Abstract
Purpose
To investigate whether digital breast tomosynthesis (DBT) and subsequently generated synthesized mammography (SM) images show a better performance than full-field digital mammography (FFDM) images for diagnosing malignant breast lesions. In addition, the radiation doses for SM using different procedures were compared.
Materials and methods
This prospective study enrolled 212 women (age ≥ 25 years) with clinically suspicious breast lesions. All participants underwent FFDM and DBT with the same breast compression. Finally, 222 lesions were confirmed by pathological analysis. The mammogram results were evaluated according to the BI-RADS criteria and compared with the pathological results. The diagnostic performances, morphological features and average glandular doses (AGDs) were compared.
Results
In total, 141 malignant lesions and 81 benign lesions were confirmed by pathological analysis. The overall AGD showed no significant difference between FFDM and DBT. Compared with 2D imaging, the AUC values of FFDM plus DBT and SM plus DBT were both significantly different overall (P = 0.0002) and remained significantly different in dense breasts (P < 0.0001). In terms of morphologic characteristics, lesions showed similar morphology between FFDM and SM, while the lesion characteristics were discordant from 2D imaging to DBT in 33 lesions in dense breasts.
Conclusions
Compared to FFDM, 2D SM images generated from DBT had significantly improved diagnostic efficacy for detecting malignant breast lesions without increasing radiation doses. This new procedure is useful for characterizing breast lesions, particularly in dense breasts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Digital breast tomosynthesis (DBT) was approved by the US Food and Drug Administration (FDA) in 2011, and it has been widely used in combination with full-field digital mammography (FFDM); the efficiency of this new technology has also been evaluated in a number of studies [1,2,3]. By providing a three-dimensional (3D) view of the breast from a series of slice images, DBT is able to reduce the overlapping of normal tissues and breast lesions thus increasing cancer detection and improving diagnostic performance [4,5,6,7].
The primary limitations of DBT in combination with FFDM are increased radiation doses and time consumption for examination and interpretation [8, 9]. Adjustments have been suggested to overcome these drawbacks of this combined procedure, such as decreasing the projection angle of DBT or canceling the FFDM examination. However, the two-dimensional (2D) portion is still essential for evaluating some abnormalities, such as microcalcifications, and for making comparisons with prior 2D images [10]. Therefore, one adjustment is to generate 2D synthesized mammography (SM) images from the DBT dataset. With this adjustment, 2D images are maintained while radiation doses are not increased [11].
SM images created by adding and filtering the stack of reconstructed DBT sections are similar to generating a maximum intensity projection (MIP). Compared with the prior procedure of DBT plus FFDM, the radiation dose can be potentially reduced by approximately 40–50% when using DBT plus SM images generated from the tomosynthesis data [12, 13]. To date, there have been several studies on the performance of SM alone or in combination with DBT versus FFDM alone or in combination with DBT. The initial experimental results demonstrated that the radiologists’ performance when reading SM plus DBT images was worse than that when reading FFDM plus DBT images [14]. With rapid improvement in the quality of 2D SM, the US FDA approved the use of SM in conventional 2D digital mammography for both DBT screening and diagnosis in 2013. Recently, some studies have supported that DBT plus SM images created from tomosynthesis can reduce radiation exposure while maintaining improved diagnostic performance [15,16,17]. However, the application of SM for diagnosing or screening for breast cancer has just begun in China, and DBT plus SM, as a new combined procedure for breast cancer detection, may be even more appealing in Asian women, because it could substantially benefit females with dense breasts.
To promote the usage of SM in the Asian population, the purpose of this study was to assess the diagnostic performances and radiation doses of two different procedures—SM plus DBT and FFDM plus DBT. Furthermore, the morphological characteristics shown in the 2D images and tomosynthesis images were also compared.
Materials and methods
Patient enrolment
The prospective study was approved by the institutional review board. All participants signed written informed consent before the examinations. The study plan and data collection were developed before the test because of the prospective design. The inclusion criteria were as follows: patients who (a) were older than 25 years old, (b) had a clinically suspicious breast lesion, and (c) had the lesion confirmed by pathology after examination. The exclusion criteria were: patients who (a) were undergoing pregnancy or lactation when the study began, (b) had undergone prior excisional biopsy or surgery of the breast, (c) had breast implants, or (d) had been diagnosed with breast cancer. A total of 93 patients were enrolled from 2 clinical trials for tomosynthesis from June to August 2015, and 119 patients were enrolled from March to May 2016. Finally, 212 participants were included in this study. All of the participants’ diagnoses were confirmed by pathological analysis of biopsy or surgical specimens.
Image acquisition
Digital mammography and digital breast tomosynthesis
For 119 patients, DBT and 2D FFDM were acquired with a GE commercial system (SenoClaire, GE, Chalfont StGiles, USA), and 93 patients were imaged with a Hological system (Selenia Dimensions, Hologic, Bedford, USA). Since the FDA of China has not approved the use of 2D SM for clinical diagnosis before clinical trials, the SM images were only available for patients during that time. The X-ray tube moved over a 20° arc in the GE system and a 15° arc in the Hologic system while the breast was compressed. All participants underwent FFDM and DBT sequentially with the same breast compression. The imaging system automatically estimated the average glandular dose (AGD). The projections were combined to create a full three-dimensional image set of the breast with 1-mm slices throughout the breast. 2D SM images were generated from the DBT dataset for each case using V-preview processing software (GE) and C-View processing software (Hologic). Finally, three sets of mammograms (2D FFDM, 2D SM and DBT images) were acquired, including two-view images of both breasts (craniocaudal and mediolateral oblique views).
Image interpretation
All images were independently reviewed by two radiologists who specialized in breast imaging with 6–10 years of experience. When the assessment results differed between the two readers, another reader with 35 years of experience, having more experience with breast imaging, interpreted the images again. Thus, consensus was established as the final assessment. All of the radiologists had participated in prior studies involving DBT. Before this review, each reader also attended a 1-day DBT reading course and read a test set of 100 cases. Readers reviewed four groups of images: (a) 2D FFDM, (b) 2D SM, (c) 2D FFDM plus DBT, and (d) 2D SM plus DBT images for all cases. The reading sessions were performed at least 2 weeks apart to minimize any possible bias resulting from reader memory. Readers were blinded to the pathologic results of each case. Mammographic breast density and abnormalities were assessed according to the Breast Imaging-Reporting and Data System (BI-RADS) of the American College of Radiology (ACR) using eight-point forced BI-RADS scores (0, 1, 2, 3, 4a, 4b, 4c, or 5) [18]. Final assessments of SM and FFDM made by the observers were divided into two categories: negative (BI-RADS score of 4a and lower) and positive (BI-RADS score of 4b and higher) because all the patients enrolled in this study with a clinically suspicious lesion and BI-RADS 4a still had a less than 10% probability of malignancy. BI-RADS 0, which was an incomplete assessment that warranted further evaluation, was considered positive in this study. “Almost entirely fat” and “scattered fibroglandular densities” were classified as “fatty” breasts, and “heterogeneously dense” and “extremely dense” breast tissue were classified as “dense” breasts. If readers detected visible lesions, they recorded the size, anatomic location (left or right, clock position, and distance from nipple) and morphological type (mass, focal asymmetry/asymmetry, architectural distortion, and calcification). If the detected lesion had multiple morphological findings, the most dominant finding was recorded. When readers detected multiple lesions in the same patient, they documented further descriptions of each lesion.
All pathologic specimens were reviewed by one breast pathologist with 15 years of experience. Pathological data included histological tumor type and the longest diameter of the lesion.
Statistical analysis
The independent t test was used to compare the difference in the AGD of DBT and FFDM images in two breast density groups and two compression thickness groups. Receiver operating characteristic (ROC) curve analysis was used to evaluate the diagnostic efficacy. The strength of the kappa agreement was defined as follows: < 0.00 = poor; 0.00–0.20 = slight; 0.21–0.40 = fair; 0.41–0.60 = moderate; 0.61–0.81 = substantial; and 0.81–1.00 = almost perfect. P < 0.05 was considered to indicate a significant difference for all comparisons. All statistical analyses were performed using SPSS ver. 19.0 (SPSS Inc., Chicago, IL, USA) and MedCalc 12.7 (MedCalc, Mariakerke, Belgium) software.
Results
Breast lesion pathology
A total of 222 lesions were confirmed by biopsy and/or surgery in 212 patients. Ten patients had two lesions, and the others all had solitary lesions. Malignant lesions (n = 141) included invasive ductal carcinoma (n = 117), ductal carcinoma in situ (DCIS) (n = 13), invasive lobular carcinoma (n = 3), invasive papillary carcinoma (n = 1), and malignant fibrous histiocytoma (n = 1). Additionally, six lesions were confirmed to be invasive carcinoma with unclear classification, and the affected patients underwent further neoadjuvant chemotherapy. Benign lesions (n = 81) included fibroadenoma (n = 33), benign phyllodes (n = 3), adenosis (n = 24), mastitis (n = 5), breast intraductal papilloma (n = 13), and sclerosing adenosis (n = 3).
Average glandular dose
The AGD of FFDM was 1.79 ± 0.79 mGy (ranged from 0.63 to 3.49 mGy), and the AGD of DBT was 1.81 ± 0.54 mGy (ranged from 0.81 to 3.52 mGy). There was no significant difference between the two groups (t = 0.321, P = 0.602). The breast density distribution of all the cases was as follows: 19 of 212 (9%) were almost entirely fatty, 43 of 212 (20%) were scattered fibroglandular dense tissue, 88 of 212 (42%) were heterogeneously dense, and 62 of 212 (29%) were extremely dense. In this study, 60 patients had “fatty” including “almost entirely fat” and “scattered fibroglandular dense” breast tissue, and 150 patients had “dense” including “heterogeneously dense” and “extremely dense” breast tissue. The compression thickness was 49.82 ± 12.00 mm (ranged from 17 to 84 mm). Because a “standard breast” according to the ACR means approximating a 45-mm compressed breast, 45 mm was defined as the boundary to assess the AGD [19]. The AGDs of FFDM and DBT images were also compared according to breast density and compression thickness. In “fatty” breasts, the AGD was higher in DBT images than in FFDM images (1.49 ± 0.60 mGy in FFDM and 1.74 ± 0.52 mGy in DBT, t = 0.432, P < 0.001), while in the “dense” breasts, there was no significant difference between FFDM and DBT images (1.88 ± 0.82 mGy in FFDM and 1.84 ± 0.55 mGy in DBT, t = 0.33, P = 0.975). There was no significance regardless of the compression thickness of the breast (P > 0.05).
Clinical performance
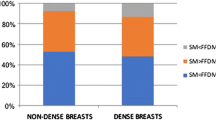
Table 1 shows the diagnostic performances of 2D images alone and 2D plus DBT images for breast lesions. The diagnostic performance was the same between 2D FFDM and 2D SM. The AUC values of reader 1, reader 2 and overall assessment were 0.724, 0.782, 0.792 for the 2D images, 0.817, 0.864, 0.885 for FFDM plus DBT images, and 0.820, 0.858, 0.882 for DBT plus SM images. Compared with 2D images, both FFDM plus DBT and SM plus DBT were significantly different (z = 3.707, P = 0.0002 and z = 3.699, P = 0.0002, respectively). There was no significant difference between FFDM plus DBT and SM plus DBT (z = 0.232, P = 0.816). According to the breast density, the AUC value in “fatty” breasts was higher than that in “dense” breasts. Compared with 2D imaging, the AUC values of FFDM plus DBT and SM plus DBT were also significantly different in “dense” breasts (z = 4.311, P < 0.0001 and z = 4.351, P < 0.0001, respectively), while the difference became nonsignificant in “fatty” breasts (z = 1.428, P = 0.1533 and z = 1.428, P = 0.1533).
Other indexes of diagnostic performance, such as sensitivity and specificity, are also listed in Table 1. Compared with 2D mammography, the sensitivity was significantly different in DBT plus SM overall and for lesions in “dense” breasts (P < 0.0001). The difference in sensitivity was nonsignificant in “fatty” breasts. Regarding the specificity, there was no significant difference between 2D mammography and DBT plus SM for all types of breast densities.
Morphological characteristics of 2D mammography and DBT
The morphological types of lesions in 2D mammography and DBT are summarized in Table 2. The lesions showed a similar morphology in the FFDM and SM images (Fig. 1). In contrast, the lesion characteristics were discordant between the 2D mammography and DBT images in 33 lesions, which all occurred in “dense” breasts (Table 3). Of 19 malignant lesions, 8 were considered asymmetric, and 6 were considered to have architectural distortion on 2D mammography and were categorized as microlobulated or spiculated masses on DBT (Figs. 2, 3). Eight benign lesions described as asymmetric on 2D mammography were categorized as obscured masses on DBT (Fig. 4). There were 19 asymmetric lesions on 2D mammography that had visible mass margins on DBT. For calcified lesions, there was no difference between 2D mammography and DBT. However, six lesions were still visible on DBT. Among them, two lesions were confirmed to be DCIS, three lesions were intraductal papilloma, and one was mastitis.
Interobserver agreement
The interobserver agreement between the two readers in terms of the BI-RADS diagnosis can be considered substantial with ϰ = 0.763 for FFDM and 0.755 for SM and almost perfect with ϰ = 0.831 for FFDM plus DBT and 0.828 for SM plus DBT. The interobserver agreement was substantial to almost perfect for the SM/FFDM findings (0.848) and for the DBT findings (0.873).
Discussion
This study found that 2D SM images created from DBT had a similar clinical performance to conventional FFDM. When the diagnostic performance of DBT plus SM was evaluated compared to 2D mammography according to breast density, the benefit was mainly attributable to sensitivity in dense breasts. In addition, the lesion characteristics showed discordance between 2D and DBT images in dense breasts, especially for lesions showing asymmetry on 2D mammography.
To our knowledge, this is the first study to investigate morphological changes in the main radiologic features from 2D images to DBT images. In line with other reports, the characteristics of spiculated masses and margin visualization were improved on DBT. Rose et al. reported that DBT could provide a clear definition of lesion margins, especially for spiculated masses, but not of microcalcifications [20]. In our study, the lesion characteristics on 2D mammography to DBT were discordant, and all these differences occurred in dense breasts, because the overlap between the lesion and normal tissue was eliminated on DBT. There were 19 asymmetric lesions on 2D mammography that showed had visible mass margins on DBT including 8 malignant lesions with spiculated masses and 6 benign lesions with obscured masses on DBT. Concerning asymmetry on 2D images, it is useful on DBT to describe this feature with the term “mass”, because adjacent dense fibroglandular tissue may impair the visibility of the margins of the mass. Of note, six lesions (including 2 cases of DCIS, 3 cases of intraductal papilloma and 1 case of mastitis) did not show any abnormalities even on DBT, which indicated that the detection and assessment of lesion characteristics in situ on DBT still need further study.
The significant improvement in the AUC for 2D mammography plus DBT compared with that of 2D mammography alone was in line with the results of published studies. The results of the study by Chae et al. indicated that the AUC value was 0.93 for FFDM and 0.95 for DBT. When diagnostic performance was evaluated by breast density, the improvement in the reader’s performance was mainly attributable to dense breasts [5]. The AUC value in our study was lower than that reported previously for an experimental version of DBT images, but the results were still consistent with a relative improvement in diagnostic performance, especially in dense breasts. The diagnostic performance was almost the same between 2D FFDM and 2D SM in our study, which was also similar to the results of a recent study. In the results of the study by Zuley et al., the reader-averaged AUC values for FFDM and SM were 0.889 and 0.894, while for FFDM plus DBT and SM plus DBT, the AUC values were 0.939 and 0.916 [21]. However, initial relevant studies on SM demonstrated that 2D SM mammography may be inferior to FFDM, because this modality did not show any positive changes that affected clinical performance [13, 22]. Because of the improvement in the quality of synthetic images, SM images created from DBT could serve in the place of FFDM for diagnosis.
Furthermore, we also compared the diagnostic performance of 2D SM plus DBT with that of 2D mammography alone. This analysis was partially consistent with earlier findings, showing that the significant improvement in the sensitivity of 2D SM plus DBT benefited all the patients and females with dense breast tissue. Gilbert et al. also found that SM plus DBT had better sensitivity for invasive cancers with a 20 mm tumor size [4]. However, regarding the effects on specificity, the results were discordant with those of recent studies. The results of the study by Gur et al. suggested that SM plus DBT had comparable specificity to that of FFDM plus DBT, and Gilbert et al. demonstrated that the specificity of SM plus DBT was better than that of FFDM [4, 14]. The results for specificity did not show any superiority in our study or the study by Chae et al. [5].
SM in the place of FFDM can also yield a significant reduction in radiation dose for patients who undergo DBT alone. Considering the similar radiation dose proposed by Paulis et al. and Choi et al., the overall AGD between DBT and DBT in our study also showed relatively little difference (mean AGD 1.79 mGy for FFDM, 1.81 mGy for DBT) [23, 24]. Further subgroup analyses according to breast density indicated that the radiation dose for DBT, which was still higher than that for FFDM in fatty breasts, was similar to that for FFDM in dense breasts, or even slightly lower (mean AGD 1.88 mGy for FFDM, 1.84 mGy for DBT). Regarding the exposure radiation to the breast, DBT alone is available and adequate for routine clinical practice, especially in patients with dense breasts.
Our study has some limitations. First, we enrolled all participants with clinical suspicion in this study. Both FFDM and DBT examinations were used in a diagnostic setting, which may have led to a selection bias. There were relatively more malignant lesions than benign lesions included. Second, in this diagnostic setting of cancer detection, final assessments were divided into two categories: positive (BI-RADS score of 4b–5) and negative (BI-RADS score of 1–4a). Because some benign lesions, such as large fibroadenomas, phyllodes and intraductal papillomas, were considered, we still preferred to assess BI-RADS 3 or even 4a, recommending further biopsy for clinical diagnosis. Additionally, BI-RADS 0 was considered positive in this study. This grouping was slightly different from that in a previously published paper and may have affected the diagnostic performance [25]. Third, breast tissue was classified for analyses in our study, and heterogeneously dense and extremely dense breasts accounted for the majority of breast densities (150/212, 70.75%). To further evaluate the value of DBT in dense breasts, patients with almost entirely fat and scattered fibroglandular densities need to be enrolled to reduce bias. Finally, the results of this study were generalized in a diagnostic setting. Further study in a larger screening population of Asian patients is warranted to determine a strategic approach for patients with dense breasts [26, 27].
In conclusion, 2D SM images generated from DBT replaced the need for FFDM and could improve the diagnostic efficacy without increasing the radiation dose compared with FFDM. This new procedure could be useful in better characterizing lesions, especially in dense breasts. Further studies are needed to validate and generalize the findings of SM in combination with DBT for both diagnostic and screening populations.
References
Martinez MP, Etxano J. Breast tomosynthesis: a new tool for diagnosing breast cancer. Radiologia. 2015;57(1):3–8.
Peppard HR, et al. Digital breast tomosynthesis in the diagnostic setting: indications and clinical applications. Radiographics. 2015;35(4):975–90.
Hodgson R, et al. Systematic review of 3D mammography for breast cancer screening. Breast. 2016;27:52–61.
Gilbert FJ, et al. Accuracy of digital breast tomosynthesis for depicting breast cancer subgroups in a UK retrospective reading study (TOMMY trial). Radiology. 2015;277(3):697–706.
Chae EY, et al. Detection and characterization of breast lesions in a selective diagnostic population: diagnostic accuracy study for comparison between one-view digital breast tomosynthesis and two-view full-field digital mammography. Br J Radiol. 2016;89(1062):20150743.
Dang PA, et al. Addition of tomosynthesis to conventional digital mammography: effect on image interpretation time of screening examinations. Radiology. 2014;270(1):49–56.
Seo M, et al. Addition of digital breast tomosynthesis to full-field digital mammography in the diagnostic setting: additional value and cancer detectability. J Breast Cancer. 2016;19(4):438–46.
Bernardi D, et al. Application of breast tomosynthesis in screening: incremental effect on mammography acquisition and reading time. Br J Radiol. 2012;85(1020):e1174–8.
Bouwman RW, et al. Average glandular dose in digital mammography and digital breast tomosynthesis: comparison of phantom and patient data. Phys Med Biol. 2015;60(20):7893–907.
Spangler ML, et al. Detection and classification of calcifications on digital breast tomosynthesis and 2D digital mammography: a comparison. Am J Roentgenol. 2011;196(2):320–4.
Skaane P, et al. Two-view digital breast tomosynthesis screening with synthetically reconstructed projection images: comparison with digital breast tomosynthesis with full-field digital mammographic images. Radiology. 2014;271(3):655–63.
Vecchio S, et al. A novel approach to digital breast tomosynthesis for simultaneous acquisition of 2D and 3D images. Eur Radiol. 2011;21(6):1207–13.
Nelson JS, et al. How does c-view image quality compare with conventional 2D FFDM? Med Phys. 2016;43(5):2538.
Gur D, et al. Dose reduction in digital breast tomosynthesis (DBT) screening using synthetically reconstructed projection images: an observer performance study. Acad Radiol. 2012;19(2):166–71.
Zuckerman SP, et al. Implementation of synthesized two-dimensional mammography in a population-based digital breast tomosynthesis screening program. Radiology. 2016;281(3):730–6.
Freer PE, et al. Clinical implementation of synthesized mammography with digital breast tomosynthesis in a routine clinical practice. Breast Cancer Res Treat. 2017;166(2):501–9.
Caumo F, et al. Digital breast tomosynthesis with synthesized two-dimensional images versus full-field digital mammography for population screening: outcomes from the Verona screening program. Radiology. 2018;287(1):37–46.
Mercado CL. BI-RADS update. Radiol Clin North Am. 2014;52:481–7.
Saunders RJ, et al. Does image quality matter? Impact of resolution and noise on mammographic task performance. Med Phys. 2007;34(10):3971–81.
Rose SL, et al. Implementation of breast tomosynthesis in a routine screening practice: an observational study. Am J Roentgenol. 2013;200(6):1401–8.
Zuley ML, et al. Comparison of two-dimensional synthesized mammograms versus original digital mammograms alone and in combination with tomosynthesis images. Radiology. 2014;271(3):664–71.
Hofvind S, et al. Digital breast tomosynthesis and synthetic 2D mammography versus digital mammography: evaluation in a population-based screening program. Radiology. 2018;287(3):787–94.
Paulis LE, et al. Radiation exposure of digital breast tomosynthesis using an antiscatter grid compared with full-field digital mammography. Investig Radiol. 2015;50(10):679–85.
Choi JS, et al. Comparison between two-dimensional synthetic mammography reconstructed from digital breast tomosynthesis and full-field digital mammography for the detection of T1 breast cancer. Eur Radiol. 2016;26(8):2538–46.
Kim SA, et al. Characterization of breast lesions: comparison of digital breast tomosynthesis and ultrasonography. Korean J Radiol. 2015;16(2):229–38.
Aujero MP, et al. Clinical performance of synthesized two-dimensional mammography combined with tomosynthesis in a large screening population. Radiology. 2017;283(1):70–6.
Pattacini P, et al. Digital mammography versus digital mammography plus tomosynthesis for breast cancer screening: the Reggio Emilia Tomosynthesis randomized trial. Radiology. 2018;288(2):375–85.
Acknowledgements
We thank all the patients of this study for their participation. We greatly appreciate Li Liu, Xiaojing Zheng, Jian Wu, Danting Hu and Yujiao Jin at Department of Radiology for their excellent assistance.
Funding
Weijun Peng received funding from the National Natural Science Foundation of China (Grant number: 61731008). Yajia Gu received funding from National Key Research and Development Program of China (Grant number: 2016YFC1303003) and Cancer Research Program of National Cancer Center (Grant number: NCC2017A03). Chao You received funding from Shanghai Municipal Health Planning Commission Youth Project (Grant number: 20184Y0010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
You, C., Zhang, Y., Gu, Y. et al. Comparison of the diagnostic performance of synthesized two-dimensional mammography and full-field digital mammography alone or in combination with digital breast tomosynthesis. Breast Cancer 27, 47–53 (2020). https://doi.org/10.1007/s12282-019-00992-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-019-00992-1