Abstract
Background
Inability to visualize indocyanine green fluorescence images in the surgical field limits the application of current near-infrared fluorescence imaging (NIR) systems for real-time navigation during sentinel lymph node (SLN) biopsy in breast cancer patients. The aim of this study was to evaluate the usefulness of the Medical Imaging Projection System (MIPS), which uses active projection mapping, for SLN biopsy.
Methods
A total of 56 patients (59 procedures) underwent SLN biopsy using the MIPS between March 2016 and November 2017. After SLN biopsy using the MIPS, residual SLNs were removed using a conventional NIR camera and/or radioisotope method. The primary endpoint of this study was identification rate of SLNs using the MIPS.
Results
In all procedures, at least one SLN was detected by the MIPS, giving an SLN identification rate of 100% [95% confidence interval (CI) 94–100%]. SLN biopsy was successfully performed without operating lights in all procedures. In total, 3 positive SLNs were excised using MIPS, but were not included in the additional SLNs excised by other methods. The median number of SLNs excised using the MIPS was 3 (range 1–7). Of procedures performed after preoperative systemic therapy, the median number of SLNs excised using the MIPS was 3 (range 2–6).
Conclusions
The MIPS is effective in detecting SLNs in patients with breast cancer, providing continuous and accurate projection of fluorescence signals in the surgical field, without need for operating lights, and could be useful in real-time navigation surgery for SLN biopsy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sentinel lymph node (SLN) biopsy is part of the standard of care for patients with primary clinically node-negative breast cancer [1]. Clinical trials and meta-analyses have shown that axillary node dissection for SLN-negative patients has no survival impact [2,3,4]. Recent studies have shown that omission of axillary node dissection for patients with limited positive SLNs has no adverse impact on survival and decreases the incidence of lymphedema [5]. Both the radioisotope (RI) and blue dye methods are well-established and used worldwide. However, the RI method requires involvement of nuclear medicine, which limits its use to relatively high-volume centers. The blue dye method requires special surgical skill to obtain sufficient accuracy and has a risk of anaphylactic reactions.
An indocyanine green (ICG) fluorescence method was developed in 2005 to overcome these problems [6]. A near-infrared fluorescence imaging system (NIR system) visualizes subcutaneous lymphatic flow and enables the surgeon to navigate and perform sequential dissection of SLNs. Several clinical trials have shown that the ICG fluorescence method has an equal or higher SLN identification rate compared with that of conventional methods [7,8,9]. Meta-analyses showed that there was no significant difference between ICG fluorescence and RI for SLN detection [10, 11]. Although the ICG fluorescence method is highly sensitive and easy to perform, current NIR systems have several technical issues that need to be improved. The current NIR systems display the fluorescence image on remote monitors, because the fluorescence signals are invisible under direct observation of the surgical field. Therefore, surgeons must look away from the surgical field to confirm the location of the fluorescence signals. These systems also require dimming of lights within the operative field to prevent white light contamination of images. These factors can disrupt surgical workflow and may increase the duration of surgery.
The Medical Imaging Projection System (MIPS) is a novel NIR system that projects the ICG images directly on the surgical field using a projection mapping technique [12]. The MIPS has the potential to provide real-time navigation for SLN biopsy. The aim of this study was to explore the clinical utility of the MIPS with ICG fluorescence for SLN biopsy.
Patients and methods
Patients
Eligibility criteria were age 20–75 years and histologically confirmed but clinically node-negative breast cancer. Patients who underwent previous axillary surgery or who had a history of allergy to ICG or iodine were excluded from the study.
Study design
At first, the study was conducted as an interventional study because the MIPS was an unapproved medical device (UMIN000020768) (N = 8). After approval of the MIPS, this study was conducted as an observational study (N = 48). We reported the results of the combined analysis of the two studies, as the eligibility criteria and primary endpoint were identical between the two studies. The primary endpoint was SLN identification rate, defined as the percentage of all patients in whom at least one SLN was detected by the MIPS. Secondary endpoints included sensitivity of the MIPS compared with the conventional NIR camera Photodynamic Eye Camera (PDE; pde-neo, Hamamatsu Photonics K.K., Hamamatsu, Japan) or RI methods. This sensitivity was calculated as the percentage of patients with tumor-positive SLNs detected using the MIPS in all patients with axillary metastases as determined by the PDE or RI. The number of SLNs detected by the MIPS was also noted. The expected identification rate was estimated to be 98%, and its threshold was estimated to be 90%. With a statistical power of 80% and a one-sided type 1 error of 5%, the number of eligible patients required for the study was calculated to be 48 using a binominal analysis method.
The study protocol was approved by the institutional review board at Kyoto University Hospital. All patients provided informed consent to participate in this study.
MIPS
A detailed description of the MIPS has been reported previously [12]. Briefly, the MIPS has a projection head that uses a half mirror to match the optical axis of the NIR camera and the projector (Fig. 1a). The MIPS obtains the location of the fluorescence ICG emission and projects its image onto the location of the fluorescence emission in real-time, regardless of shifting and deformation of the organ. The difference between the location on the real fluorescence ICG emission and the projected image is within 1 mm, with a time lag within 100 ms. The projection head is designed to be located approximately 100 cm above the operative field and is not held by the surgeon. The projector of the MIPS can also illuminate the surgical field, allowing surgeons to perform the procedure without the need for operating lights (Fig. 1b, c).
The Medical Imaging Projection System (MIPS). a Photograph of the MIPS showing the projection head and pole components. b Intraoperative view using the MIPS. The projection head (yellow bold arrow) is located approximately 100 cm above the operative field. c Operative field is well-lit without use of operating lights
Surgical procedures
ICG (5 mg in 1 mL; Diagnogreen®; Daiichi Sankyo Co., Tokyo, Japan) was injected intradermally at the edge of the areola. Fluorescent subcutaneous lymphatics were visualized using the MIPS and traced to the axilla where occasionally nodes could be seen percutaneously. We also used a plastic capsule to push and thinner the subcutaneous tissue to help the recognition of the fluorescence signals from SLNs percutaneously. SLNs detected by the MIPS were then excised. All these procedures were performed with the operating lights turned off, as per the manufacturer’s recommendations. After the SLN biopsy using the MIPS, residual SLNs were removed using a conventional NIR camera PDE camera (Hamamatsu Photonics) and/or RI. In the first interventional study, combined use of RI or PDE was mandate. In the second cohort study, combined use of RI or PDE was recommended. All the excised SLNs were also examined using the MIPS, PDE, and a hand-held gamma probe, and the detectability of each signal was recorded. All SLNs underwent pathological evaluation according to the local protocol, which includes serial sectioning at 2–3 mm followed by routine staining with hematoxylin and eosin (H&E).
Results
A total of 56 patients (53 unilateral, 3 bilateral) underwent SLN biopsy using the MIPS from March 2016 to November 2017. This analysis was based on a total of 59 procedures. Median age and Body Mass Index (BMI) were 54 years (range 28–75 years) and 20.4 kg/m2 (range 15.4–31.3 kg/m2), respectively (Table 1). More than half were T1 stage (57%), and 10 procedures (17%) were performed on patients with ductal carcinoma in situ. Of the 59 procedures, 12 (20%) were performed after preoperative systemic therapy (PST). In 38 procedures (64%), both the RI and ICG methods were used.
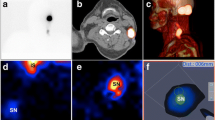
Figure 2 shows the direct-view pictures of SLN biopsy using the MIPS. In all procedures, at least one SLN was detected by the MIPS, giving an SLN detection rate of 100% [95% confidence interval (CI) 94–100%]. SLN biopsy was successfully performed without operating lights in all procedures. If we excluded 12 patients with PST, identification rate by MIPS was 100% (95% CI 92–100%). Of the 201 SLNs excised, 174 (87%) were detected by only the MIPS, and 27 (13%) were excised additionally by PDE, RI, or palpation (Table 2). In most of the additionally excised SLNs, the MIPS could retrospectively detect ICG fluorescent signals in the excised tissue.
Photographs of sentinel lymph node (SLN) biopsy using the MIPS. a Subcutaneous lymph channels (blue) visualized using the MIPS. b Real-time fluorescence imaging helps to identify the fluorescent SLN after the skin incision is made. The ICG fluorescence signal visualized using a color scale indicating the strength of the signal (red = strong, yellow = medium; blue = weak). c The projected fluorescence image is automatically adjusted upon deformation of the organ
Among the 201 SLNs dissected, only 3 contained macrometastasis; 1 SLN had isolated tumor cells only. In the procedures involving these 3 SLNs with macrometastases, the RI method was not combined with ICG fluorescence. All 3 positive SLNs were excised using the MIPS and were not included in the additional SLNs excised using the PDE. The low percentage of the positive SLNs made it difficult to evaluate sensitivity of the MIPS.
The median number of SLNs per patient excised by the MIPS was 3 (range 1–7) (Table 3). Although patients with a high BMI (≥ 22 kg/m2) compared to those with a low BMI (< 22 kg/m2) tended to have fewer SLNs excised, this difference was not statistically significant (P = 0.07). Of procedures performed after PST, the median number of SLNs excised using the MIPS was 3 (range 2–6).
Discussion
This study demonstrates that the MIPS has a high SLN identification rate. The MIPS provides direct visualization of ICG fluorescence projected onto the surgical field and enables SLN biopsy without disrupting surgical workflow.
The MIPS SLN identification rate was comparable to that of the conventional NIR system. A previous meta-analysis showed that the identification rate using the ICG fluorescence method ranges from 89 to 100%; and the ICG fluorescence and RI methods do not differ significantly in SLN detection [11]. Since the basic NIR system is a common feature of conventional NIR systems and the MIPS, it is reasonable that the MIPS had a high SLN identification rate. The mean number of SLNs removed using the ICG fluorescence method has been reported as 1.5–3.4 [11]. The median number of SLNs excised by the MIPS was 3, which is also comparable with reported results using the conventional ICG fluorescence method.
Several new NIR systems have been developed. The HyperEye Medical System (HEMS) (Mizuho Corp., Tokyo, Japan) can display superimposed color images and ICG fluorescence images on a remote monitor [13]. Although the HEMS facilitates the localization of ICG signals because of the color background image, it still requires surgeons to look away from the surgical field at a monitor screen. Mondal et al. developed another NIR system, named the optical see-through goggle-augmented imaging and navigation system [14]. In this goggle system, an ICG fluorescence image is projected onto a see-through display on the goggles. Although this system has the potential to facilitate real-time navigation, it has not been systematically evaluated in patients as yet.
Detection of SLNs decreases with increasing BMI [15]. In our study, fewer SLNs were excised from patients with high BMI than those with low BMI, but this difference was not statistically significant. SLN biopsy after PST was considered feasible, especially for patients with clinically node-negative cancer at baseline [1, 16,17,18]. However, several clinical trials have shown that among patients with clinically node-positive, SLN biopsy after PST has a lower identification rate and a higher false-negative rate than does SLN biopsy before PST [19,20,21]. Further analysis showed that the false-negative rate is estimated to be below 10% if at least 3 or more SLNs were excised. In the present study, SLN biopsies were performed after PST in 12 procedures. Although this is a small number of cases, the identification rate among them was 100% (95% CI 76–100%) and the median number of SLNs excised was 3 (range 2–6).
The principal clinical benefit of the MIPS is continuous and accurate projection of the ICG fluorescence image onto the surgical field. One of the advantages of the ICG fluorescence method is real-time monitoring of the lymphatic channels. However, conventional NIR systems could not take full advantage of ICG fluorescence in terms of real-time navigation, because surgeons had to disrupt the surgical workflow to confirm the location of the fluorescence signals. The MIPS enables SLN biopsy to be performed without shifting the visual focus and handling of operating light. Although quantitative comparison of these advantages is difficult in this single arm design study, these advantages will likely lead to shorter duration of surgery and lower surgical stress.
Our determination of a high SLN identification rate using the MIPS was based on relatively few procedures; however, this sample size does not hinder the demonstration of clinical utility of the MIPS, because the lower limit of 95% CIs was over 90%. Of the 201 SLNs excised, 27 (13%) were excised by PDE, RI, or palpation. However, MIPS could detect ICG fluorescence signals retrospectively in 23 of these 27 additional SLNs after excision. A person outside of the surgery adjusted the angle of the projection head of the MIPS, which may influence the detectability of SLNs. Improved flexibility of the projection head should solve this problem. In our study, the percentage of positive SLNs (1.5%) was very low compared with that in previous reports [22]. Preoperative examination of axillary lymph nodes in our institution includes palpation, ultrasonography, and contrast-enhanced magnetic resonance imaging (CE-MRI). If nodal involvement is suspected in these examinations, ultrasound-guided fine-needle aspiration biopsy (US-FNA) is also performed. Several studies showed that both US-FNA and CE-MRI increase the accuracy of preoperative axillary staging [23, 24], and involvement of these examinations may contribute to the low percentage of positive SLNs in our study.
In conclusion, this study demonstrates that the MIPS has a high SLN identification rate in patients with breast cancer. The MIPS provides continuous and accurate projection of ICG fluorescence images onto the surgical field and enables real-time navigation during surgery for SLN biopsy.
Abbreviations
- SLN:
-
Sentinel lymph node
- RI:
-
Radioisotope
- ICG:
-
Indocyanine green
- NIR:
-
Near-infrared fluorescence imaging system
- MIPS:
-
Medical Imaging Projection System
- PDE:
-
Photodynamic Eye Camera
- BMI:
-
Body Mass Index
References
Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35:561–4.
Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer. 2006;106:4–16.
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33.
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349:546–53.
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Kitai T, Inomoto T, Miwa M, Shikayama T. Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer. 2005;12:211–5.
Sugie T, Kinoshita T, Masuda N, Sawada T, Yamauchi A, Kuroi K, et al. Evaluation of the clinical utility of the ICG fluorescence method compared with the radioisotope method for sentinel lymph node biopsy in breast cancer. Ann Surg Oncol. 2016;23:44–50.
Sugie T, Sawada T, Tagaya N, Kinoshita T, Yamagami K, Suwa H, et al. Comparison of the indocyanine green fluorescence and blue dye methods in detection of sentinel lymph nodes in early-stage breast cancer. Ann Surg Oncol. 2013;20:2213–8.
Wishart GC, Loh SW, Jones L, Benson JR. A feasibility study (ICG-10) of indocyanine green (ICG) fluorescence mapping for sentinel lymph node detection in early breast cancer. Eur J Surg Oncol. 2012;38:651–6.
Ahmed M, Purushotham AD, Douek M. Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol. 2014;15:e351–62.
Sugie T, Ikeda T, Kawaguchi A, Shimizu A, Toi M. Sentinel lymph node biopsy using indocyanine green fluorescence in early-stage breast cancer: a meta-analysis. Int J Clin Oncol. 2017;22:11–7.
Nishino H, Hatano E, Seo S, Nitta T, Saito T, Nakamura M, et al. Real-time navigation for liver surgery using projection mapping with indocyanine green fluorescence: development of the novel medical imaging projection system. Ann Surg. 2018;267(6):1134–40.
Hokimoto N, Sugimoto T, Namikawa T, Funakoshi T, Oki T, Ogawa M, et al. A novel color fluorescence navigation system for intraoperative transcutaneous lymphatic mapping and resection of sentinel lymph nodes in breast cancer: comparison with the combination of gamma probe scanning and visible dye methods. Oncology. 2018;94:99–106.
Mondal SB, Gao S, Zhu N, Habimana-Griffin L, Akers WJ, Liang R, et al. Optical see-through cancer vision goggles enable direct patient visualization and real-time fluorescence-guided oncologic surgery. Ann Surg Oncol. 2017;24:1897–903.
Goyal A, Newcombe RG, Chhabra A, Mansel RE, Group AT. Factors affecting failed localisation and false-negative rates of sentinel node biopsy in breast cancer—results of the ALMANAC validation phase. Breast Cancer Res Treat. 2006;99:203–8.
Classe JM, Bordes V, Campion L, Mignotte H, Dravet F, Leveque J, et al. Sentinel lymph node biopsy after neoadjuvant chemotherapy for advanced breast cancer: results of Ganglion Sentinelle et Chimiotherapie Neoadjuvante, a French prospective multicentric study. J Clin Oncol. 2009;27:726–32.
van Deurzen CH, Vriens BE, Tjan-Heijnen VC, van der Wall E, Albregts M, van Hilligersberg R, et al. Accuracy of sentinel node biopsy after neoadjuvant chemotherapy in breast cancer patients: a systematic review. Eur J Cancer. 2009;45:3124–30.
Curigliano G, Burstein HJ, E PW, Gnant M, Dubsky P, Loibl S, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen international expert consensus conference on the primary therapy of early breast cancer 2017. Ann Oncol. 2017;28:1700–12.
Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455–61.
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14:609–18.
Boileau JF, Poirier B, Basik M, Holloway CM, Gaboury L, Sideris L, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol. 2015;33:258–64.
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Ashikaga T, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol. 2007;8:881–8.
Houssami N, Ciatto S, Turner RM, Cody HS III, Macaskill P. Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: meta-analysis of its accuracy and utility in staging the axilla. Ann Surg. 2011;254:243–51.
Liang X, Yu J, Wen B, Xie J, Cai Q, Yang Q. MRI and FDG-PET/CT based assessment of axillary lymph node metastasis in early breast cancer: a meta-analysis. Clin Radiol. 2017;72:295–301.
Acknowledgements
This study was supported by Acceleration Transformative research for Medical innovation, Japan Agency for Medical Research and Development (AMED, Grant number 17im0210201h0203). The authors thank Tomoko Okuda for her valuable help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
About this article
Cite this article
Takada, M., Takeuchi, M., Suzuki, E. et al. Real-time navigation system for sentinel lymph node biopsy in breast cancer patients using projection mapping with indocyanine green fluorescence. Breast Cancer 25, 650–655 (2018). https://doi.org/10.1007/s12282-018-0868-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-018-0868-2