Abstract
Objective
To examine breast cancer burden in females using incidence, mortality and mortality-to-incidence ratio (MIR) and its association with human development.
Methods
We employ the data of breast cancer in females from the Global Burden of Disease 2016 study for the period 1990 to 2016 for 102 countries. Human development is measured using the human development index (HDI). 5-year survival rate of breast cancer is proxied using the mortality-to-incidence ratio (MIR).
Findings
Globally, breast cancer has claimed 535341 female lives and 1.7 million incident cases had surfaced in 2016. High incidence rates were observed in very high HDI countries led by the Netherlands (117.2/100,000), whereas the mortality rate was high in low/medium HDI countries led by Afghanistan (35.4/100,000). Breast cancer incidence has more than doubled in 60/102 countries, whereas deaths have doubled in 43/102 countries. Globally, breast cancer MIR decreased from 0.41 to 0.32 over 1990–2016 and displayed negative gradient with HDI (r = − 0.87), indicating a low 5-year survival in less developed countries.
Conclusion
Heterogeneity in breast cancer burden, as per human development, and increasing breast cancer incidence and low survival rates, indicated by MIR, call for broader human development, improving breast cancer awareness, and cost-effective screening and treatment in less developed countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a leading cancer burden in females, claiming 535341 lives and resulting in 14.8 million disability-adjusted life years (DALYs), and 1.7 million new cases of breast cancer arose in 2016 making it one of the biggest causes of mortality and morbidity in females, worldwide [1, 2]. The incidence of breast cancer is increasing not only in developed countries, but also in developing countries [2]. The survival rate of breast cancer, although improved, showed distinct and heterogenous patterns in different countries due to factors such as lack of screening, early-stage detection and cost-effectiveness of treatment [3].
Measuring and tracking survival rate of different cancers (including breast cancer) is costly and mortality-to-incidence ratio (MIR) is demonstrated to be quite a useful indicator of 5-year survival [4]. 5-year survival proxied by MIR has been examined for different neoplasia: prostate cancer [5], bladder cancer [6], gastric cancer [7], liver cancer [8] and colorectal cancer [9]. Previous studies examining 5-year survival rates using mortality-to-incidence ratio (MIR) examined the association between MIR and human development index or other development indicators using data of select geographical locations (mostly advanced countries) or employed shorter time frame.
In this study, we examine the past trends of incidence, mortality and mortality-to-incidence ratio of breast cancer in females employing data from the Global Burden of Disease 2016 study for the period 1990–2016 for 102 countries. Progress in breast cancer and other neoplasms is often associated with country-level per capita income and countries are often categorised as per World Bank classification into low-, lower-middle, upper-middle and high-income countries [10]. We, however, conjecture that a country’s human development index—a composite measure of education (composite of mean years of schooling and expected years of schooling), income (gross national income (GNI) per capita) and health (life expectancy at birth)—is a better measure of its development and more broadly reflects the efficiency and efficacy of its health-care system. Figure 1 illustrates this point showing that MIR is predicted better by HDI (adj. R2 = 0.78) than its individual components, such as life expectancy (adj. R2 = 0.65), mean years of schooling (adj. R2 = 0.64) and expected years of schooling (adj. R2 = 0.60), and least by per capita income (adj. R2 = 0.48).

Data source: MIR was calculated by the author using crude mortality and incidence data of female breast cancer from the GBD 2016 study, and HDI data (and its components) was procured from the UNDP database
Relationship between MIR and HDI components in 2015, a MIR vs HDI, b MIR vs LE, c MIR vs Exp schooling, d MIR vs mean schooling, e MIR vs income. MIR mortality-to-incidence ratio, HDI Human Development Index, LE life expectancy at birth (in years), Exp schooling expected years of schooling, mean schooling mean years of schooling, income real gross national income (GNI) per capita at 2011 purchasing power parity (PPP) prices.
Therefore, we examine the past trends of breast cancer burden in terms of incidence, mortality (both all-age and age-standardised) and MIR across countries as per their HDI, which is expected to provide a more accurate assessment of the association between breast cancer burden in a country and its development status.
Materials and methods
We employ breast cancer data from the Global Burden of Disease (GBD) 2016 study, which provides location-, year-, age- and sex-wise estimates of cause of death for 195 countries and sub-national locations from 1990 to 2016 [1]. GBD 2016 employs all available data from sources such as vital registration, verbal autopsies, surveillance data and disease registry data, and uses Cause of Death Ensemble Model (CodeM) developed by Foreman et al. [11] to arrive at cause-specific mortality estimates. It uses separately estimated mortality-to-incidence ratio along with mortality estimates to arrive at cancer incidence [1, 2]. In this paper, we divide publicly available data of all-age crude death rate by all-age crude incidence rate of breast cancer in females from the GBD 2016 study to calculate the mortality-to-incidence ratio (MIR). We employ the data of breast cancer in females for 102 countries, which had incidence greater than 1000 cases in 2016 [12].Footnote 1 Combined, these countries accounted for 97% of global cancer deaths and 98% of incident cases in 2016. GBD estimates are provided with 95% uncertainty intervals (UI) and are reported inside square brackets along with mean estimates in this paper; where percentage change is reported alone, it is calculated from the mean estimates.
The development level of a country is measured using Human Development Index (HDI): a composite measure of education (composite of mean years of schooling and expected years of schooling), income (GNI per capita) and health (life expectancy at birth) [13]. Each of these individual indicators is converted to a scale of 0 (worst) to 1 (best) and the geometric mean of the three individual indicators gives the aggregate value of HDI for a given country in a year. Data pertaining to Human Development Index (HDI) for the period 1990–2015 is procured from the United Nations Development Program (UNDP) database for 100 countries, except for North Korea and Puerto Rico which did not have HDI values [13]. For descriptive as well as statistical analysis, countries were categorised into four groups as per UNDP classification of countries in 2015: very high (HDI > 0.800, 36 countries), high (0.700 < HDI < 0.799, 31 countries), medium (0.550 < HDI < 0.669, 18 countries) and low (HDI < 0.550, 15 countries) HDI categories.Footnote 2 All the analysis is done in MS-Excel 2016 and Stata 13.
Results
Globally, female deaths from breast cancer increased from 336857 [95% UI 319076–367033] in 1990 to 535341 [95% UI 506372–573133] in 2016 (Table 1). The incident cases increased from 815406 [95% UI 788481–857562] in 1990 to 1.68 million [95% UI 1.61–1.78] in 2016. In age-standardised terms, globally, the rate of breast cancer mortality (age-standardised mortality rate, ASMR) decreased from 17.2 [95% UI 16.4–18.9] in 1990 to 14.6 [95% UI 13.8–15.6] per 100,000 females in 2016, whereas age-standardised incidence rate (ASIR) increased from 41.0 [39.8–43.1] in 1990 to 45.6 [95% UI 43.6–48.2] in 2016. 102 countries combined in this study accounted for 1.65 million of the total 1.68 million incident cases and 517614 of the total 535341 global incident cases of female breast cancer in 2016.
HDI category-wise burden in 2016
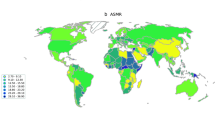
In terms of absolute numbers, very high HDI locations led all HDI categories followed by high HDI locations with low and medium HDI countries recording lesser numbers (both incidence and mortality) as compared to their developed counterparts (col I-II, Fig. 2). In terms of incidence and mortality, China (high HDI country) was the leading country with 290726 [95% UI 232995–333019] incident cases and 69872 [95% UI 58945–79505] deaths due to breast cancer in 2016 (Table 1). Interestingly, India a medium HDI country, ranks third in terms of breast cancer incidence (115922 [95% UI 104676–127235]) behind China and the USA (very high HDI country, 259634 [95% UI 249312–270812]). This is in contrast to mortality, which is more reminiscent of the strength of a country’s health-care system and its development, being higher in India (60462 [95% UI 51651–68759]) than in the USA (48780 [95% UI 46819–50963]), although the number of incident cases was higher in the USA than in India.
HDI category-wise mortality, incidence, ASIR, ASMR and MIR in 2016. ASIR age-standardised incidence rate, ASMR age-standardised mortality rate, MIR mortality-to-incidence ratio. Data pertains to low HDI (15 countries), medium HDI (18 countries), high HDI (31 countries) and very high HDI (36 countries) for the period 1990 to 2016 and is procured from the Global Burden of Disease study 2016. Countries were categorised into four groups as per HDI value in 2015: very high (HDI > 0.800), high (0.700 < HDI < 0.799), medium (0.550 < HDI < 0.669) and low (HDI < 0.550)
In terms of age-standardised incidence rate (ASIR), very high HDI locations occupied 19 of the top 20 positions, whereas in terms of age-standardised mortality rate (ASMR) 8 out of top 20 countries belonged to the very high HDI category (Table 1). The Netherlands and Belgium were the leading countries with ASIR of 117.2 [107.6–128.3] and 115.2 [95% UI 106.9–126.1] per 100,000 females, respectively, in 2016 (Fig. 2; Table 1). The age-standardised mortality rate (ASMR), however, was higher in the low HDI category than in other HDI categories with the highest ASMR recorded by Afghanistan at 35.4 [95% UI 14.6–64.5] per 100,000 females, followed by 31.5 [95% UI 19.0–51.3] per 100,000 females in Haiti in 2016. The age-standardised incidence rate (ASIR) was the lowest in North Korea at 13.1 [95% UI 9.6–19.7] with ASMR being the lowest in South Korea at 7.7 [4.8–11.4] per 100,000 females in 2016 (Table 1).
Mortality-to-incidence ratio (MIR), a representative indicator of 5-year survival, exhibited distinct patterns compared to absolute numbers and age-standardised rates with the highest MIR recorded in low HDI countries followed by medium HDI countries and the least MIR recorded in the very high HDI category (col v, Fig. 2). The majority of very high HDI locations recorded MIR lower than the global MIR of 0.32 in 2016, whereas the majority of low HDI countries were present at the bottom: 14 of 15 low HDI countries and 12 of the 18 medium HDI countries registered MIR greater than 0.5, whereas all countries in the high and very high HDI categories recorded MIR lower than 0.5 in 2016. In our sample of countries, Japan and South Korea recorded minimum MIR close to 0.18, closely followed by the USA with MIR of 0.19 in 2016. Country-wise, the highest MIR in the very high HDI category was recorded in Argentina with an MIR of 0.39, even greater than South Africa, a medium HDI country, which registered an MIR of 0.36. Among the high HDI locations, China recorded the lowest MIR of 0.24 in 2016 (which is even lower than many very high HDI countries), and Bosnia and Herzegovina (high HDI country) recorded the highest MIR in its category (0.47)—even greater than the MIR of few medium HDI countries. Myanmar, a medium HDI country, was the only country with an MIR greater than 1 in 2016, which was even greater than the MIR of many low HDI countries.
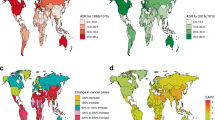
Temporal patterns: 1990–2016
Breast cancer exhibited distinct patterns of change over the period 1990 to 2016 when examined using different metrics: all age incidence and mortality, age-standardised rates and mortality-to-incidence ratio (MIR). Breast cancer mortality more than doubled in 43 countries out of 102 countries (more than tripled in ten countries) with Iran recording the maximum increase of 289% between 1990 and 2016 (Table 2 of “Appendix”). In terms of incidence, breast cancer burden more than tripled in 30 countries with 30 other countries experiencing more than the doubling of breast cancer incidence over the period 1990–2016; the largest increase of 855% was registered in Saudi Arabia, whereas the minimum change was experienced by Georgia where it decreased by 18.5% between 1990 and 2016. The breast cancer burden in already heavily burdened countries of China, India and the USA increased by 84, 130 and 12%, respectively, in terms of incidence and increased by 286, 188 and 40%, respectively, in terms of mortality over the period 1990–2016.Footnote 3
Looking at the temporal patters of ASMR, percent changes are not as big as that observed with respect to all-age incidence and mortality. 40 countries experienced a rise in ASMR between 1990 and 2016, and very high and high HDI locations underwent a reduction in ASMR barring few exceptions: ASMR increased by 32% in Saudi Arabia (very high HDI) and increased by 61% in Iran (high HDI location) (Table 2 in “Appendix”). ASMR decreased the most in Switzerland and the UK by 42 and 36%, respectively, over the period 1990 to 2016. ASIR decreased the most in Nepal by 11% from 1990 to 2016 and increased in 86 of 102 countries, with five witnessing a doubling of ASIR and Saudi Arabia and Iran witnessing a tripling of ASIR between 1990 and 2016 (Table 2 in “Appendix”).
In 102 countries, the incidence of breast cancer increased faster than mortality which resulted in the reduction of MIR in all but six countries over the period 1990–2016. The maximum reduction in MIR was recorded in Saudi Arabia from 0.72 in 1990 to 0.26 in 2016, followed by Libya and China, which experienced a reduction close to 53% between 1990 and 2016. The six countries (five in low HDI category) which experienced an increase in MIR were: Zimbabwe (13.8%), North Korea (11%), Angola (4.6%), Democratic Republic of Congo (3.9%), Ethiopia (2.73%) and Afghanistan (2.43%).
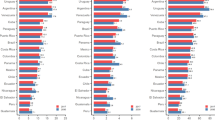
Bivariate association between MIR and HDI
MIR of breast cancer showed a negative gradient with HDI—low HDI countries recorded the highest MIR both in 1990 and 2016, followed by medium HDI countries, while very high HDI countries registered the lowest MIR with few exceptions (Fig. 3) (pairwise correlation, r = − 0.87). Over the period 1990–2015, as HDI increased for different countries, MIR of breast cancer decreased correspondingly, showing the significance of human development in reducing breast cancer burden and improving breast cancer survival. Pairwise correlation between MIR and HDI was the maximum in case of very high HDI countries with correlation coefficient of − 0.78, followed by medium HDI countries (r = − 0.62) and high HDI countries (r = − 0.58) with least correlation recorded for low HDI countries (r = − 0.55).
MIR vs HDI over the period 1990–2015. Mortality-to-incidence ratio (MIR) is calculated as the ratio of crude death rate and crude incidence rate. Countries were categorised into four groups as per HDI value in 2015: very high (HDI > 0.800), high (0.700 < HDI < 0.799), medium (0.550 < HDI < 0.669) and low (HDI < 0.550)
Discussion
In this paper, we examine the breast cancer incidence and mortality in females for 102 countries for the period 1990–2016 and use mortality-to-incidence ratio (MIR) as a representative indicator of breast cancer survival. We investigate a country’s progress in the fight against breast cancer vis-à-vis its development status, measured using the Human Development Index (HDI).
We observe that the global burden of breast cancer in females increased in terms of incidence and mortality between 1990 and 2016 with age-standardised rates either stagnated or decreased in the majority of countries examined in this study. The incidence (both all-age as well as age-standardised rate) of breast cancer is the highest in very high and high HDI countries, and correlates positively with country-specific HDI (r = 0.77). Breast cancer incidence more than tripled in 30 countries, whereas cancer mortality more than doubled in 43 out of 102 countries. Saudi Arabia recorded a maximum increase in incidence of 855% in the study period, whereas Iran registered a maximum increase of 289% in breast cancer mortality between 1990 and 2016 (Table 2 of “Appendix”). The incidence rates were the highest in developed countries led by the Netherlands and Belgium with ASIR of 117.2/100,000 and 115.2/100,000 females, respectively, in 2016. The age-standardised mortality rate (ASMR), however, was highest in the low HDI category led by Afghanistan with ASMR of 35.4/100,000 females, followed by 31.5/100,000 females in Haiti in 2016.
The breast cancer incidence, although highest in developed countries, is also on the rise in low and medium HDI countries, exemplified by countries such as India, a medium HDI country, which ranks third in terms of incidence (behind only China and the USA) and second behind China in terms of all-age mortality. What explains this rising incidence of breast cancer in low and medium HDI countries? There are multiple factors behind the increasing incidence of breast cancer in these countries: increased longevity, improved cancer registration and improving awareness towards breast cancer. Other likely reasons for increased incidence of breast cancer in developing countries is westernisation of lifestyle, characterised by a change in reproductive patterns such as earlier age at menarche, later first birth, lower parity, shorter duration of breastfeeding [14], and obesity and overweight [15]. The problem of the growing incidence of breast cancer in low and medium HDI countries is also associated with low survival rates [3] which is also evidenced by high MIR in these countries.
Globally, MIR reduced from 0.41 in 1990 to 0.32 in 2016; though all HDI categories underwent a reduction, high HDI locations experienced the steepest fall with low HDI countries recording the least progress in 5-year breast cancer survival measured using MIR (Fig. 6 in “Appendix”). Human development measured using HDI is strongly correlated with MIR implying that all the factors (health, education and income) incorporated in HDI, and not a single factor such as per capita income, are significant in determining the survival of breast cancer patients. On average, it is expected that health-care system’s quality and access are similar in countries having similar HDI value and it also proved to be a good predictor of breast cancer survival in this study (R2 = 0.76). In our analysis, however, there were a few exceptions to this relationship, with few countries performing better or worse than predicted by their HDI. For instance, South Korea in very high HDI category, China in high HDI category, Indonesia in medium HDI category and Nigeria in low HDI category performed better in terms of MIR than that predicted by their HDI, whereas Argentina and Russia in very high, Bosnia and Herzegovina in high, Myanmar in medium, and Ethiopia and Afghanistan in low HDI category performed worse than that predicted by their HDI. It implies that factors other than longevity, years of schooling and per capita income also explain the survival rate of breast cancer. Besides HDI, the survival rate of breast cancer depends upon country-specific health-care factors such as access to screening, early detection, case-specific treatment (Her-2 positive or ER positive etc) and availability of infrastructure (radiological instruments, physicians etc). South Korea, for instance, having the lowest ASMR as well as low MIR (indicating high survival rate), started National Cancer Screening Programme in 2002, which resulted in better prognosis of breast cancer and thereby higher survival rate [16].Footnote 4
The stage of breast cancer at first diagnosis crucially determines its prognosis and differs markedly across countries—about 75% women in developing countries are diagnosed first in stage III and IV, whereas 70% of women in North America are diagnosed in stage 0 or 1, which results in better prognosis in developed regions as compared to the developing ones [3, 17, 18]. As far as early detection is concerned, WHO identified two strategies: screening and clinical downstaging [19]. Screening programs focus on detecting cancer in asymptomatic population, whereas clinical downstaging aims at ensuring that a patient with early symptoms meets an oncologist. In developed countries, breast cancer screening rates are high and screening has been quite instrumental in detecting cancer early and thereby improving survival in developed countries; the screening programs, however, are also found to be susceptible to high false positive rate and overdiagnosis/overtreatment [20,21,22,23,24]. Moreover, the cost-effectiveness of population-wide screening mammography is further questioned in developing countries; considering the low incidence rate per 100,000 females (due to large population) in these countries, the cost per life saved due to population-wide screening therefore, becomes astronomically high in these already resource-constrained economies [25]. Other alternatives to screening mammography are breast self-examination (BSE) and clinical breast examination (CBE). These methods are a cost-effective alternative to screening mammography; their efficacy, however, in early diagnosis and improved survival is still inconclusive [25, 26]. WHO’s second early-detection strategy which calls for clinical downstaging to improve survival rates seems to be a more suitable and cost-effective alternative to screening mammography in low resource economies [27, 28].
Lastly, the high MIR and ASMR in low and medium HDI countries may also be reflective of other challenges specific to these countries. First, universal health coverage is positively correlated with HDI (Fig. 4a) and is negatively correlated with mortality-to-incidence ratio (MIR; Fig. 4b). Due to lack of universal health coverage in low and medium HDI countries, a large percentage of health expenditure incurred is spent from one’s own pocket (Fig. 4c), which is also evidenced by high out-of-pocket (OOP) expenditure in low and medium HDI countries [29]. Second, most of the cancer care units in low and medium HDI countries are located in urban areas, making it more difficult and costlier for rural patients to access quality care. Third, there is low awareness (knowledge) of breast cancer. For instance, low percent of women in these countries are aware that a painless lump on the breast may be symptomatic of breast cancer, and if suspicious these women first reach out to a local healer after detecting any abnormality on the breast or nipple which causes a delay in diagnosis and thereby poor prognosis ensues. Therefore, improving breast cancer survival in these countries require strategies that focus on increased awareness, universal health coverage, improved access to either publicly funded or affordable screening programs and treatment paradigms.

Data source: MIR is calculated by the author using crude mortality and incidence data, HDI data is procured from the UNDP database and UHC data is procured from the WDI database of World Bank which in turn was compiled from Hogan et al. [30]. OOP data is also from the WDI database of World Bank
Relationship between MIR and HDI with UHC: a UHC vs HDI, b MIR vs UHC, c OOP vs HDI. MIR mortality-to-incidence ratio, HDI Human Development Index, UHC universal health coverage service index, OOP out-of-pocket expenditure as percent of current health expenditure.
Conclusion
This paper examines breast cancer burden in females in 102 countries for the period 1990–2016. We find that the incidence of breast cancer is higher in developed countries (high/very high HDI), but is also increasing in low and medium HDI countries. Breast cancer mortality rates were the highest in low and medium HDI countries, which was also supported by high MIR (proxy for survival rate) in these countries. Based on past trends, breast cancer incidence is expected to escalate further in future posing multifaceted challenges to already resource-constrained least developed countries. In the fight against breast cancer, a multipronged strategy must be adopted which focuses on improved human development, increases breast cancer awareness, universal health coverage and, lastly, breast cancer screening and treatment approaches which suit low-resource environments.
Limitations
This study employed data available from the Global Burden of Disease (GBD) study, which draws strength from data availability from cancer registries. The data from cancer registries, however, is far from complete in many resource-poor economies. This incomplete data yields mortality and incidence estimates with wide uncertainty intervals (UIs). This limitation, however, can be remedied by improved cancer registration in low/medium income countries which will help us gauge the current state of fight against cancer more accurately.
Notes
1000 cases are chosen so as to exclude countries with too few cancer cases as it may lead to too large or too small MIR values which may not truly reflect countries’ development status and may distort main conclusions of the paper.
National Cancer Screening Program in Georgia also one of the successful screening program which resulted in downstaging of breast cancer and improved survival rate. Source: http://www.gnsc.ge/?act=page&id=44&lang=en (Accessed 18 Oct 2018).
References
GBD 2016 Cause of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2016;390(10100):1151–210.
Global Burden of Disease Cancer Collaborators. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990–2016. a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2018. https://doi.org/10.1001/jamaoncol.2018.2706.
Sankaranarayanan R, Swaminathan R, Brenner H, Chen K, Chia KS, Chen JG, et al. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol. 2010;11(2):165–73.
Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML, Visser O, Verbeek AL, Kiemeney LA. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Public Health. 2010;21(5):573–7.
Chen SL, Wang SC, Ho CJ, Kao YL, Hsieh TY, Chen WJ, et al. Prostate cancer mortality-to-incidence ratios are associated with cancer care disparities in 35 countries. Sci Rep. 2017;7:40003.
Wang SC, Sung WW, Kao YL, Hsieh TY, Chen WJ, Chen SL, et al. The gender difference and mortality-to-incidence ratio relate to health care disparities in bladder cancer: National estimates from 33 countries. Sci Rep. 2017;7(1):4360.
Tsai MC, Wang CC, Lee HL, Peng CM, Yang TW, Chen HY, et al. Health disparities are associated with gastric cancer mortality-to-incidence ratios in 57 countries. World J Gastroenterol. 2017;23(44):7881.
Wang CC, Tsai MC, Peng CM, Lee HL, Chen HY, Yang TW, et al. Favorable liver cancer mortality-to-incidence ratios of countries with high health expenditure. Eur J Gastroenterol Hepatol. 2017;29(12):1397–401.
Sunkara V, Hebert JR. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer. 2015;121(10):1563–9.
Ginsburg O, Bray F, Coleman MP, Vanderpuye V, Eniu A, Kotha SR, et al. The global burden of women’s cancers: a grand challenge in global health. Lancet. 2017;389(10071):847–60.
Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10(1):1.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016. (GBD 2016). 2017. Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME). http://ghdx.healthdata.org/gbd-results-tool. Accessed 5 July 2018.
United Nations Development Program (UNDP). Human Development Database. 2018. http://hdr.undp.org/en/data#. Accessed 30 June 2018 and 1 July 2018.
Porter P. “Westernizing” women’s risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358(3):213–6.
Arnold M, Pandeya N, Byrnes G, Renehan AG, Stevens GA, Ezzati M, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 2015;16(1):36–46.
Park SK, Kim Y, Kang D, et al. Risk factors and control strategies for the rapidly rising rate of breast cancer in Korea. J Breast Cancer. 2011;14:79–87.
Hortobagyi GN, de la Garza Salazar J, Pritchard K, Amadori D, Haidinger R, Hudis CA, et al. The global breast cancer burden: variations in epidemiology and survival. Clin Breast Cancer. 2005;6(5):391–401.
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56(2):106–30.
WHO Guide for effective programmes; cancer control: knowledge into action; module 3: early detection (free full text). 2018. http://www.who.int/cancer/publications/cancer_control_detection/en/. Accessed 6 Aug 2018.
Jørgensen KJ, Zahl PH, Gøtzsche PC. Overdiagnosis in organised mammography screening in Denmark. A comparative study. BMC Womens Health. 2009;9(1):36.
Gøtzsche PC, Nielsen M. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2009. https://doi.org/10.1002/14651858.CD001877.pub3.
Jørgensen KJ, Zahl PH, Gøtzsche PC. Breast cancer mortality in organised mammography screening in Denmark: comparative study. BMJ. 2010;340:c1241.
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005.
Kalager M, Adami HO, Bretthauer M, Tamimi RM. Overdiagnosis of invasive breast cancer due to mammography screening: results from the Norwegian screening program. Ann Intern Med. 2012;156(7):491–9.
Corbex M, Burton R, Sancho-Garnier H. Breast cancer early detection methods for low and middle-income countries, a review of the evidence. Breast. 2012;21(4):428–34.
Sankaranarayanan R, Ramadas K, Thara S, Muwonge R, Prabhakar J, Augustine P, Venugopal M, Anju G, Mathew BS. Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst. 2011;103(19):1476–80.
Luthar UK. Clinical downstaging of cancer of the uterine cervix e an interim strategy for developing countries. In: Proceedings of the UICC congress. 1994.
Devi BCR, Tang TS, Corbex M. Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak, Malaysia. Ann Onc. 2007;18(7):1172–6.
World Bank Database. 2018. WDI data. http://databank.worldbank.org/data. Accessed 25 July 2018.
Hogan DR, Stevens GA, Hosseinpoor AR, Boerma T. Monitoring universal health coverage within the Sustainable Development Goals: development and baseline data for an index of essential health services. Lancet Glob Health. 2018;6(2):e152–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of the paper declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Figs. 5 and 6 and Tables 2 and 3.
HDI groupwise annual percentage change of breast cancer burden, 1990–2016. ASIR age-standardised incidence rate, ASMR age-standardised mortality rate, MIR mortality-to-incidence ratio. Countries were categorised into four groups as per HDI value in 2015: very high (HDI > 0.800), high (0.700 < HDI < 0.799), medium (0.550 < HDI < 0.669) and low (HDI < 0.550)
HDI category-wise temporal movement of mortality-to-incidence ratio (MIR), 1990–2016. Data pertains to aggregate of data for low HDI (15) countries, medium HDI (18) countries, high HDI (31) countries and very high HDI (36) countries for the period 1990 to 2016 and is procured from Global Burden of Disease study 2016. Countries were categorised into four groups as per HDI value in 2015: very high (HDI > 0.800), high (0.700 < HDI < 0.799), medium (0.550 < HDI < 0.669) and low (HDI < 0.550)
About this article
Cite this article
Sharma, R. Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990–2016: evidence from Global Burden of Disease Study 2016. Breast Cancer 26, 428–445 (2019). https://doi.org/10.1007/s12282-018-00941-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-018-00941-4