm in a pronation position while exposing the radial neck, in order to keep the posterior interosseus nerve far away from the surgical field
-
avoid the tissue dissection beyond the biceps tuberosity on the radius.
Osteoarthritis
Osteoarthritis (OA) of the capitellum is usually the consequence of post-traumatic cartilage lesions, and it can deteriorate faster if a residual instability or a prosthesis hyper-pressure is present.
Stiffness and heterotopic ossifications
The most common complication associated with radial head prosthesis is postoperative stiffness that can be caused by capsular contracture, OA, HOs, or ulnar neuropathy.
Others
Dissociation of the components, deep infection.
Conclusions
For many years, radial head resection has been the only surgical treatment available for displaced radial head fractures and, until a recent past, it was not uncommon listening expert senior surgeons remembering just few unsatisfactory results after having performed many radial head resections during their career. Moreover, some papers reporting good clinical outcome after radial head resection in long-term follow-up studies are also available [3,4,5]. Probably, after the RH resection, a grossly common extensor tendon imbrication (tensioning the LCL complex), a long cast applied for 4–6 weeks, often with the hand in supination (tensioning the MCL) could explain the lower than expected rate of instability cases. Moreover, it is a common experience that many residual instabilities of the elbow evolve in arthritis quickly, with a partial loss of motion but regaining stability. A mild residual instability or a postsurgical degenerative ulno-humeral arthritis are situations usually well tolerated in low demand patients, explaining the confidence, especially in the past, to perform resection in every not fixable radial head fracture.
Nowadays, we are aware of the mechanical importance of the radial head, of its role in elbow stability and kinematics and, if it is not possible to fix the fracture, the shared attitude by the majority of dedicated elbow surgeons is to implant a RHP if intra-operative instability is present. In fact, it is a common experience to see patients with a chronic recurrent or persistent elbow instability caused by simple resection of a radial head fracture, and their treatment represents one of the most difficult challenges of the elbow surgery. The primary technical goal of the RHP is to replicate closely the kinematics and the biomechanics of the native radial head.
Three are the different philosophies following this target:
-
Loose fit implant
-
Bipolar implant
-
Anatomical implant.
There is currently no evidence to prefer one type of RHP over another. In particular, some studies report similar outcomes and complications using monopolar or bipolar implant [15, 16].
Even if it has been suggested that acute radial head arthroplasty may only serve as a spacer allowing the torn ligament to heal, RHP need to be performed with the same attention and precision used for the replacement of all the other joints, treating properly the associated lesions.
Concern exists for the young age of the patients that often require a RHP. Personal experience and literature analysis suggest that if the clinical and radiographic results are positive after a 6–12-month follow-up, good outcomes can be also expected at a medium- or long-term follow-up.
References
Hammacher ER, van der Werken C (1996) Radial head fractures: operative or conservative treatment? The Greek temple model. Acta Orthop Belg 62(Suppl 1):112–115
van Riet RP, van Glabbeek F (2007) History of radial head prosthesis in traumatology. Acta Orthop Belg 73(1):12–20
Antuña SA, Sánchez-Márquez JM, Barco R (2010) Long-term results of radial head resection following isolated radial head fractures in patients younger than forty years old. J Bone Joint Surg Am 92(3):558–566
Faldini C, Nanni M, Leonetti D, Capra P, Bonomo M, Persiani V, Galante C, Giannini S (2012) Early radial head excision for displaced and comminuted radial head fractures: considerations and concerns at long-term follow-up. J Orthop Trauma 26(4):236–240
Nestorson J, Josefsson PO, Adolfsson L (2017) A radial head prosthesis appears to be unnecessary in Mason-IV fracture dislocation. Acta Orthop 88(3):315–319
Bain GI, Ashwood N, Baird R, Unni R (2005) Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. Surgical technique. J Bone Joint Surg Am 87 Suppl 1(Pt 1):136–147
Van Glabbeek F, Van Riet RP, Baumfeld JA, Neale PG, O’Driscoll SW, Morrey BF, An KN (2004) Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am 86-A(12):2629–2635
Rowland AS, Athwal GS, MacDermid JC, King GJ (2007) Lateral ulnohumeral joint space widening is not diagnostic of radial head arthroplasty overstuffing. J Hand Surg Am 32(5):637–641
Shors HC, Gannon C, Miller MC, Schmidt CC, Baratz ME (2008) Plain radiographs are inadequate to identify overlengthening with a radial head prosthesis. J Hand Surg Am 33(3):335–339
Frank SG, Grewal R, Johson J, Faber KJ, King GJ, Athwal GS (2009) Determination of correct implant size in radial head arthroplasty to avoid overlenghtening. J Bone Joint Surg Am 91(7):1738–1746
Athwal GS, Rouleau DM, MacDermid JC, King GJ (2011) Contralateral elbow radiographs can reliably diagnose radial head implant overlengthening. J Bone Joint Surg Am 93(14):1339–1346
van Riet RP, van Glabbeek F, de Weerdt W, Oemar J, Bortier H (2007) Validation of the lesser sigmoid notch of the ulna as a reference point for accurate placement of a prosthesis for the head of the radius: a cadaver study. J Bone Joint Surg Br 89(3):413–416
Moon JG, Berglund LJ, Domire Z, An KN, O’Driscoll SW (2009) Stem diameter and micromotion of press fit radial head prosthesis: a biomechanical study. J Shoulder Elb Surg 18(5):785–790
Abdulla I, Langohr GD, Gladwell M, Yeung C, Faber KJ, King GJ, Athwal GS (2015) The effect of fracture comminution on the reliability and accuracy of radial head sizing. J Shoulder Elb Surg 24(3):364–368
Heijink A, Kodde IF, Mulder PG, Veltman ES, Kaas L, van den Bekerom MP, Eygendaal D (2016) Radial head arthroplasty: a systematic review. JBJS Rev 4(10). doi:10.2106/JBJS.RVW.15.00095
Rotini R, Marinelli A, Guerra E, Bettelli G, Cavaciocchi M (2012) Radial head replacement with unipolar and bipolar SBi system: a clinical and radiographic analysis after a 2-year mean follow-up. Musculoskelet Surg 96(Suppl 1):S69–S79
Marsh JP, Grewal R, Faber KJ, Drosdowech DS, Athwal GS, King GJ (2016) Radial head fractures treated with modular metallic radial head replacement: outcomes at a mean follow-up of eight years. J Bone Joint Surg Am 98(7):527–535
O’Driscoll SW, Herald JA (2012) Forearm pain associated with loose radial head prostheses. J Shoulder Elb Surg 21(1):92–97
Berschback JC, Lynch TS, Kalainov DM, Wysocki RW, Merk BR, Cohen MS (2013) Clinical and radiographic comparisons of two different radial head implant designs. J Shoulder Elb Surg 22(8):1108–1120
Gauci MO, Winter M, Dumontier C, Bronsard N, Allieu Y (2016) Clinical and radiologic outcomes of pyrocarbon radial head prosthesis: midterm results. J Shoulder Elb Surg 25(1):98–104
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Marinelli, A., Guerra, E., Ritali, A. et al. Radial head prosthesis: surgical tips and tricks. Musculoskelet Surg 101 (Suppl 2), 187–196 (2017). https://doi.org/10.1007/s12306-017-0504-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-017-0504-x