Abstract
Chronic Lead (Pb) exposure is associated with disrupting certain endocrine levels and is referred to as an endocrine disruptor. Thyroid hormones, involved in regulating numerous physiological functions, are reported with conflicting associations with chronic Pb exposure. This study broadly evaluated the association between long-term lead exposure and thyroid function parameters. In this systematic review, the observational studies documenting the changes in thyroid function parameters between the chronically Pb-exposed and controls were systematically identified from PubMed-Medline, Scopus, and Embase digital databases from the beginning to March 31, 2022. The protocol was previously registered with PROSPERO (ID: CRD42022315520) and executed following PRISMA 2020 guidelines. The random-effects model was used to analyze the mean differences in thyroid function parameters between groups. The classical I2 statistic was applied to assess heterogeneity, while the Newcastle Ottawa Scale was used to assess the risk of various biases. Where data allowed, sub-group, sensitivity, and meta-regression analyses were carried out. The current systematic review included fifteen observational studies. The Pb-exposed have a higher mean blood Pb level [i.e. 28.07 (95% CI 21.43–34.72) µg/dl], significantly higher free T3 [(i.e. 0.48 pg/dl (95% CI 0.05–0.95)] and trend of higher T3. T4, FT4, and TSH levels than controls with high heterogeneity (I2 > 85%). Considering the important role of thyroid hormone in multiple biological functions, the present findings emphasize the requisite for high-quality studies to investigate the association between levels of thyroid function parameters among individuals known for cumulative exposure to Pb.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lead (Pb), a common heavy metal pollutant, is associated with multiple systemic disorders and diseases on chronic exposure. Recent evidence suggests the role of Pb as an endocrine disruptor because of its association with changes in the levels of vitamin D, prolactin, and others [1]. Subclinical thyroid function aberrations on chronic Pb exposure are speculated as well. Thyroid hormones (T4 and T3) are secreted by the thyroid gland's follicular cells and regulated centrally by TSH (Thyroid Stimulating Hormone) released from the pituitary gland. These hormones interact with the majority of the physiological systems, including the metabolism of protein, carbohydrates, and lipids and regulating bone growth (synergy with growth hormone), neural maturation, and many more. Therefore, aberrations in thyroid function may potentially affect multiple physiologic regulations and their functions.
The primary literature on the association between blood Pb levels and thyroid functions is inconsistent with contrasting observations, thereby inconclusive. A recent systematic review observed no association between occupational Pb exposed men and changes in thyroid hormone levels/functions [2]. The observations from the cited systematic review were drawn from primary studies recruiting patients with clinical conditions such as male infertility, musculoskeletal, neurological, gastrointestinal, and other symptoms [3, 4], and those studies investigating only Pb exposed group (without comparative control group) [5,6,7,8,9] in addition to observational comparative studies (i.e. studies comparing occupational Pb exposed against the controls). In addition to the studies mentioned above, few recent studies report a significant association between chronic Pb exposure and aberrations in thyroid function [10,11,12], thereby requiring an update in this field. Because of the inconsistent reports and addition of recent literature with contrasting observations, the present updated systematic review aims to comprehensively investigate the association between long-term Pb exposure and thyroid functions by pooling the existing evidence from primary literature reporting the thyroid function changes among apparently healthy adults with occupational Pb exposure as compared to those without apparent occupational Pb exposure.
Methods
The study employed PRISMA (Preferred Reporting Items of Systematic reviews and Meta-Analysis) guidelines to systematically review the existing evidence on changes in thyroid function parameters among otherwise healthy adults with occupational exposure to Pb compared to those without an obvious history of occupational exposure to Pb [13]. Details of the study proposal were earlier digitally registered (PROSPERO ID: CRD42022315520) [14]. Thyroid function parameters such as thyroid Stimulating Hormone (TSH), Triiodothyronine (T3), Thyroxine (T4), and thyroid releasing hormone (TRH) were primarily investigated, while free thyroxine (FT4), free triiodothyronine (FT3), anti-thyroid antibody (Anti-T3/4 Ab) and thyroid peroxidase were secondarily considered for the review. Observational studies of either cross-sectional or longitudinal design evaluating the above-listed thyroid parameters among occupationally Pb-exposed participants as against those without obvious Pb exposure were systematically searched using pre-validated search terms from Embase, Scopus, and Pubmed digital sources from their time of inception to March 31, 2022. The search terms were developed using the conventional PECOS approach, i.e. Participants, Exposure (i.e. occupational Pb exposure), Controls (no apparent occupational Pb exposure), Outcome (thyroid function parameters listed earlier), and Study design. Strategies to maximize the precision and sensitivity of the search were adopted. Detailed search strategies and the search words/ terms used in the current study are described in supplement Tables 1–3. A lateral search using the bibliography of included studies for potential studies was attempted. Studies with preclinical models (i.e. animal/cell line), those reporting observations by involving patients with symptomatic Pb poisoning or seeking healthcare services or individuals with congenital/acquired disorders of thyroid metabolism or other endocrine disturbances or review, commentaries, letters to the editors, editorials and methodology articles were excluded from the review.
Screening and Reviewing of Studies
Studies were screened and reviewed according to existing standard published methods [15, 16]. Briefly, all-digital records were pooled and independently screened using the cloud-based “Rayyan intelligent systematic review” (RB, KU, and AV) [17]. The full text of identified records was independently reviewed (RB, KU, and AV), and relevant data were extracted from records meeting the inclusion–exclusion criteria. All conflicts during the independent review were resolved by mutual consensus.
Data Collection, Extraction, Analysis, and Management
Briefly, a data extraction (Google sheets) sheet including details of the participants (sample size, age, gender, and duration of employment), occupation/workplace (nature of workplace, location, simultaneous exposure to other heavy metals), outcome measures, in addition to details of the article (title, year of publication, journal, authors and contact details of the corresponding author) were extracted, wherever available.
Central tendency values and data dispersion for the outcome parameters were independently extracted from all included studies. Standard conversion factors were used to convert outcome parameters reported in unconventional/non-standard units to the standard units. The Pb and thyroid function parameters units were converted to the SI units, i.e. mg/dL, μg/dL, ng/dL and pg/dL [18]. The reports were recorded as mean and standard deviation for uniform reporting using conventional transformations [19]. Lastly, for studies [11, 12] reporting more than one exposed group, the grand mean was estimated and used for the current quantitative analysis [20]. Pooled mean difference (95% CI) between the two groups was estimated using the generic inverse variance method by pooling the mean and SD from individual studies. A random-effects model was employed during the meta-analysis in anticipation of high heterogeneity.
Heterogeneity, Meta-Regression, Sensitivity, and Subgroup Analysis
The assessment and interpretation of heterogeneity among studies, subgroup (if more than two primary studies were available in the particular subgroup), sensitivity, and meta-regression (if more than nine primary studies were available) analyses were executed using conventional methods [14, 15]. The present study regarded I2 > 25% or Cochrane-Q < 0.1 as evidence of heterogeneity among the included studies. Funnel and contour-enhanced funnel plots were employed to explore the potential sources of heterogeneity when > 10 studies were available [21, 22]. Asymmetric funnel plots or significant (p < 0.05 on Eggers test) were regarded as evidence for the potential publication bias among the studies.
Data were analyzed using Stata version 16 [23]. All results with two-sided p < 0.05 were considered statistically significant except for the subgroup analysis, wherein p < 0.10 were considered significant.
Assessment of the Risk of Bias in Included Studies
Newcastle Ottawa scale (NOS) was employed independently by the authors to assess the risk of bias in the included studies [24]. The authors developed an SOP specific to the present review to assess the risk of bias among the included studies, as guided by OHRI NOS (description available in the supplement material). Briefly, the tool is used to rate the risk of bias during participant selection, whether the cases and controls are comparable, and assess the exposure. Based on clarifying the definition of cases and controls, their representativeness and comparability, and the exposure assessment, individual studies are rated with star(s).
Results
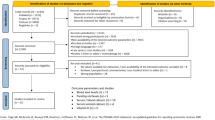
The electronic search identified 4250 studies. On excluding the duplicates, screening of abstracts and titles resulted in 23 studies suitable for full-text review. Fifteen studies finally qualified all the inclusion and exclusion criteria for data extraction and review. The reasons for exclusion along with the number of studies excluded at each phase are described in the PRISMA flowchart (Fig. 1 and supplement Table 2).
Description of Studies
Details such as sample size, the mean age of the participants, duration of occupational exposure, type of industry, and outcome parameters reported in the individual studies are described in Table 1. The outcome variables of both exposed and control groups in the majority of included studies were within the recommended normal values (i.e. TSH: 0.5–5 mIU/L, total T3: 80–220 ng/dL, total T4: 5–12 µg/dL and free T4: 0.7–1.9 ng/dL). However, the mean thyroxine levels of both Pb exposed and controls from Akbal et al. [25] and the mean free thyroxine level of controls from Dursun and Ahmad [26] were lower than the recommended values. Genart et al. [27, 28] reported the free thyroxine index as the substitute for the free thyroxine level, wherein the normal range is 1.1–4.3 ng/dL. None of the included studies reported the exclusion of participants with hyper/hypothyroidism based on thyroid antibody and thyroid peroxidase values. Briefly, the occupationally exposed group were employed at Pb battery and its allied industries, foundries, e-waste recycling process, welding, automobile, smelting, and paint industries. The mean duration of occupational Pb exposure ranged from 2.5 to 22 years. The studies were restricted to Latin American (Argentina, Columbia), North American (Canada, southeastern USA), Asian (India), European (Turkey, Sweden, Belgium), and African (Egypt) countries. In contrast, no studies from Australia and vast regions of Africa or Asia were available.
Risk of Bias Assessment
The risk of bias in participant selection, exposure assessment, and outcome parameters was performed using NOS (OHRI) (Table 2). Most studies reported the exposed and control population based on the participant's history of thyroid dysfunction, however, lacked documented evidence of their previous thyroid hormone levels, thereby these studies were identified with a high risk of bias in participant selection. Apart from Schumacher et al., all included studies involved comparable study and control groups for the analysis of blood Pb levels and (the exception being Zaidi et al.) [11, 29] thyroid-related parameters. Because of including the observational studies, the interviewer and the participants from all studies were potentially aware of their respective participant’s exposure and participation status, as either exposed or control. As the awareness among the interviewer and or the participant could potentially bias the exposure assessment in these studies, none of the included studies could be compared with that of well-designed randomized controlled trials.
Results of Individual Outcome Parameters
Blood lead levels Present study identified twelve studies describing the BLL among occupationally Pb-exposed and control workers [10, 11, 25, 26, 28, 30,31,32,33,34,35,36,37]. The majority of identified studies reported significantly (p < 0.05) higher BLL among the Pb-exposed group as compared to their respective comparative control group. The results were in line with the current pooled quantitative analysis, wherein individuals with occupational Pb exposure exhibited a mean BLL of 28.07 μg/dL (95% CI 21.43 to 34.72, I2 = 99.76%, p < 0.01) higher as compared to the control group. (Fig. 2). Subgroup analysis, involving studies that recruited participants with a history of simultaneous occupational exposure to other heavy metal(s), did not alter the results (Supplement Fig. 1). Additionally, the meta-regression with participants’ age as well did not significantly reduce the heterogeneity/alter the results. Further, the funnel plot shows asymmetry is suggestive of publication bias (p < 0.01); the contour-enhanced funnel plot suggests the presence of other biases as well (supplement Fig. 2).
Forest plot for the association between occupational Pb exposure and Blood lead levels. Legends/footnotes Forest plot revealing the group mean differences of blood lead levels (BLL) in µg/dL between the occupationally Pb exposed workers and control participants (i.e. without obvious Pb exposure). The square and whisker (horizontal lines) represent respectively the mean difference and 95% confidence interval of individual studies. The length and width of the diamond indicate the pooled mean difference and 95% confidence interval derived from random-effect analysis
Serum Thyroid-Stimulating Hormone (TSH)
All but Bledsoe et al. [10,11,12, 25, 26, 28, 29, 31,32,33,34,35,36,37] reported thyroid-stimulating hormone (TSH) levels for both occupationally Pb exposed and those without obvious occupational Pb exposure. The majority (Nine) of these studies reported relatively higher TSH among the occupationally Pb-exposed workers as compared to the control participants, while five (5) of the studies reported statistically significant differences (p < 0.05) [10, 12, 29, 36, 37]. The pooled mean difference between the duo revealed 0.25 mIU/L (95% CI − 0.04 to 0.54, I2 = 88.45%), with a trend of higher TSH levels but statistically not significant (i.e. p > 0.05) among the occupational Pb exposed group (Fig. 3). On subgroup analysis, by pooling results of studies involving participants with a history of simultaneous exposure to additional heavy metals did not affect the heterogeneity or change the direction of results (Supplement Fig. 3). Meta-regression, including the participant’s age, did not affect the results. Although the Egger’s test (p = 0.09) is not significant, the asymmetric funnel plot is suggestive of publication bias; the contour-enhanced funnel plot also suggests the presence of other biases. (Supplement Fig. 4).
Forest plot for the association between occupational Pb exposure and levels of thyroid-stimulating hormones (TSH). Legends/footnotes Forest plot revealing the group mean differences in levels of TSH in mIU/L between the occupationally Pb exposed workers and control participants. The square and whisker (horizontal lines) represent respectively the mean difference and 95% confidence interval of individual studies. The length and width of the diamond indicate respectively the pooled mean difference and 95% confidence interval derived from random-effect analysis
Serum Total Triiodothyronine (T3)
Six (6) of the included studies reported total serum triiodothyronine levels [26, 28, 33,34,35, 37]. All studies reported marginally higher T3 among the exposed group, while none of these studies observed statistical significance. The pooled mean difference revealed non-significant differences between the groups (0.11 ng/dL with 95% CI − 0.23 to 0.44 and I2 = 0%) (Fig. 4a). The results suggest higher T3 levels (but statistically not significant) among the occupationally Pb-exposed workers compared to the non-exposed control participants. Subgroup and meta-regression analyses and funnel plots weren’t taken up because of fewer available studies.
Forest Plot for group differences in triiodothyronine (A) and thyroxine (B) between the occupationally Pb exposed and control workers. Legends/footnotes Forest plot revealing the group mean differences in triiodothyronine in ng/dL (A) and thyroxine in µg/dL (B) between the occupationally Pb exposed workers and control participants. The square and whisker (horizontal line) represent respectively the mean difference and 95% confidence interval of individual studies. The length and width of the diamond indicate respectively the pooled mean difference and 95% confidence interval derived from random-effect analysis
Serum Total Thyroxine (T4)
Nine (9) of the included studies reported total thyroxine (T4) levels; all but Singh et al. (2000), Schumacher et al. and Bledsoe et al. [11, 25, 26, 28, 30, 33,34,35, 37] observed higher serum T4 levels among the occupational Pb-exposed group as compared to the control group. Two of these studies observed statistical differences (p < 0.05) [26, 35]. The pooled mean difference between the two groups was 0.44 μg/dL (95% CI − 0.06 to 0.94, I2 = 94.15%) with high heterogeneity (Fig. 4b). The results suggest higher T4 levels (but statistically not significant) among the occupational Pb-exposed group, compared to the non-exposed control group. Subgroup analysis by pooling studies involving participants with a history of simultaneous exposure to additional heavy metals did not significantly reduce the heterogeneity or change the direction of results (Supplement Fig. 5). Meta-regression analyses and funnel plots weren’t taken up because of fewer available studies.
Serum-Free Triiodothyronine (FT3)
Seven studies among those considered for this review reported FT3, and four (4) of these studies observed higher FT3 while two (2) reported statistical significance (p < 0.05) among the Pb exposed group as compared to the non-exposed group [10, 12, 26, 31,32,33, 36]. The pooled mean difference between the two (2) groups was 0.48 pg/dL (95% CI 0.05–0.91, I2 = 95.33%) with high heterogeneity (Fig. 5a). The results indicate significantly higher FT3 point estimates among Pb-exposed. Subgroup analysis by pooling studies of those involved participants with a history of additional exposure to other heavy metals did not significantly alter the heterogeneity or affect the direction of results (Supplement Fig. 6). Due to the fewer studies, meta-regression analysis and funnel plots were not executed.
Forest Plot for group differences in free-triiodothyronine (A) and free-thyroxine (B) between the occupationally Pb exposed and control workers. Legends/footnotes Forest plot revealing the group mean differences in free-triiodothyronine in ng/dL (A) and free-thyroxine in µg/dL (B) between the occupationally Pb exposed workers and control participants. The square and whisker (horizontal line) represent respectively the mean difference and 95% confidence interval of individual studies. The length and width of the diamond indicate respectively the pooled mean difference and 95% confidence interval derived from random-effect analysis
Serum-Free Thyroxine (FT4)
Eleven (11) of the included studies reported free thyroxine (FT4) levels, with four (4) of them reporting higher FT4 levels among Pb exposed, with three (3) observing statistical significance [10,11,12, 26, 28, 30,31,32,33, 35, 36]. The pooled mean difference between the duo was 0.18 ng/dL (95% CI − 0.11 to 0.47, I2 = 98.88%) with high heterogeneity (Fig. 5b). The results indicate that despite the point estimate of the effect measure of FT4 was marginally higher among occupational Pb-exposed, the results were statistically not significant (p > 0.05). Subgroup analysis by pooling results of studies involving participants with a history of simultaneous exposure to additional heavy metals at the workplace (Supplement Fig. 7) or the meta-regression with participant’s age did not significantly reduce the heterogeneity or alter results. Further, the funnel plot shows asymmetry suggestive of publication bias (p for Egger’s test is 0.59); the contour-enhanced funnel plot also suggests the presence of other biases. (Supplement Table 8).
Discussion
Existing primary literature investigating the associations between occupational Pb exposure and changes in thyroid function parameters were systematically reviewed by following the PRISMA guidelines. Primary studies comparing the thyroid function parameters of apparently healthy adults with occupational (chronic) Pb exposure and controls with no history of obvious occupational Pb exposure were included in the systematic review. The occupationally Pb-exposed group exhibited relatively higher TSH, T3, T4, FT3, and FT4 levels as compared to the control group. However, the change in FT3 alone was statistically significant. To note, high levels of heterogeneity were observed among the primary studies included in the review, and the permissible analyses, viz. subgroup and/or meta-regression to detect the sources of heterogeneity or modify the results were inconclusive.
The Pb-exposed group consistently exhibited significantly higher blood Pb levels across all included studies, irrespective of the occupation and duration of exposure. The control group, although without obvious Pb exposure as well had Pb in their blood, however at levels significantly lower than the exposed group. Despite the fact that Pb has no known physiological function in humans, the CDC (Center for Disease Control) released the reference BLL as < 10 μg/dl for the general population (i.e. adults without occupational Pb exposure) in the “Adult Blood Lead Epidemiology and Surveillance” program, based on the population Pb levels recorded [38, 39]. The mean BLL of the control group of two of the included studies was > 10 μg/dL [10, 28]. Due to the extensive Pb usage in the recent past as additives in paints, plumbing, fuel, and other sources, Pb persists in the environment and is potentially responsible for the lead in the blood of the control group. Considering Pb’s no known physiological role in humans and its potentially hazardous nature, all potential sources of environmental Pb exposure should be investigated, and control plans should be initiated for seizing any further exposure.
Pooled results reveal a trend of higher T3, T4, free T4, and TSH among occupationally Pb exposed as compared to the control group. While free T3 was significantly higher among the Pb-exposed group. However, given the high heterogeneity among the primary literature (I2 > 95%) and potential high publication biases (revealed by funnel plots and contour-enhanced funnel plots), current observations mandate cautious interpretation. Further, due to the availability of fewer primary literature, meta-regression and subgroup analyses were restricted for fewer outcome parameters.
Recent evidence suggests the possible role of Pb as an endocrine disruptor affecting the central (i.e. via hypothalamic-pituitary)—peripheral (i.e. endocrinological) axis. Recent systematic reviews independently reported the association between Pb exposure and elevation in prolactin levels and Pb exposure and the trend of reducing vitamin D levels [15, 16]. In similar lines, the imbalance in thyroid hormone levels among the Pb-exposed individuals were speculated to be mediated via altering the central axis (viz. hypothalamic–pituitary–thyroid axis) [2, 26, 37], affecting the equilibrium between protein-bound and free thyroid hormone [30] either by inhibiting the enzyme synthesis by inducing oxidative stress, cellular membrane damage [36] or other possible mechanisms. Current literature concerning chronic Pb exposure and its association with changes in thyroid hormone levels is restricted to free and total T3 and T4, and TSH. Hence, there is a need to investigate the other potential mechanisms listed earlier to confirm any association between chronic Pb exposure and changes in thyroid function. However current evidence suggests a trend but the non-significant association between chronic Pb exposure and changes in the identified thyroid function parameters.
The present study systematically reviewed the association between chronic Pb exposure and thyroid function by comprehensively including all the available thyroid function parameters. Current observations were in a similar direction to the earlier systematic review reports despite additionally pooling observations from recent primary studies [2]. Present results are to be cautiously interpreted with the background of limitations associated with systematically pooling individual observations from the primary studies, viz., absence of high-powered studies, heterogeneity among them, non-uniform reporting, and others. Further, the present systematic review included studies of observational and cross-sectional designs, with inherently high levels of risk of bias, fewer primary studies available for meta-regression, sub-group, and sensitivity analyses, and pooled mean differences with wide confidence intervals.
Conclusions
Current literature on the association between long-term Pb exposure and thyroid function changes is restricted to the assessment of core clinical thyroid function assessments. Pooled evidence suggests a trend of association (however statistically not significant) between chronic Pb exposure and the routine clinical thyroid function parameters. Because of the limited evidence from high-quality studies and assessments evaluating the subclinical thyroid aberrations, future studies with longitudinal design and larger samples comprehensively investigating the subclinical thyroid aberrations (such as the thyroid releasing hormone, oxidative stress, integrity of cellular membranes, and others if any) is warranted. Though the current study lacks strong support for the association between the duos, a precautionary periodic screening of thyroid function parameters is suggested among the chronic Pb-exposed for early detection and initiating appropriate action.
References
Ahamed M, Siddiqui MK. Low level lead exposure and oxidative stress: current opinions. Clin Chim Acta. 2007;383(1–2):57–64. https://doi.org/10.1016/j.cca.2007.04.024.
Krieg EF Jr. A meta-analysis of studies investigating the effects of occupational lead exposure on thyroid hormones. Am J Ind Med. 2016;59(7):583–90. https://doi.org/10.1002/ajim.22591.
Cullen MR, Kayne RD, Robins JM. Endocrine and reproductive dysfunction in men associated with occupational inorganic lead intoxication. Arch Environ Health. 1984;39(6):431–40. https://doi.org/10.1080/00039896.1984.10545877.
Yilmaz H, Keten A, Karacaoglu E, Tutkun E, Akcan R. Analysis of the hematological and biochemical parameters related to lead intoxication. J Forensic Leg Med. 2012;19(8):452–4. https://doi.org/10.1016/j.jflm.2012.04.001.
Andrzejak R, Antonowicz J, Bolanowska B, Hebdzinski L, Kabacinska-Knapik D, Smolik R. Thyroid function in smelters after long-term exposure to heavy metals. Med Pr. 1996;47(3):253–8.
Bielecka W, Frydrych J, Wojtas A. Thyroxine (T4) levels in workers exposed to lead. Med Pr. 1987;38(1):40–4.
Horiguchi S, Endo G, Kiyota I. Measurement of total triiodothyronine (T3), total thyroxine (T4) and thyroid-stimulating hormone (TSH) levels in lead-exposed workers. Osaka City Med J. 1987;33(1):51–6.
Robins JM, Cullen MR, Connors BB, Kayne RD. Depressed thyroid indexes associated with occupational exposure to inorganic lead. Arch Intern Med. 1983;143(2):220–4.
Tuppurainen M, Wagar G, Kurppa K, Sakari W, Wambugu A, Froseth B, et al. Thyroid function as assessed by routine laboratory tests of workers with long-term lead exposure. Scand J Work Environ Health. 1988;14(3):175–80. https://doi.org/10.5271/sjweh.1934.
Fahim YA, Sharaf NE, Hasani IW, Ragab EA, Abdelhakim HK. Assessment of thyroid function and oxidative stress state in foundry workers exposed to lead. J Health Pollut. 2020;10(27):200903. https://doi.org/10.5696/2156-9614-10.27.200903.
Schumacher C, Brodkin CA, Alexander B, Cullen M, Rainey PM, van Netten C, et al. Thyroid function in lead smelter workers: absence of subacute or cumulative effects with moderate lead burdens. Int Arch Occup Environ Health. 1998;71(7):453–8. https://doi.org/10.1007/s004200050305.
Sherif MM, Mohammed YS, Zedan HAE-M, Kheder MAE-h, Mohammed AHAE-S. Toxic effect of some heavy metals (cadmium and lead) on thyroid function. Egypt J Hosp Med. 2017;69(5):2512–5.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Upadhyay K, Viramgami A, Balachandar R, Bagepally BS. Study the association between blood lead levels and thyroid function: an updated systematic review and meta-analysis. Prospero. 2022;CRD42022315520.
Balachandar R, Bagepally BS, Kalahasthi R, Haridoss M. Blood lead levels and male reproductive hormones: a systematic review and meta-analysis. Toxicology. 2020;443:152574. https://doi.org/10.1016/j.tox.2020.152574.
Upadhyay K, Viramgami A, Bagepally BS, Balachandar R. Association between blood lead levels and markers of calcium homeostasis: a systematic review and meta-analysis. Sci Rep. 2022;12(1):1850. https://doi.org/10.1038/s41598-022-05976-4.
Mourad O, Hossam H, Zbys F, Ahmed E. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:2–10. https://doi.org/10.1186/s13643-016-0384-4.
Christiansen S, Iverson C, Flanagin A. AMA manual of style: a guide for authors and editors. 2020 https://academic.oup.com/amamanualofstyle/si-conversion-calculator.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. https://doi.org/10.1186/1471-2288-5-13.
Altman DG, Bryant TN, Gardner MJ. Statistics with confidence. 2nd ed. BMJ Books; 2000.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. https://doi.org/10.1136/bmj.d4002.
StataCorp. Stata statistical software release 16. College Station, TX: StataCorp LLC.; 2019.
Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014.
Akbal A, Tutkun E, Yilmaz H. Lead exposure is a risk for worsening bone mineral density in middle-aged male workers. Aging Male. 2014;17(3):189–93. https://doi.org/10.3109/13685538.2013.836482.
Dursun N, Tutus A. Chronic occupational lead exposure and thyroid function. J Trace Elem Exp Med. 1999;12(1):45–9. https://doi.org/10.1002/(SICI)1520-670X(1999)12:1%3c45::AID-JTRA5%3e3.0.CO;2-D.
Ferri FF. Ferri’s clinical advisor 2022, E-Book. Elsevier Health Sciences; 2021.
Gennart JP, Bernard A, Lauwerys R. Assessment of thyroid, testes, kidney and autonomic nervous system function in lead-exposed workers. Int Arch Occup Environ Health. 1992;64(1):49–57. https://doi.org/10.1007/BF00625951.
Zaidi SSA, Kumar S, Gandhi SJ, Saiyed HN. Preliminary studies on thyroid function in welders. J Occup Health. 2001;43(2):90–1. https://doi.org/10.1539/joh.43.90.
Bledsoe ML, Pinkerton LE, Silver S, Deddens JA, Biagini RE. Thyroxine and free thyroxine levels in workers occupationally exposed to inorganic lead. Environ Health Insights. 2011;5:55–61. https://doi.org/10.4137/EHI.S7193.
Dundar B, Oktem F, Arslan MK, Delibas N, Baykal B, Arslan C, et al. The effect of long-term low-dose lead exposure on thyroid function in adolescents. Environ Res. 2006;101(1):140–5. https://doi.org/10.1016/j.envres.2005.10.002.
Erfurth EM, Gerhardsson L, Nilsson A, Rylander L, Schutz A, Skerfving S, et al. Effects of lead on the endocrine system in lead smelter workers. Arch Environ Health. 2001;56(5):449–55. https://doi.org/10.1080/00039890109604481.
Gravel S, Lavoue J, Bakhiyi B, Lavoie J, Roberge B, Patry L, et al. Multi-exposures to suspected endocrine disruptors in electronic waste recycling workers: associations with thyroid and reproductive hormones. Int J Hyg Environ Health. 2020;225:113445. https://doi.org/10.1016/j.ijheh.2019.113445.
Gustafson A, Hedner P, Schutz A, Skerfving S. Occupational lead exposure and pituitary function. Int Arch Occup Environ Health. 1989;61(4):277–81.
Lopez CM, Pineiro AE, Nunez N, Avagnina AM, Villaamil EC, Roses OE. Thyroid hormone changes in males exposed to lead in the Buenos Aires area (Argentina). Pharmacol Res. 2000;42(6):599–602. https://doi.org/10.1006/phrs.2000.0734.
Pekcici R, Kavlakoğlu B, Yilmaz S, Şahin M, Delibaşi T. Effects of lead on thyroid functions in lead-exposed workers. Cent Eur J Med. 2010;5(2):215–8. https://doi.org/10.2478/s11536-009-0092-8.
Singh B, Chandran V, Bandhu HK, Mittal BR, Bhattacharya A, Jindal SK, et al. Impact of lead exposure on pituitary-thyroid axis in humans. Biometals. 2000;13(2):187–92. https://doi.org/10.1023/a:1009201426184.
Definit C. Blood lead concentration reference blood lead levels (BLL) for adults in the US. CDC lead document, 2015, https://www.cdc.gov/niosh/topics/ables/pdfs/Reference%20Blood%20Levels%20for%20Adults-2015-12-18_508.pdf.
Kirschner K, et al. Very high blood lead levels among adults—United States, 2002–2011. MMWR Morb Mortal Wkly Rep. 2013;62(47):967–71.
Funding
No funding support for this work.
Author information
Authors and Affiliations
Contributions
UK: Conceptualization, Data curation, Investigation, Methodology and Review. VA: Conceptualization, Data curation, Investigation, Methodology and Review. BBS: Data curation, Formal analysis, Investigation, Methodology, Software and Review. BR: Conceptualization, Data curation, Investigation, Methodology, Original draft and Review.
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Balachandar, R., Viramgami, A., Bagepally, B.S. et al. Association Between Blood Lead Levels and Thyroid Function: An Updated Systematic Review and Meta-Analysis. Ind J Clin Biochem 38, 426–436 (2023). https://doi.org/10.1007/s12291-023-01113-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-023-01113-8