Abstract
Background
Glenoid bone defect and excessive medialization could represent challenging issues during reverse shoulder arthroplasty, especially in the setting of revision surgery. Although a solution is offered by the Boileau’s BIO-RSA technique in primary cases, only autologous iliac crest bone graft and homologous graft from bone banks are available for revision surgeries, with known disadvantages and risk of graft resorption and implant failure.
Materials and methods
We describe in this work a new technique based on a customized porous tantalum device to be used in salvage situations, aimed at lateralization of the glenoid component of a reverse shoulder arthroplasty. Between 2014 and 2015, five patients received a customized tantalum-augmented RSA at our institution. The augments we applied are actually on the market for acetabular bone loss management: these were opportunely prepared and fixed to the metal back of the glenoid component before implantation.
Results
In the five cases treated, no major or minor complications have been recorded to date. Despite the short follow-up, all the implants are still in situ. All of the patients referred complete subjective satisfaction and return to their daylife activities without pain within 4 months after surgery.
Conclusions
The customized tantalum-augmented RSA technique represents in our experience a useful and safe solution in managing glenoid bone loss and medialization. Adaptability to virtually every device in the market should be regarded as important point of strength of this technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glenoid bone defect and excessive medialization represent important challenges during surgery for shoulder arthroplasty. Both functional results and eventual complications could be consistently influenced by the management of these issues. When dealing with reverse shoulder arthroplasty (RSA), medialization of the center of rotation could result in loss of shoulder contour and cosmetic concerns, lower tension of the residual rotator cuff tendons and periarticular soft tissues, higher risk of medial impingement and scapular notching, and implant instability as well. Several changes to the original design of the Grammont’s prosthesis have been proposed through metallic lateralization (of the glenosphere or of the baseplate), leaving doubts about the increased shear forces applied to the glenoid component, that could potentially drive to increased risk of glenoid loosening [1–3]. In 2011, Pascal Boileau and coworkers described the bony increased-offset reversed shoulder arthroplasty technique (BIO-RSA), with autogenous bone graft harvested from the humeral head on a specifically designed baseplate, maintaining the prosthetic center of rotation at the prosthesis–bone interface. The authors described good functional results and high rate of osteointegration of the graft [4]. In our opinion, the BIO-RSA technique offers a useful but partial solution to the problem of a mediatized glenoid. Despite reliable in the case of primary RSA in patients with good bone quality, the destiny of the graft is not clear, especially in the case of low-quality humeral bone. Furthermore, the BIO-RSA technique is obviously not applicable when dealing with revision surgery and in most cases of fracture sequelae, especially when osteosynthesis devices are present. In such cases, only autologous iliac crest bone graft and homologous graft from bone banks are available, both endowed, however, with known disadvantages and risk of graft resorption and implant failure [5, 6].
Osteoinductive and osteoconductive properties of porous tantalum are well known in the field of revision adult joint reconstruction [7–10]. In this work, we describe a new technique aimed at increasing glenoid base-plate lateralization in reverse shoulder arthroplasty by means of a customized porous tantalum augment to be used in salvage situations.
Materials and methods
Between 2014 and 2015, five patients (five shoulders) were managed in our institution by the senior authors (N.I.) and received a glenoid-augmented reverse total shoulder arthroplasty (DePuy-Johnson and Johnson, Warsaw, IN). All these cases represented salvage situations with severe glenoid bone loss or dimorphic glenoid. Initial diagnosis were: fracture sequelae in one case, failure of previous anatomic total shoulder arthroplasty in one case, deep infection sequelae after previous RSA in one case, primary advanced shoulder osteoarthritis with dimorphic glenoid in one case and eccentric glenohumeral osteoarthritis with severe glenoid erosion in one case. In order to face the sensible medialization and bone loss of the glenoid, patients were treated with a customized augmentation of the prosthetic glenoid component by means of a porous tantalum device normally on the market for acetabular bone defect management (Trabecular Metal™, Zimmer, Warsaw, IN). The device was adequately prepared and implanted as described below. A standard deltopectoral approach was used in all cases. General anesthesia was used, supplemented with interscalene brachial plexus block. Antibiotic prophylaxis and antithromboembolic prophylaxis were constantly used, choosing drugs and posology upon anesthesiologic and/or infectivologic pre-operative evaluations. After surgery, the shoulders were immobilized with a sling in adduction and internal rotation, and a standard physiotherapy program started after the third week from surgery.
Description of the technique
A porous tantalum dish of 26 mm diameter and 6 mm thickness (Trabecular Metal™, Zimmer, Warsaw, IN) is drilled in order to obtain a full congruency with the multi-hole long central pegged glenoid component (+10 glenoid component; Delta Xtend, DePuy-Johnson and Johnson, Warsaw, IN). The slightly concave aspect of the dish is then cemented to the glenoid metal back through using antibiotic-charged polymethylmethacrylate cement. Cement thickness could vary of few millimeters, depending on the desired lateralization. Before cement solidification, cement in excess is removed from the contour of the construct and from the screw holes. When the cement is solid, the tantalum-augmented glenoid component is then implanted through careful impaction on the pre-drilled scapular plan, and fixed with 3–4 screws depending on glenoid anatomy and bone stock. The glenosphere is positioned and fixed with a central coaxial screw, in line with instructions from the manufacturer (Fig. 1, 2). In the case of revision of previous prosthetic glenoid component, with residual concentric glenoid bone loss, bone chips from the humeral metaphysis are eventually used for partial bone stock recovery before implanting the final prosthetic component (Fig. 3). When dealing with acquired dimorphic or mild dysplastic retroverted glenoid (e.g., Walch type B1 and 2), a slight eccentric glenoid reaming is conducted first, in order to increase the contact area between glenoid bone and tantalum device of at least 70 %. Finally, the humeral shaft is prepared and the humeral prosthetic component is implanted. After careful trials for implant stability evaluation, the definitive insert thickness is chosen, and the final implant is reduced.
Description of the technique, a the long pegged glenoid metal back, b, c pre-drilling of the tantalum dish: after the central hole is prepared, the peripheral screw holes are drilled using the glenoid component as a mask, d, e the prepared augment and the augment presented on the glenoid component, f–h the concave aspect of the dish is cemented to the glenoid metal back through using antibiotic-charged polymethylmethacrylate cement, i final aspect of the construct before implantation, j, k impaction of the construct on the glenoid plan and screw fixation
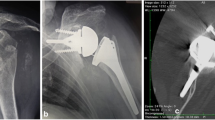
Case n. 1: 44-year-old male treated with ORIF for complex proximal humeral fracture, a X-rays 3 months after surgery in the district hospital, showing progressive humeral head osteonecrosis; b, c X-rays 6 months after further treatment in another institution: the patient presented to our attention complaining pain and severe function impairment; glenoid bone shows severe erosion and medialization, d, e X-ray control 3 months after surgery with tantalum-augmented reverse shoulder prosthesis implantation
Case n. 2: 72-year-old male treated with total shoulder arthroplasty 9 years before for post-traumatic glenohumeral arthropathy, a pre-operative X-ray evaluation, b intraoperative appearance after removal of the polyethylene glenoid component: Severe concentric glenoid bone loss is shown, c partial bone stock recovery with chips from the humeral metaphysis, d tantalum-augmented glenoid component impaction, e final X-ray control after surgery
Results
With a follow-up ranging from 5 to 20 months, all the implants were in place at the time of this study. No in-hospital medical complications were reported in our series in the perioperative period, and no postoperative complications were reported in the follow-up time. All the patients in the series were pain-free and satisfied with the final clinical outcome. Return to daylife activities was achieved within 4 months from surgery.
Discussion
Medialization of the center of rotation is one of the fundamental hallmarks in the Grammont’s reverse prosthesis design, reducing shear forces and torque acting on the prosthetic glenoid component, and promoting implant stability [11]. However, it is not free of unwanted consequences. Through lowering the tension of the residual rotator cuff, it is plausible a not favorable effect takes place upon humeral internal and external rotation. Furthermore, proximity of the implant to the scapular neck could favor notching, impingement and eventual dislocation of the implant itself. Finally, typical modification of the shoulder contour could drive to cosmetic concerns. Excessive glenoid medialization, as often seen in severely dimorphic glenoid and in revision surgery, could eventually drive to excessive and unfavorable deltoid lever arm distance and enhance the above-mentioned side effects as well.
The BIO-RSA approach proposed by Pascal Boileau and coworkers offers an appealing solution to these issues [4]. Harvesting a small bone dish from the humeral head on the glenoid baseplate, this technique provides glenoid lateralization while maintaining the prosthetic center of rotation at the prosthesis–bone interface, and graft integration is described in almost all the reported cases [4]. With the BIO-RSA approach, some authors have recently described reduction of scapular notching incidence, despite a sensible gain in active external rotation was not always demonstrated [12, 13]. Obvious limits of this technique are revision surgery and fracture sequelae, due to humeral head unavailability, while conditions of low bone quality could represent a relative contraindication. Alternative techniques are represented by autologous bone graft from iliac crest, homologous bone graft from bone banks, and metallic lateralization. All of them present several disadvantages due to donor site disease, graft resorption, implant failure and limited published data available [3, 5, 6].
In the last decade, porous tantalum has gained wide attention in bone defect treatment in joint revision surgery, due to its notable properties of biocompatibility, osteoinduction and osteoconduction, facilitating vascularization and biologic in-growth [7–9]. Only recently, however, it has been introduced in the shoulder arthroplasty scenario, with some prosthetic devices endowed with porous tantalum covering the glenoid metal back, the glenoid central peg and the metaphysis of the humeral stem (Trabecular Metal Reverse Shoulder System, Zimmer, Warsaw, IN). At the time we carried out the cases described in this work, such new devices were not in the market yet, or just coming out. Nevertheless, we believe the modality of fixation of the glenoid component (i.e., with a central coaxial screw) and the number of available glenoid screws (i.e., four instead of two) give the prosthetic device we used a consistent reliableness when dealing with implant stability, also in the presence of a customized glenoid augmentation.
In this work, we described the use of tantalum augments in situations of severe glenoid bone loss or severe glenoid medialization. All the five cases in which we used this technique represented salvage situations.
In our technique, a tantalum dish is prepared and cemented to a long pegged metal back and then the construct is fixed to the native glenoid. Coaptation of the device to the glenoid is ensured by the long central peg fit and peripheral screws fixation. Despite the limited number of patients treated, and the short follow-up to date, this technique resulted reliable, without major or minor complications. By analogy with several other similar situations in which porous tantalum has been successfully used, we are confident this technique could give useful and reproducible results. Adaptability to virtually every device in the market should be regarded as important point of strength of this technique, freeing the surgeon in the choice of the prosthesis.
We are aware our work could arise some doubts and critics about safeness and legal responsibility. The technique we presented should be regarded as an off-label use of devices normally present in the market for different indications. Furthermore, and despite generally accepted and performed by surgeons, manipulation of the tantalum augments through drilling and shape adaptation is not suggested by the manufacturer. These could be obviously seen as important shortcomings of the presented technique. However, we have to highlight that customized tantalum augments were applied only in exceptional and salvage situations in this work, where possible alternatives were few in number and the perspective of success not appealing, and after careful explanation to the patients and final patients’ free consent. After drilling with adequate instrumentation, the tantalum augment was accurately washed and cleaned up as best as possible of metallic debris. Finally, we payed attention in following the original technique described by the manufacturer about avoiding direct contact between the tantalum device and the prosthetic component through placing a cement layer in-between, avoiding metal-on-metal friction and secondary metallic debris production. We are actually coworking with a certified manufacturer to the development of glenoid-dedicated and ready-to-use augments in order to overcome the need of extemporary handling and modification of such devices in the operatory room.
With the number of revision shoulder surgeries progressively widening in the last years, we should consider that what are today extraordinary difficult-to-manage cases could became more and more frequent situations to face off in the next future. In this perspective, it is desirable new modular and ready-to-use devices and augmentations be developed, based on reliable biomaterials and conforming as much as possible with the glenoid bone defect to be treated. Efforts from companies and surgeons are warmly advocated in this direction.
References
Frankle M, Levy JC, Pupello D, Siegal S, Saleem A, Mighell M, Vasey M (2006) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency: a minimum two-year follow-up study of sixty patients: surgical technique. J Bone Joint Surg Am 88(Suppl 1):178–190
Valenti P, Sauzieres P, Cogswell L, O’Toole G, Katz D (2008) The reverse shoulder prosthesis: surgical technique. Tech Hand Up Extrem Surg 12:46–55
Costantini O, Choi DS, Kontaxis A, Gulotta LV (2015) The effects of progressive lateralization of the joint center of rotation of reverse total shoulder implants. J Shoulder Elbow Surg 24(7):1120–1128
Boileau P, Moineau G, Roussanne Y, O’Shea K (2011) Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 469(9):2558–2567
Shinar AA, Harris WH (1997) Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg Am 79(2):159–168
Wagner E, Houdek MT, Griffith T, Elhassan BT, Sanchez-Sotelo J, Sperling JW, Cofield RH (2015) Glenoid bone-grafting in revision to a reverse total shoulder arthroplasty. J Bone Joint Surg Am. 97(20):1653–1660
Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M (2004) Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am 86(Suppl 2):123–129
Levine B, Della Valle CJ, Jacobs JJ (2006) Applications of porous tantalum in total hip arthroplasty. J Am Acad Orthop Surg 14:646–655
Lingaraj K, Teo YH, Bergman N (2009) The management of severe acetabular bone defects in revision hip arthroplasty using modular porous metal components. J Bone Joint Surg Br. 91-B:1555–1560
Balla VK, Bodhak S, Bose S, Bandyopadhyay A (2010) Porous tantalum structures for bone implants: fabrication, mechanical and in vitro biological properties. Acta Biomater 6(8):3349–3359
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) The Grammont reverse prosthesis: design, rationale and biomechanics. J Shoulder Elbow Surg 14:147S–161S
Athwal GS, MacDermid JC, Reddy KM, Marsh JP, Faber KJ, Drosdowech D (2015) Does bony increased-offset reverse shoulder arthroplasty decrease scapular notching? J Shoulder Elbow Surg 24(3):468–473
Greiner S, Schmidt C, Herrmann S, Pauly S, Perka C (2015) Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg 24(9):1397–1404
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N. I. is a consultant for Depuy-Synthes and receives financial support for educational programs. T. M., G. C., M. R. and A. L. declare that they have no conflict of interest. No funding was received for this work.
Rights and permissions
About this article
Cite this article
Ivaldo, N., Mangano, T., Caione, G. et al. Customized tantalum-augmented reverse shoulder arthroplasty for glenoid bone defect and excessive medialization: description of the technique. Musculoskelet Surg 100 (Suppl 1), 13–18 (2016). https://doi.org/10.1007/s12306-016-0404-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0404-5