Abstract
Purpose
To evaluate the distribution pattern of kinetic parameters in breast cancers with various molecular subtypes.
Materials and methods
This study was approved by institutional review board and was compliant with HIPAA. We classified 192 invasive breast cancers of 186 patients into four molecular subtypes using hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) results and evaluated the distribution pattern of kinetic parameters (percent volume of kinetic types relative to the tumor volume) in the molecular subtypes.
Results
In the delayed phase, all three types of kinetic parameter (persistent, plateau, and washout pattern) were observed in each molecular subtype without any dominant type of kinetic parameter. The percentages of washout pattern in the HR+ and HER2− type and triple negative (TN) cancers tended to be lower than those in the other molecular subtype cancers.
Conclusion
Each molecular subtype of invasive breast cancer showed a heterogeneous kinetic pattern in dynamic-contrast magnetic resonance imaging (MRI). The HR+/HER2− cancers and the TN cancers had relatively lower percentages of washout pattern. When a manual assessment of the kinetic parameters is performed, close attention should be paid in order to identify the malignant washout kinetic pattern, particularly in HR+/HER2− cancer and TN cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a heterogeneous disease. Several studies using microarray technology and cluster analyses of gene profiling have provided a new classification of breast cancer: the molecular subtype [1–4]. These studies have shown that several breast cancer subtypes that vary in gene expression and clinical course are identifiable [1–4]. In this classification, at least four major subtypes are identified: Luminal A type, Luminal B type, HER2 (human epidermal growth factor receptor 2) type, and Basal cell type [1–4]. Immunohistochemical (IHC) staining has been shown to be a reliable surrogate for these subtypes [3–5]. Clinically, the term “triple-negative cancer” (TN) has been used for the Basal cell type as a surrogate.
The two Luminal subtypes are the most common subtypes, and they are more often low-grade compared to the HER2 and Basal cell subtypes. Luminal subtypes carry a relatively better prognosis than the others, but the Luminal B type tends to be higher grade than the Luminal A type and has a worse prognosis than Luminal A [3, 4]. The HER2 type is more likely to be high-grade and poorly differentiated [4]. The Basal cell type (triple-negative cancer) has a high proliferation rate, is not amenable to conventional target therapies, and has a poor prognosis [3, 4]. In addition, each breast cancer is unique in its appearance, due not only to the difference in subtype, but also to various components in the tumor such as necrosis, fibrosis, hemorrhage, and mucin.
We speculated that when breast cancer contains such components, the kinetic parameters obtained in a dynamic study using post-contrast breast magnetic resonance imaging (MRI) will be heterogeneous. The typical malignant kinetic pattern shows a rapid uptake in the early phase and a washout pattern in the delayed phase, but it is also well known that the kinetic pattern is influenced by the various histological subtypes and tumor components [6–16]. In Japan, when we assess the kinetic parameters, the region of interest (ROI) is usually placed manually. CADstream, a dedicated breast MRI workstation, can automatically assess the kinetic parameters in whole breast lesions. With the CADstream, color-overlay (an angiomap) shows the changes in signal intensity over time.
Some studies have shown the correlation of radiologic findings with each molecular subtype of breast cancer [17–22]. However, to the best of our knowledge, there has been no study that evaluated the association between the distribution of kinetic parameters and each molecular subtype of breast cancer. If there are some associations, they may indicate the molecular subtype, and this indication may be useful for therapeutic planning for breast cancer. The present study was conducted to clarify the distribution patterns of kinetic parameters in regard to the molecular subtypes of breast cancer.
Materials and methods
Patients
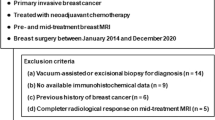
This retrospective study was approved by institutional review board at the University of Chicago and was compliant with HIPAA (the US Health Insurance Portability and Accountability Act of 1996). Informed consent was waived. Between January 2010 and August 2011, 236 cases of breast cancer were proven by biopsy or surgery in 228 women (eight of the 228 women had bilateral breast cancers) who underwent breast MRI at the University of Chicago. Of these 236 cancers, 34 were excluded from our study because the final pathology was pure ductal carcinoma in situ (DCIS), and 10 cancers were excluded because the distribution of kinetic parameters was not available. The exclusion of these 44 cancers left 192 cases of invasive breast cancer from 186 women (range 23–87 years old, mean 58.1 years old) that comprised the study population.
MRI technique
During the study period, we used two different MRI techniques with a dedicated breast coil and the patient in the prone position. In 97 patients, MR exams were performed using a 1.5 Tesla system (Achieva 1.5T, Philips Healthcare). The imaging protocol obtained axial, fast spin-echo, T2-weighted images (TR/TE 2000/326, echo train length 15, slice thickness 2 mm, matrix 480 × 480, FOV 360 mm), and a dynamic contrast-enhanced study was performed using one pre- and six post-contrast-enhanced, axial, T1-weighted images with a 3D gradient-echo sequence with fat suppression (5.5/2.7, flip angle 10°, matrix 480 × 480, slice thickness 2 mm, FOV 360 mm, acquisition time 75 s).
In 95 patients, MR exams were performed using a 3 Tesla system (Achieva 3T Tx, Philips Healthcare). The image protocol obtained axial, fast spin-echo, T2-weighted images (TR/TE 2000/270, echo train length 15, slice thickness 1.6 mm, matrix 448 × 448, FOV 340 mm), and a dynamic contrast-enhanced study was performed using one pre- and five post-contrast-enhanced, axial, T1-weighted images with a 3D gradient-echo sequence with fat suppression (4.9/2.47, flip angle 10°, matrix 448 × 448, slice thickness 1.6 mm, FOV 340 mm, acquisition time 65 s). The contrast material was injected intravenously [0.1 mmol/kg of gadodiamide (Omniscan, GE Healthcare)] and followed by a 20-mL saline flush at a rate of 2 mL/s. In the dynamic contrast-enhanced study, the first post-contrast phase was scanned just after the contrast material injection.
Postprocessing
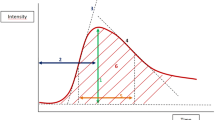
All MRI scans were collected and sent to a dedicated Breast MR workstation (CADstream, version 4.1.3, Merge Healthcare, Chicago, IL). With the CADstream, a color overlay (an angiomap) showing the changes in signal intensity over time is automatically made in all slices using a predefined minimum threshold (Figs. 1b, 2b). We defined the minimum threshold as a 50 % increase in relative enhancement in the initial phase of the enhancement (i.e., the first 2 min or the second phase of the dynamic contrast-enhanced study). When the relative enhancement increase was 50–100 % in the initial phase, we defined it as “medium uptake”, and when it was more than 100 %, we defined it as “rapid uptake”. When the signal intensity continued to show an increase (10 % or more) at the delayed phase of the enhancement (at 5 min after the contrast injection), we defined it as “persistent”, and when the signal intensity remained constant at the delayed phase, we defined it as a “plateau”. When the signal intensity showed a decrease (10 % or less) at delayed phase, it was defined as a “washout”.
Type 3 (ER−, PgR− and HER2+) invasive breast carcinoma (invasive ductal carcinoma) in a 58-year-old patient. a A post-contrast subtracted, fat-suppressed, axial, T1-weighted image shows an enhancing mass with an irregular shape and margin. b In the color-coded image, the mass appears heterogeneous and has a predominant washout pattern (red washout pattern, yellow plateau pattern, blue persistent pattern) (color figure online)
Type 1 (ER+, PgR+ and HER2−) breast carcinoma (invasive lobular carcinoma) in a 62-year-old patient. a A post-contrast subtracted, fat-suppressed, axial, T1-weighted image shows an enhancing mass with an irregular shape and margin. b In the color-coded image, the mass appears heterogeneous and has a predominant persistent pattern (red washout pattern, yellow plateau pattern, blue persistent pattern) (color figure online)
By choosing the “volumes” option in the CADstream and clicking on a voxel in the tumor, the CADstream program automatically provides the 3D volume of the tumor by segmenting continuous enhancing voxels. Clicking on a voxel in the tumor was performed by one radiologist (K.Y.). The CADstream also measures the distribution of kinetic parameters in terms of percent volume for six kinetic types (medium-persistent, medium-plateau, medium-washout, rapid-persistent, rapid-plateau, and rapid-washout) relative to the segmented tumor (Figs. 1b, 2b).
All images were independently evaluated by two experienced radiologists (K.Y. and H.A.). The molecular subtype of each lesion was blinded during these evaluations. If the patient had multiple lesions in the ipsilateral breast, the largest lesion was used for the analysis as an index lesion. If different assessments were assigned by the two radiologists, a consensus was reached after the findings were discussed.
Pathology
All pathology data were based on pathological reports collected from the electronic medical records of our institution. Of the 192 cases, there were 39 cases of invasive ductal carcinoma (IDC), 110 cases of IDC with in situ components, 34 cases of invasive lobular carcinoma (ILC) or IDC with lobular components, six cases of mucinous carcinoma or IDC with mucinous components, two cases of metaplastic carcinoma, and one case of poorly differentiated carcinoma. We classified these 192 invasive breast cancers into four molecular subtypes.
At first, we tried to classify the subtypes according to the St. Gallen International Expert Consensus 2010 [23], but our data of the cell proliferation marker Ki67 were not sufficient. Therefore, the classification of molecular subtypes was only based on the results of IHC staining of estrogen receptor (ER), progesterone receptor (PgR), and human epidermal growth factor receptor 2 (HER2), and the value of HER2/chromosome 17 fluorescence in situ hybridization (FISH). The IHC staining of ER and PgR was considered positive when the expression was 10 % or greater. For the IHC staining of HER2, which was scored from 0 to 3+, 3+ was considered positive and 0 and 1+ were considered negative. If the staining was scored 2+, greater than 2.2 in the value of FISH was considered positive.
The classification of the four molecular subtypes was performed as follows; type 1 ER+ (positive) and/or PgR+ and HER2− (negative), type 2 ER+ and/or PgR+ and HER2+, type 3 ER−, PgR− and HER2+, type 4 [triple-negative (TN) cancers] negative for ER, PgR and HER2 [5, 23]. Of the 192 cases, 121 cases were classified as type 1, 21 cases were classified as type 2, 10 cases were classified as type 3, and 40 cases were classified as TN cancer. The pathology data are summarized in Table 1.
Statistical analysis
We performed a statistical evaluation of the differences in median percentages of each kinetic parameter within the molecular subtypes using the Kruskal–Wallis nonparametric test; p values <0.05 were considered significant. The PASW statistics 18 software package (SSPS Inc., Chicago, IL) was used for this analysis.
Results
The mean size of all lesions was 36.6 mm (range 3–121 mm). Of the 192 lesions, there were one focus lesion, 150 mass lesions and 41 non-mass-like enhancement lesions. In the manual assessment of kinetic parameters in the initial phase, 14 lesions (nine type 1, one type 2, zero type 3, and four type 4 lesions) were identified as having the medium uptake pattern, and 178 lesions (112 type 1, 20 type 2, 10 type 3 and 36 type 4 lesions) had the rapid uptake pattern. In the manual assessment of kinetic parameters in the delayed phase, 32 lesions (23 type 1, three type 2, zero type 3 and six type 4 lesions) were found to have the persistent pattern; 18 lesions (14 type 1, two type 2, three type 3, and zero type 4 lesions) had the plateau pattern and 142 lesions (84 type 1, 16 type 2, eight type 3, and 34 type 4 lesions) showed the washout pattern.
The mean and median percentages of each kinetic parameter according to molecular subtype are summarized in Table 2. In the initial phase, the abundant rapid uptake pattern was more common than the medium uptake pattern in all four molecular subtypes. There were no significant differences in the median percentages of medium uptake and rapid uptake within the molecular subtypes (p = 0.201 and 0.202, respectively). In the delayed phase, each molecular subtype appeared heterogeneous in terms of kinetic distribution; all three types (persistent, plateau, and washout pattern) of kinetic parameters were observed in each molecular subtype without any type of dominant kinetic parameter (Figs. 1, 2, 3).
a A chart of kinetic parameters in the initial phase shows that each molecular subtype has more of the rapid uptake pattern than the medium uptake pattern. b A chart of kinetic parameters in the delayed phase shows that each molecular subtype has internal heterogeneity of kinetic parameters. The mean percentages of the washout pattern in the type 1 (ER+ and/or PgR+ and HER2−) and type 4 (triple-negative cancers) were lower than those in the type 2 (ER+ and/or PgR+ and HER2+) and type 3 (ER−, PgR− and HER2+)
The mean percentages of washout pattern in type 1, type 2, type 3, and type 4 were 24.15 (median 23.00) %, 37.52 (median 41.00) %, 38.00 (median 42.00) %, and 31.08 (33.50) %, respectively, and there was a significant difference in the median percentage of the washout pattern within the molecular subtypes (p = 0.014). The mean and median percentages of the washout pattern in type 1 and type 4 were lower than those in type 2 and type 3 (Figs. 1, 2, 3). There were no significant differences in the median percentages of the persistent pattern or plateau pattern within the molecular subtypes (p = 0.121 and 0.991, respectively).
Discussion
The results of the present study show that all four of the breast cancer molecular subtypes we studied have internal heterogeneity in the distribution of dynamic kinetic parameters, and that the percentages of the washout pattern in the type 1 [hormone receptor (HR)+ and HER2−) and type 4 (TN cancer) cancers tended to be lower than those in the type 2 (HR+ and HER2+) and type 3 (HR− and HER2+) cancers. This tendency might have been caused by the variety of histological components in each molecular subtype.
Invasive breast cancers including lobular components and mucinous components were most frequently seen in the type 1 cancers (82 and 83 %, respectively).
In previous reports, large populations of invasive lobular carcinoma and mucinous carcinoma were characterized as HR+ and HER2− (equal to our type 1) [24–29]. Invasive lobular carcinoma tends to show a non-washout pattern more often than invasive ductal carcinoma in dynamic contrast MRI [12, 13]; this may be caused by the invasion of cancer cells through fibrous connective tissue [25]. Mucinous carcinoma also tends to show a non-washout pattern (particularly the persistent pattern) because of its mucin component, which causes slow diffusion of the contrast material [14, 15]. In addition, DCIS shows a variable enhancement pattern from washout to persistent pattern [16]. In our present study, DCIS was most frequently associated with IDC in the type 1 cancers. We suspect that these variable histological components in the type 1 cancers are the cause of its heterogeneity and less-frequent washout pattern.
Here, the type 4 (TN cancer) cancers also tended to show the washout pattern less frequently compared to the type 2 and 3 cancers. TN cancer is highly associated with central scarring and tumor necrosis [30, 31]. Uematsu et al. [18] reported that TN cancer tends to show a persistent pattern, possibly due to the presence of components such as central scarring and tumor necrosis.
In our study, each molecular subtype appeared heterogeneous in terms of kinetic distribution. All three types of delayed-phase kinetic parameters (persistent, plateau, and washout pattern) were observed in each molecular subtype without any type of dominant kinetic parameter. It is thus difficult to suggest the molecular subtype from our results using CADstream assessments. However, the CADstream can automatically assess the kinetic parameters in whole breast lesions, and we can more easily see the heterogeneous distribution of kinetic parameters and identify the malignant washout pattern using the CADstream compared to with manual assessment.
According to the American College of Radiology Breast Imaging Reporting and Data System (BI-RADS), in the kinetic curve assessment in MRI, the ROI should be placed on the fastest-enhancing portion of the lesion or the most suspicious washout curve pattern in the lesion [10]. However, if the kinetic pattern is heterogeneous, and the percentage of washout parameter is relatively lower within a cancer such as a type 1 (HR+ and HER2−) or TN cancer, the typical malignant washout kinetic pattern may be missed. Thus, close attention should be paid to identification of the malignant kinetic pattern in cancers that have a heterogeneous kinetic pattern, when the kinetic parameters must be obtained through a manual assessment.
In the manual assessment of delayed-phase parameters, we observed a predominant pattern: 37 of the 121 type 1 lesions were assessed as showing the non-washout pattern. However, the lesions with the non-washout pattern that we assessed manually may include a small amount of the true washout pattern because of intratumoral heterogeneity. When only manual assessments (without a color-coded map) of internal heterogeneity are conducted, such discrepancies may occur.
Our study has some limitations; one is that there was a relatively small number of type 3 (HR− and HER+) cases (n = 10) compared to the other subtypes. Further studies with large numbers of cases are needed for more meaningful results. Another limitation is the lack of comparison with benign lesions. However, previous studies reported that benign breast lesions mainly show homogeneous enhancement in post-contrast MRI morphologically [9, 32]. On this basis, we suspect that many benign breast lesions show a more homogeneous distribution pattern than breast cancer in this kinetic analysis. Further comparison studies of each molecular subtype of cancer and benign lesions may help clarify this issue.
In conclusion, each of the four molecular subtypes of invasive breast cancer studied here had particular heterogeneous kinetic parameters. The percentages of the washout pattern in the type 1 (HR+ and HER2−) and type 4 (TN) cancers tended to be lower than those in the type 2 (HR+ and HER2−) and type 3 (HR− and HER2+) cancers. We should pay close attention to identification of the malignant washout kinetic pattern in cancers that have a heterogeneous kinetic pattern, particularly in type 1 and TN cancers when a manual assessment of the kinetic parameters is performed.
References
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–74.
Perou CM, Borresen-Dale AL. Systems biology and genomics of breast cancer. Cold Spring Harb Perspect Biol. 2011;3:2.
Brenton JD, Carey LA, Ahmed AA, Caldas C. Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol. 2005;23:7350–60.
Tamimi RM, Baer HJ, Marotti J, Galan M, Galaburda L, Fu Y, Deitz AC, et al. Comparison of molecular phenotypes of ductal carcinoma in situ and invasive breast cancer. Breast Cancer Res. 2008;10:R67.
Kuhl CK, Mielcareck P, Klaschik S, Leutner C, Wardelmann E, Gieseke J, et al. Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology. 1999;211:101–10.
Liu PF, Debatin JF, Caduff RF, Kacl G, Garzoli E, Krestin GP. Improved diagnostic accuracy in dynamic contrast enhanced MRI of the breast by combined quantitative and qualitative analysis. British J Radiol. 1998;71:501–9.
Siegmann KC, Muller-Schimpfle M, Schick F, Remy CT, Fersis N, Ruck P, et al. MR imaging-detected breast lesions: histopathologic correlation of lesion characteristics and signal intensity data. Am J Roentgenol. 2002;178:1403–9.
Baum F, Fischer U, Vosshenrich R, Grabbe E. Classification of hypervascularized lesions in CE MR imaging of the breast. Eur Radiol. 2002;12:1087–92.
American College of Radiology (ACR) BI-RADS. Breast Imaging Atlas. In: ACR Breast Imaging Reporting and Data System, editor. Magnetic resonance imaging. Reaston: American College of Radiology; 2003.
Caramella T, Chapellier C, Ettore F, Raoust I, Chamorey E, Balu-Maestro C. Value of MRI in the surgical planning of invasive lobular breast carcinoma: a prospective and a retrospective study of 57 cases: comparison with physical examination, conventional imaging, and histology. Clin Imaging. 2007;31:155–61.
Dietzel M, Baltzer PA, Vag T, Gröschel T, Gajda M, Camara O, et al. Magnetic resonance mammography of invasive lobular versus ductal carcinoma: systematic comparison of 811 patients reveals high diagnostic accuracy irrespective of typing. J Comput Assist Tomogr. 2010;34:587–95.
Mann RM, Veltman J, Huisman H, Boetes C. Comparison of enhancement characteristics between invasive lobular carcinoma and invasive ductal carcinoma. J Magn Reson Imaging. 2011;34:293–300.
Monzawa S, Yokokawa M, Sakuma T, Takao S, Hirokaga K, Hanioka K, et al. Mucinous carcinoma of the breast: MRI features of pure and mixed forms with histopathologic correlation. Am J Roentgenol. 2009;192:W125–31.
Okafuji T, Yabuuchi H, Sakai S, Soeda H, Matsuo Y, Inoue T, et al. MR imaging features of pure mucinous carcinoma of the breast. Eur J Radiol. 2006;60:405–13.
Jansen SA, Newstead GM, Abe H, Shimauchi A, Schmidt RA, Karczmar GS. Pure ductal carcinoma in situ: kinetic and morphologic MR characteristics compared with mammographic appearance and nuclear grade. Radiology. 2007;245:684–91.
Yang WT, Dryden M, Broglio K, Gilcrease M, Dawood S, Dempsey PJ, et al. Mammographic features of triple receptor-negative primary breast cancers in young premenopausal women. Breast Cancer Res Treat. 2008;111:405–10.
Uematsu T, Kasami M, Yuen S. Triple-negative breast cancer: correlation between MR imaging and pathologic findings. Radiology. 2009;250:638–47.
Ko ES, Lee BH, Kim HA, Noh WC, Kim MS, Lee SA. Triple-negative breast cancer: correlation between imaging and pathological findings. Eur Radiol. 2010;20:1111–7.
Dogan BE, Gonzalez-Angulo AM, Gilcrease M, Dryden MJ, Yang WT. Multimodality imaging of triple receptor-negative tumors with mammography, ultrasound, and MRI. Am J Roentgenol. 2010;194:1160–6.
Tamaki K, Ishida T, Miyashita M, Amari M, Ohuchi N, Tamaki N, et al. Correlation between mammographic findings and corresponding histopathology: potential predictors for biological characteristics of breast diseases. Cancer Sci. 2011;102:2179–85.
Choi YJ, Seong MH, Choi SH, Kook SH, Kwag HJ, Park YL, et al. Ultrasound and clinicopathological characteristics of triple receptor-negative breast cancers. J Breast Cancer. 2011;14:119–23.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, et al. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Zhao H, Langerod A, Ji Y, Nowels KW, Nesland JM, Tibshirani R, et al. Different gene expression patterns in invasive lobular and ductal carcinomas of the breast. Mol Biol Cell. 2004;15:2523–36.
Weigelt B, Geyer FC, Natrajan R, Lopez-Garcia MA, Ahmad AS, Savage K, et al. The molecular underpinning of lobular histological growth pattern: a genome-wide transcriptomic analysis of invasive lobular carcinomas and grade- and molecular subtype-matched invasive ductal carcinomas of no special type. J Pathol. 2010;220:45–57.
Weigelt B, Horlings HM, Kreike B, Hayes MM, Hauptmann M, Wessels LF, et al. Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol. 2008;216:141–50.
Yu J, Dabbs DJ, Shuai Y, Niemeier LA, Bhargava R. Classical-type invasive lobular carcinoma with HER2 overexpression: clinical, histologic, and hormone receptor characteristics. Am J Clin Pathol. 2011;136:88–97.
Di Saverio S, Gutierrez J, Avisar E. A retrospective review with long term follow up of 11,400 cases of pure mucinous breast carcinoma. Breast Cancer Res Treat. 2008;111:541–7.
Bae SY, Choi MY, Cho DH, Lee JE, Nam SJ, Yang JH. Mucinous carcinoma of the breast in comparison with invasive ductal carcinoma: clinicopathologic characteristics and prognosis. J Breast Cancer. 2011;14:308–13.
Fulford LG, Easton DF, Reis-Filho JS, Sofronis A, Gillett CE, Lakhani SR, et al. Specific morphological features predictive for the basal phenotype in grade 3 invasive ductal carcinoma of breast. Histopathology. 2006;49:22–34.
Livasy CA, Karaca G, Nanda R, Tretiakova MS, Olopade OI, Moore DT, et al. Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma. Mod Pathol. 2006;19:264–71.
Tozaki M, Igarashi T, Fukuda K. Positive and negative predictive values of BI-RADS-MRI descriptors for focal breast masses. Magn Reson Med Sci. 2006;5:7–15.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yamaguchi, K., Abe, H., Newstead, G.M. et al. Intratumoral heterogeneity of the distribution of kinetic parameters in breast cancer: comparison based on the molecular subtypes of invasive breast cancer. Breast Cancer 22, 496–502 (2015). https://doi.org/10.1007/s12282-013-0512-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-013-0512-0