Abstract
Complex fractures of the distal radius are articular lesions and comminuted at the level of the epiphysis and metaphysis. Their treatment is difficult and in most cases surgical. Of all the different osteosynthesis methods available, internal fixation with plate and screws is the most commonly used. In particular, angular stability plates are superior in terms of rigidity and stability to conventional volar and dorsal plates. DVR plate has these mechanical characteristics, and its low profile has reduced frictions with surrounding soft tissues. For these reasons, this device implanted through a single volar approach, can stabilize the majority of volarly and dorsally displaced unstable distal radius fractures. In this study, 48 patients, affected by complex fractures of the distal radius treated with DVR volar plates, were assessed by the Mayo modified wrist score, the Italian version of the disability of the arm, shoulder and hand. The satisfactory results observed confirm the efficacy of this device.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular fracture of the distal radius is one of the most common lesions of the upper limb [1]. In particular, complex fractures (Type C according to the AO classification system) [2] in most cases are the result of high energy trauma and affect mostly young adults. In elderly patients, this type of injury may also occur following a simple trauma with low energy forces. Type C fractures are articular lesions and comminuted at the level of the epiphysis and the metaphysis and, for this reason, are considered difficult to treat. In order to accurately assess the type of fracture and plan a correct treatment strategy, a conventional radiograph usually has to be completed by computerized tomography (CT), and in some cases a three-dimensional (3D) reconstruction may be needed. The aim of treatment is to restore anatomically the articular surface and the proper height of the radius, its radial slope and volar tilt via stable fixation [3], which is an essential condition to allow early joint mobilization of the wrist and avoid degenerative osteoarthritis. Of all the different osteosynthesis methods available, the open reduction and internal fixation (ORIF) is the most commonly used [4, 5]. In the past, the main difficulty with ORIF was related to weak stability of the screws within the cancellous bone, often osteoporotic and comminuted, and for this reason early joint mobilization of the wrist was rarely performed [6–10].
Angular stability fixation of the distal radius was introduced by Kambouroglou [11] and Jupiter [12, 13] who first developed in the 1990s volar and dorsal plates with angular stability screws. Since then, this type of plate system has significantly evolved and has proved superior in terms of rigidity and stability to conventional volar and dorsal plates [14–16]. In particular, the authors believe that the introduction on the market of low profile angular stability plates has reduced the incidence of impingement between soft tissue and plate, without losing its fixation stability properties, which often occurs with older generation plates.
In the past, the surgical rationale was that volarly displaced fractures should be treated with a volar approach, and those with dorsal displacement should be treated with a dorsal approach or with double access [8, 9]. Using this type of volar implant allows to strongly stabilize also dorsally dislocated fractures [14–16], thus avoiding extensor tendon friction against the hardware and reducing periosteous gapping. Also the volar approach at the wrist provides little adverse effects to the flexor tendons, and their contact with the plate can be avoided with the reinsertion of the pronator quadratum [17, 18]. Satisfactory results with this device have been also reported in the literature for the treatment of complex wrist fractures, with considerable comminuted fragments, despite the presence of osteoporosis [19–22].
Materials and methods
Between January 2006 and December 2007, in the Orthopedics and Traumatology Unit of the Department of Surgical Sciences at the University of Parma, 48 complex fractures of the distal radius (Type C fractures in the AO classification) were treated surgically with distal volar radius (DVR) plate (Hand Innovation©). This means of synthesis used by the authors is a low-profile Titanium anatomical plate, held in place with traditional screws for diaphysis fixation and with a double row angular stability screws (with or without threading) for epiphysis fixation.
At admission, each patient sustained a radiographic investigation. In 35 cases a CT scan with 3D reconstruction was done to better classify the type of fracture and to plan a more effective surgery. For each patient, the following parameters were analyzed: age at the time of trauma, type of fracture, trauma mechanism, elapsed time until radiographic (X-ray) consolidation of the fracture and post-operative complications.
All patients were assessed before and after at least 1 year from surgery using the Italian version of the disability of the arm, shoulder and hand (DASH) questionnaire [23] which evaluates subjective functional capacity of the upper limb for various activities of daily living (ADL), and the Mayo modified wrist score (MMWS) [24, 25] which allows for a more objective assessment of pain and wrist function during the patients’ ADL. Range of motion (ROM) and grip strength (evaluated in percentage compared to the contralateral side) were also measured using a wrist goniometer and calibrated (January 2007) Jamar dynamometer. The American Society of Hand Therapists’ (ASHT) [26] standardized procedure was used to evaluate ROM and grip strength.
Follow-up X-rays were analyzed after 1 year from surgery to highlight any losses of fracture reduction, the consolidation progress and any early complications. In agreement with the Lidström scale [27], post-operative X-rays and final X-rays were examined by measuring radius height, radial slope angle and volar tilt angle of the radius using standard contralateral wrist X-ray’s as a comparator [28]. One-way analysis of variance (ANOVA-1) was used to determine whether the plate maintained bone reduction in complex fractures following early mobilization, considering a statistical significance at P < 0.05.
Results
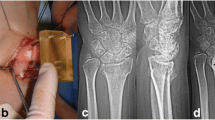
Of 48 patients included in this study, 20 (41.6%) were males and the mean age of the study group was 52.5 years (range 25–82 years). Mean follow-up was 26 months (range 12–36 months). According to the AO classification (Fig. 1), fractures were divided as follows: 16 were Type C1, 21 were Type C2 (Figs. 2, 3, 4) and 11 were Type C3. Thirty-two (66.7%) patients sustained a fracture after a fall on an outstretched hand and 16 (33.3%) patients were involved in a road accident. In all cases a volar approach osteosynthesis [17, 18] under X-ray control was done using the DVR plate.
The final step of the surgery consisted of reinserting the pronator quadratus which allowed to cover the plate. In no case was the carpal tunnel released. In adjunct to DVR plates in eight cases two Kirschner wires were used to stabilize distal ulnar epiphysis fractures, and in one case two cannulated screws were inserted in the radius metaphysis to obtain fragment compression. Post-operative immobilization was ensured through a volar univalve cast held in place for 15 days before rehabilitation. Rehabilitation was done by a single therapist (ST) and consisted of unrestricted early active wrist motion in warm water, non-resistive exercises for the hand and wrist, and functional electrical stimulation (FES) for approximately 10–15 days once bone callus formation was visible on X-ray. Self-managed wrist passive stretchings were added after this period, and strengthening exercises were added a week after this step to reinforce finger and wrist muscles. Scar massage began 24–48 h following suture removal or later if patients were referred later. In general, 2–3 therapy sessions per week were done for approximately 4–8 weeks of rehabilitation from the time of rehabilitation admission.
All fractures healed following a mean time of 2.6 months from the surgery (range 1.8–4.2 months). Mean DASH score was 43.5/100 (range 16/100–80/100) for the first section of the questionnaire, 26.5/100 for the second section (range 12.5/100–87.5/100) and 28.5/100 for the third section (range 12.5/100–87.5/100). A general DASH score was unavailable since some subjects omitted some sections of the questionnaire. Mean MMWS score was 82.5 (range 25–100). Six cases (12.5%) scored poorly, 6 (12.5%) scored satisfactory, 12 (27%) scored good and 24 (50%) scored excellent (Fig. 5). Final mean ROM of the wrist was 60.5° in flexion (range 40–90°), 62.5° in extension (range 25–90°), 40° in radio-ulnar deviation (range 25–55°). Final mean ROM of the forearm was 88° in pronation (the range 70–90°) and 83° in supination (range 45–90°). Final mean grip strength of the affected hand was 14.9 kg (range 7–40 kg) and represented 85% of the contralateral side.
The Lidström scale values assessed on X-rays after bone consolidation were as follows: 2 (4.2%) poor results, 7 (14.6%) sufficient, 24 (50%) good and 15 (31.2%) excellent (Fig. 6). Mean radius height was 8.8 ± 3.7 mm (range 5–15 mm), mean radial slope was 22.4 ± 5.4° (range 17–30°) and mean volar tilt was 9.7 ± 4.1° (range 6–13°). The same measurements were made using post-operative X-rays. Mean radius height was 9.2 ± 3.4 mm (range 7–15 mm), mean radial slope was 23.2 ± 5.8° (range 19–31°) and mean volar tilt was 10.3 ± 3.8° (range 8–15°). No significant statistical differences (P > 0.05) were found for any of the above parameters between post-operatively and final follow-up values (Table 1).
Seven (14.6%) patients underwent a second surgery for associated capsulo-ligamentous lesions undiagnosed at the time of injury which averaged 11 months (range 4–15 months) from the first surgery. In four cases, there were central lesions of the triangular fibro-cartilaginous complex (TFCC) (Type 1A according to the Palmer classification) [29]. These patients referred pain on the ulnar side of the wrist despite no clinical signs of radio-ulnar instability, and were treated with arthroscopic shaving. The other three patients presented with Grade III scafo-lunate dissociations according to the Geissler classification [30] through post-operative X-ray observation. The lesions were confirmed by contrast-enhanced magnetic resonance imaging. In these patients a modified Brunelli open reduction tenodesis [31, 32] was performed following arthroscopy confirmation.
In only one single case, an excessively long DVR plate, which extended beyond the radius diaphysis, was removed in a Type C3 fracture at 1 year and 2 months from the surgery. No symptoms were reported by the patient, but removal was done as a precautionary measure since the subject was a professional motorcyclist (Figs. 7, 8).
Discussion
The treatment of distal radius fractures has drastically changed over the past 20 years. Abraham Colles’ [33] statement about a casted wrist that “in some remote point in time will regain once more its complete range of motion and it will be completely free from pain” can no longer be considered reliable. The same is true for the common belief that the wrist is less inclined to develop osteoarthritis following trauma because of its non-weight bearing purpose. As early as 1981, Brand [34] demonstrated that forearm flexor muscles, upon activation, transfer approximately 500 kg at the radio-carpal joint of the wrist.
It is for these reasons that the authors have widened their range of surgical treatments for distal radius fracture in their clinical setting in order to ensure the reconstruction of a congruent articular surface, a stable bone reduction and the recovery of maximum ROM and function.
The occasional use of external fixators and Kirschner wires did not prove to be sufficient in restoring and maintaining radius height, radial slope and volar tilt for complex distal radius fractures [35–37]. Instead, opting for an ORIF approach for this type of fracture ensures a more accurate reduction and a more stable and durable osteosynthesis. Low-profile angular stability volar plates tend to minimize soft tissue irritation (especially with tendons), and allows for accurate alignment of the distal radius and permits early mobilization of the wrist.
Dorsal or combined volar/dorsal accesses are less indicated, even for complex fractures of the distal radius. Most fractures can be managed through a single volar access despite the presence of dorsal fragments and obtain acceptable outcomes and good implant stability. Orbay and Osada et al. [14–16] have shown that clinical results, in terms of fracture healing, reduction preservation over time, ROM and function of the wrist and hand in patients with complex fractures of distal radius with dorsally displaced fragment, following volar plate osteosynthesis, were similar to subjects operated with dorsal plates [16] and that the volar hardware provided similar stability at the fracture site as the dorsal plate hardware [14, 15].
The osteosynthesis technique described in this study also represented a low-profile design which minimized shear forces against tendinous and vasculo-nervous structures, and resulted in 48 satisfactory cases following complex fractures of the distal radius. The high tolerability properties of this plate are confirmed by the fact that none of the patients treated so far required hardware removal. In one case an excessively long DVR plate, which extended beyond the radius diaphysis, was removed in a Type C3 fracture at 1 year and 2 months from the surgery. No symptoms were reported by the patient, but removal was done as a precautionary measure since the subject was a professional motorcyclist.
The DVR plate also owns biomechanical properties of fixation that guarantee an excellent stability of the synthesis, even in comminuted fractures and severe articular fractures (Type C2 and C3 fractures of the AO classification) [19, 20]. In fact, the analysis of this study’s results do not show significant secondary losses of the radius with respect to height, radial slope and volar tilt, which are common complications in these types of fracture. The surgical reduction remained the same over time, and the differences between the X-ray parameters measured immediately following surgery and at final follow-up were not statistically significant.
The authors believe that the DVR plate holds specific biomechanical properties of fixation due to its distal positioning of screws and pegs which lie over a subchondral zone at the distal portion of the system. Distal locking can be done with smooth pegs or with screws partially or completely threaded inserted in a double row of holes. In particular, the pegs serve the purpose of stabilizing the subchondral bone while the threaded screws “capture” the dorsal fragment and compress it against the radius. The layout of screws/pegs fan out on a frontal plane. The two rows of holes allow the screws and pegs from one row to cross over the other row, thus forming a kind of 3D subchondral meshed support for the distal articular surface. The screws and pegs form a predetermined angle of 12° with respect to the plate and their radial divergence allows for the fixation of the radial styloid. From of a technical point view, Drobetz [38] demonstrated that the precise distal positioning of the pegs and screws within the radial epiphysis in the subchondral zone significantly increases the synthesis stability of the fracture in comparison to a more proximal positioning. The results in the present study also seem to confirm Drobetz’s findings. Radiograph parameters changed considerably in six of the authors’ patients treated with pegs and screws that were positioned too proximally.
There were little complications with this surgical device and they were all due to technical mistakes. Although the DVR plate fixation system has a low level of difficulty, a learning curve is still warranted in correctly placing the plate. Orbay [16] showed that the long-term results of this type of fracture depend on the quality of the reduction at the time of surgery and the stability preserved over time. In the authors’ experience, the worst outcomes were observed in those patients who presented poor X-ray parameters immediately following surgery (height, radial slope and volar tilt).
It is well documented that prognosis and outcome of intra-articular fractures of the distal radius depend also on the presence of associated injuries such as capsular, ligamentous and cartilaginous lesions of the wrist [39–46]. The literature reports 6–78% [31] of the cases have associated partial or complete lesions of the TFCC, but most studies report 30–40% of the cases [47–51]. Associated intra-carpal ligament lesions are just as frequent with varying incidence, from 25 to 56% according to the different series found in the literature [30, 48–50], with a clear prevalence of partial or complete lesions of the scapho-lunate and luno-triquetral ligaments. Unfortunately, complex wrist fractures are difficult to evaluate in full detail through imaging at the time of injury, and thus these ligamentous lesions remain undiagnosed at the time of admission. Arthroscopy could be of assistance in the diagnostic process and for early treatment of these associated insidious lesions, although this procedure is not a common practice in treating acute complex fractures.
Conclusions
Angular stability volar plates are an excellent mean of synthesis for comminuted and articular fractures of the distal radius (Type C of the AO classification).
According to this study, the DVR plate ensures an excellent stability for these comminuted fractures as anatomical reduction is always warranted in order to obtain good functional results. To reach this aim, arthroscopic reduction may be of assistance.
This plate is well tolerated because of its low profile anatomy which reduces soft tissue friction and the necessity of hardware removal after bone consolidation.
References
Graff S, Jupiter J (1994) Fracture of the distal radius: classification of treatment and indications for external fixation. Injury Suppl 25(4):D14–D25
Muller ME, Nazarian S, Koch P, Schatzker J (1990) The comprehensive classification of fractures of long bones. Springer, Berlin
Leung F, Zhu L, Ho H, Lu WW, Chow SP (2003) Palmar plate fixation of AO TYPE C2 fracture of distal radius using a locking compression plate. A biomechanical study in a cadaveric model. J Hand Surg Br 28:263–266
McQueen M, Caspers J (1988) Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br 70:649–651
Fernandez DL (1993) Fractures of the distal radius: operative treatment. Instr Course Lect 42:73–88
Bradway JK, Amadio PC, Cooney WP (1989) Open reduction and internal fixation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am 71(6):839–847
Weber SC, Szabo RM (1986) Severely comminuted distal radial fracture as an unsolved problem: complications associated with external fixation and pins and plaster techniques. J Hand Surg Am 11(2):157–165
Axelrod TS, McMurtry RY (1990) Open reduction and internal fixation of comminuted, intra-articular fractures of the distal radius. J Hand Surg Am 15(1):1–11
Carter PR, Frederick HA, Laseter GF (1997) Open reduction and internal fixation of unstable distal radius fractures. J Hand Surg Am 22:777–784
Rikli DA, Regazzoni P (1996) Fractures of the distal end of the radius treated by internal fixation and early function. A preliminary report of 20 cases. J Bone Joint Surg Br 78:588–592
Kambouroglou GK, Axelrod TS (1998) Complications of the AO/ASIF titanium distal radius plate system (pi plate) in internal fixation of the distal radius: a brief report. J Hand Surg Am 23:737–741
Jupiter JB (1991) Current concepts review: fractures of the distal end of the radius. J Bone Joint Surg Am 73:461–469
Ring D, Jupiter JB, Brennwald J, Büchler U, Hastings H 2nd (1997) Open reduction and internal fixation of unstable distal radius fractures. J Hand Surg Am 22:777–784
Osada D, Viegas SF, Shah MA, Morris RP, Patterson RM (2003) Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg Am 28:94–104
Liporace FA, Kubiak EN, Jeong GK, Iesaka EgolK, Koyal KJ (2006) A biomechanical comparison of two volar locked plates in a dorsally unstable distal radius fracture model. J Trauma 61:668–672
Orbay JL, Touhami A (2006) Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res 445:58–67
Orbay JL, Badia A, Indriago IR, Infante A, Khouri RK, Gonzalez E, Fernandez DL (2001) The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg 5(4):204–211
Henry MH, Griggs SM, Levaro F, Clifton J, Masson MV (2001) Volar approach to dorsal displaced fractures of the distal radius. Tech Hand Up Extrem Surg 5:31–41
Orbay JL, Fernandez DL (2002) Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am 27(2):205–215
Orbay JL, Fernandez DL (2004) Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am 29(1):96–102
Rossi G, De Sessa F, Ivaldi M (2007) Risultati nell’utilizzo delle placche DVR-A nel trattamento delle fratture instabili del radio distale. Riv Chir Man 1:27–31
Tarallo L, Adani R, Amorico MG, Spagni A, Salento A (2008) The treatment of articular wrist fractures with hand innovation plate. GIOT 34:53–57
Padua R, Padua L, Ceccarelli E, Romanini E, Zanoli G, Amadio PC, Campi A (2003) Italian version of disability of the arm shoulder and hand (DASH) questionnaire. cross-cultural adaptation and validation. J Hand Surg Br 28:179–186
Cooney WP, Bussey R, Dobyns JH, Linscheid RL (1987) Difficult wrist fractures. Perilunate fracture-dislocation of the wrist. Clin Orthop 214:136–147
Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL (1989) Scaphoid malunion. J Hand Surg Am 14(4):679–687
American Society of Hand Therapists (ASHT) (1992) Clinical assessment recommendations, 2nd edn. Chicago
Lidström A (1959) Fractures of the distal end of the radius. A clinical and statistical study of end results. Acta Orthop Scand Suppl 41:1–118
van Eerten PV, Lindeboom R, Oosterkamp AE, Goslings JC (2008) An X-ray template assessment for distal radial fractures. Arch Orthop Trauma Surg 128:217–221
Palmer AK (1989) Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am 14:594–606
Geissler WB, Freeland AE, Savoie FH (1996) Intracarpal soft tissue lesions associated with an intraarticular fracture of the distal end of the radius. J Bone Joint Surg Am 78:357–365
Brunelli GA, Brunelli GR (1995) A new surgical technique for carpal instability with scapho-lunate dislocation. Ann Chir Main Memb Super 14:207–213
Garcia-Elias M, Lluch AL, Stanley JK (2006) Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am 31(1):125–134
Colles A (1814) On fracture of the carpal extremity of the radius. Edinburgh Med Surg 10:182–186
Brand PW, Beach RB, Thompson DE (1981) Relative tension and potential excursion of muscles in the forearm and hand. J Hand Surg Am 6(3):209–219
Cooney WP (1983) External fixation of distal radial fractures. Clin Orthop Relat Res 180:44–49
Seitz WH Jr, Froimson AI, Leb R, Shapiro JD (1991) Augmented external fixation of unstable distal radius fractures. J Hand Surg Am 16:1010–1016
Sanders RA, Keppel FL, Waldrop JI (1991) External fixation of distal radial fractures: results and complications. J Hand Surg Am 16:385–391
Drobetz H, Bryant AL, Pokorny T, Spitaler R, Leixnering M, Jupiter JB (2006) Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction: a biomechanic study in a cadaveric model. J Hand Surg Am 31(4):615–622
Hardy P, Gomes N, Chebil M, Bauer T (2006) Wrist arthroscopy and intra-articular fractures of the distal radius in young adults. Knee Surg Sports Traumatol Arthrosc 14:1225–1230
Ruch DS, Vallee J, Poehling GG, Smith BP, Kuzma GR (2004) Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy 20(3):225–230
Metha JA, Bain GI, Heptinstall RJ (200) Anatomical reduction of intra-articular fractures of the distal radius. J Bone Joint Surg Br 82:79–86
Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H (1999) Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am 81:1093–1110
Kamano M, Koshimune M, Kazuki K, Honda Y (2005) Palmar plating for AO ASIF C3.2 fractures of the distal radius with arthroscopically assisted reduction. Hand Surg 10(1):71–76
Fernandez DL, Geissler WB (1991) Treatment of displaced articular fractures of the radius. J Hand Surg Am 16:375–384
Knirk JL, Jupiter JB (1986) Intraarticular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 68:647–658
Edwards CC II, Harasztic J, McGillivary GR, Gutow AP (2001) Intraarticular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am 26:1036–1041
Richards RS, Bennett JD, Roth JH, Milne K Jr (1997) Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am 22(5):772–776
Cognet JM, Bonnomet F, Ehlinger M, Dujardin C, Kempf JF, Simon P (2003) Controle arthroscopique dans le traitement de fractures articulaires du radius distal: a propos d’une serie de 16 cas. Rev Chir Orthop Reparatrice Appar Mot 89(6):515–523
Mathoulin C, Sbihi A, Panciera P (2001) Interet de l’arthroscopie du poignet dans le traitement de fractures articulaires du ¼ inferieur du radius: a propos de 27 cas. Chir Main 20(5):342–350
Chen AC, Chan YS, Yuan LJ, Ye WL, Lee MS, Chao EK (2002) Arthroscopically assisted osteosynthesis of complex intra-articular fractures of the distal radius. J Trauma 53(2):354–359
Shih JT, Lee HM, Hou YT, Tan CM (2001) Arthroscopically-assisted reduction of intra-articular fractures and soft tissue management of distal radius. Hand Surg 6(2):127–135
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frattini, M., Soncini, G., Corradi, M. et al. Complex fractures of the distal radius treated with angular stability plates. Musculoskelet Surg 93, 155–162 (2009). https://doi.org/10.1007/s12306-009-0035-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-009-0035-1