Abstract
Objectives
There are limited data on the outcomes of patients treated with repeat lumpectomy at the time of ipsilateral breast tumor recurrence (IBTR). Especially, the impact of radiotherapy (RT) on a second IBTR is unknown.
Methods
We retrospectively analyzed 143 patients from 8 institutions in Japan who underwent repeat lumpectomy after IBTR. The risk factors of a second IBTR were assessed.
Results
The median follow-up period was 4.8 years. The 5-year second IBTR-free survival rate was 80.7 %. There was a significant difference in the second IBTR-free survival rate according to RT (p = 0.0003, log-rank test). The 5-year second IBTR-free survival rates for patients who received RT after initial surgery, RT after salvage surgery, and no RT were 78.0, 93.5, and 52.7 %, respectively. Multivariate analysis revealed that RT was a significantly independent predictive factor of second IBTR-free survival.
Conclusion
Repeat lumpectomy plus RT is a reasonable option in patients who did not undergo RT at the initial surgery. In contrast, caution is needed when RT is omitted in patients who have undergone repeat lumpectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mastectomy has long been regarded as the standard of care for ipsilateral breast tumor recurrence (IBTR) after breast-conserving surgery [1], although many women with breast cancer recurrence previously treated with breast-conserving surgery desire repeat lumpectomies.
At present, there are limited data on the outcomes of patients treated with repeat lumpectomy at the time of IBTR [2–7]. Most of the available data on the outcomes of patients treated with repeat lumpectomy are those of patients treated with initial breast-conserving surgery followed by radiotherapy (RT) [2–6]. On the other hand, there is little information on the outcomes of repeat lumpectomy for patients treated with initial breast-conserving surgery without RT. Despite the robust benefits of RT for local control, a recent study suggested the underutilization of RT among patients treated with initial breast-conserving surgery [8]. Data from the Surveillance, Epidemiology, and End Results registry indicate that the omission of RT increased significantly from 1992 (15.5 %) to 2007 (25 %) [8]. Therefore, it is clinically useful to verify the risk of second IBTR according to RT (i.e., RT after initial surgery, RT after salvage surgery, or no RT).
This study investigated the risk factors of second IBTR after repeat lumpectomy using data from a multi-institutional series, focusing on RT.
Patients and methods
A total of 271 consecutive patients with histologically confirmed IBTR without distant metastases who underwent definitive surgery for IBTR between 1989 and 2008 were registered from 8 institutions in Japan. This retrospective study was approved by each institutional review board. Inclusion criteria were: (1) patients who underwent breast-conserving and axillary surgery (sentinel lymph node biopsy was only allowed if these nodes had no metastases); (2) patients in whom IBTR was confirmed histologically; (3) patients who underwent definitive surgery for IBTR before 2008. Exclusion criteria were the following: (1) synchronous (defined as occurring within 3 months) metastases; (2) bilateral breast cancer patients; (3) prior malignancy other than breast cancer; (4) patients with tumors located in the skin or muscle only, without associated parenchymal disease.
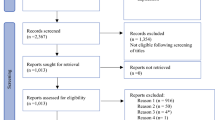
Of the 271 patients, as salvage surgery, mastectomy of the conserved breast was performed in 122 patients and repeat lumpectomy was performed in 149 patients. Of these 149 patients, 6 patients were excluded from this analysis for reasons as follows: unavailable data for radiotherapy for the ipsilateral breast (n = 3), and unavailable data for second IBTR (n = 3). Finally, 143 patients who underwent repeat lumpectomy were included in this analysis. Patients and tumor characteristics examined are listed in Table 1. Numbers of patients who received RT after the initial surgery, RT after salvage surgery, and no RT were 69, 55, and 19, respectively. One patient received RT both after the initial and salvage surgery, and this patient was included in the RT after salvage surgery group. A patient flowchart is shown in Fig. 1.
Family history was defined as positive when first-degree relatives had been diagnosed with breast cancer. For breast-conserving surgery, the margin was regarded as positive when an invasive or noninvasive component was present at the cut margin. Estrogen receptor (ER) status was determined by immunohistochemistry, and tumors with 10 % or more positively stained tumor cells were classified as positive for ER. HER2 status was considered positive if immunohistochemistry was 3+ or fluorescence in situ hybridization (her-2/neu to chromosome 17 ratio) was >2.0. Both ER and HER2 status was evaluated by each institution. Proliferation activity was assessed by immunostaining with the Ki-67 antibody (Dako). The Ki-67 index was centrally evaluated by one pathologist (N.A.), from whom all patient data were masked. The proportion of proliferating cells was determined by counting at least 500 tumor cells. Breast cancer subtypes were modified by the criteria recently recommended by the St. Gallen panelists [9]: triple-negative (ER- and HER2-negative), HER2 (HER2-positive and ER-negative), luminal-A (ER-positive, Ki-67-low, and HER2-negative), and luminal-B (ER-positive and Ki-67-high or HER2-positive or both). In this study, the cut-off value of the Ki-67 index was defined as 20 % (the median value of prior studies by Nishimura et al. [10]).
The association of RT with various clinicopathological factors was assessed using a Chi-square test.
Patients received a physical examination every 3–6 months for 5 years after salvage surgery and annually thereafter. Mammograms were performed annually after salvage surgery.
Second IBTR-free survival was calculated from the first IBTR to any local recurrence in the ipsilateral breast. Local recurrences were counted as events only when they were the first sites of failure or occurred concurrently with regional or distant metastasis. In the calculation of second IBTR-free survival, occurrences of regional or distant metastases, contralateral breast cancer, other second primary cancers, being alive without second IBTR, and deaths without evidence of recurrence were treated as censoring events.
Distant disease-free survival (DDFS) was defined as the period from the date of surgery for IBTR to the date of appearance of distant metastases.
Second IBTR-free survival and DDFS curves were calculated employing the Kaplan–Meier method. The log-rank test was used to evaluate the differences in second IBTR-free survival among the various patient subgroups. Multivariate analyses for second IBTR-free survival were performed using the Cox proportional hazards model. All of the statistical tests and p values were two-tailed, and p values of <0.05 were considered significant.
Results
Within a median follow-up period of 4.8 years (range 0.2–16.7 years), 29 of 143 patients (20.3 %) experienced a second IBTR. The 5-year second IBTR-free survival rates were 80.7 %.
Patient characteristics according to RT are shown in Table 1. There were significant differences in the tumor size of IBTR and use of trastuzumab after salvage surgery according to RT (p = 0.0128 and 0.0450, respectively, Chi-square test).
The 5-year second IBTR-free survival rates according to the various clinicopathological parameters are shown in Table 2. There was a significant difference in the second IBTR-free survival rate according to RT (p = 0.0003, log-rank test). The 5-year second IBTR-free survival rates for patients who received RT after the initial surgery, RT after salvage surgery, and no RT were 78.0, 93.5, and 52.7 %, respectively (Fig. 2). Multivariate analysis including the age at IBTR, RT, time interval from initial surgery to IBTR, margin of IBTR, ER status of IBTR, hormone therapy after salvage surgery, and chemotherapy after salvage surgery showed that age at IBTR, RT, margin of IBTR, and hormone therapy after salvage surgery were significantly independent predictive factors of second IBTR-free survival (p = 0.0026, Table 3). Furthermore, to adjust the differences in patient characteristics between 3 groups according to RT, we added the tumor size of IBTR to this multivariate analysis, and significance persisted (p = 0.0070). Because all patients with HER2-positive tumors who received RT after salvage surgery or no RT did not receive trastuzumab after salvage surgery, odds calculation of the use of trastuzumab after salvage surgery could be unstable. Therefore, we could not add the use of trastuzumab after salvage surgery to this multivariate analysis.
We also analyzed the period from the date of initial surgery to the date of appearance of second IBTR according to RT. There was also a significant difference according to RT (p = 0.0079, log-rank test).
The 5-year DDFS rates after IBTR were 78.5 %. There were no differences in DDFS after IBTR according to RT (p = 0.6241, log-rank test). Five-year DDFS rates for patients who received RT after the initial surgery, RT after salvage surgery, and no RT were 76.4, 77.9, and 88.8 %, respectively.
Discussion
Our analyses revealed that the omission of RT after repeat lumpectomy was an independent risk factor of second IBTR after repeat lumpectomy. To date, little information exists regarding the impact of RT on the risk of second IBTR after repeat lumpectomy. One report from a single institute [7] showed no association of RT with second IBTR rates after repeat lumpectomy. The different findings may result from a small sample size (n = 78). Our results suggested that the omission of RT after repeat lumpectomy resulted in unacceptably high second IBTR rates in cases of RT absence after the initial breast-conserving surgery. Therefore, caution is needed when RT is omitted in patients who have undergone repeat lumpectomy. Although 5-year second IBTR-free survival for patients treated with RT after the initial breast-conserving surgery (78.0 %) was inferior to that for RT after salvage surgery (93.5 %) and unacceptable, RT after the initial breast-conserving surgery might also suppress the second IBTR, because it achieved apparently better outcomes than no RT (52.7 %). It is speculated that RT after initial breast-conserving surgery eradicated subclinical diseases left behind, at least to some degree.
One could assume that there were no differences in the periods from the date of initial surgery to the date of appearance of second IBTR according to RT because the time interval from initial surgery to IBTR might be shorter in patients who did not receive RT after initial surgery than in those who did. However, in this study, there was no difference in the time interval from initial surgery to IBTR according to RT. Furthermore, there was also a significant difference in the period from the date of initial surgery to the date of appearance of second IBTR according to RT. Therefore, the assumption that there were no differences in the periods from the date of initial surgery to the date of appearance of second IBTR according to RT is not correct.
In this study, second-IBTR rate after repeat lumpectomy plus RT was acceptably low. However, our results do not indicate that RT after initial breast-conserving surgery can be omitted because RT after initial breast-conserving surgery not only substantially reduces the risk of recurrence but also moderately reduces the risk of death from breast cancer [11].
In our study, the age at IBTR, margin of IBTR, and hormone therapy after salvage surgery were also significantly independent predictive factors of second IBTR-free survival. Kurtz et al. [2] reported their experiences involving 50 patients who underwent repeat lumpectomy after IBTR, and reported that late recurrence with a negative surgical resection margin predicted more favorable local control after IBTR. This result was compatible with ours. Age and hormone therapy are both well-known risk factors of IBTR after initial breast-conserving surgery.
Recently, the breast cancer subtype has become known to be useful in estimating the risk of not only distant [12, 13] but also locoregional recurrences [14–16]. Our previous analysis suggested that the breast cancer subtype, as approximated by ER, HER2, and Ki-67 of IBTR, was associated with distant recurrence in patients with IBTR, which was reported elsewhere [17]. However, no association of the breast cancer subtype with second IBTR was observed in this study. To our knowledge, there has been no report regarding the role of the breast cancer subtype in second IBTR after repeat lumpectomy.
In conclusion, the omission of RT after repeat lumpectomy was an independent risk factor of second IBTR after repeat lumpectomy. Caution is needed when RT is omitted in patients who have undergone repeat lumpectomy. In contrast, repeat lumpectomy plus RT is a reasonable option in patients who did not undergo RT at the initial surgery.
References
Clemons M, Hamilton T, Mansi J, Lockwood G, Goss P. Management of recurrent locoregional breast cancer: oncologist survey. Breast. 2003;12:328–37.
Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Is breast conservation after local recurrence feasible? Eur J Cancer. 1991;27:240–4.
Voogd AC, van Tienhoven G, Peterse HL, Crommelin MA, Rutgers EJ, van de Velde CJ, et al. Local recurrence after breast conservation therapy for early stage breast carcinoma: detection, treatment, and outcome in 266 patients. Dutch Study Group on Local Recurrence after Breast Conservation (BORST). Cancer. 1999;85:437–46.
Alpert TE, Kuerer HM, Arthur DW, Lannin DR, Haffty BG. Ipsilateral breast tumor recurrence after breast conservation therapy: outcomes of salvage mastectomy vs. salvage breast-conserving surgery and prognostic factors for salvage breast preservation. Int J Radiat Oncol Biol Phys. 2005;63:845–51.
van der Sangen MJ, van de Poll-Franse LV, Roumen RM, Rutten HJ, Coebergh JW, Vreugdenhil G, et al. The prognosis of patients with local recurrence more than five years after breast conservation therapy for invasive breast carcinoma. Eur J Surg Oncol. 2006;32:34–8.
Gentilini O, Botteri E, Veronesi P, Sangalli C, Del Castillo A, Ballardini B, et al. Repeating conservative surgery after ipsilateral breast tumor reappearance: criteria for selecting the best candidates. Ann Surg Oncol. 2012 (Epub ahead of print).
Ishitobi M, Komoike Y, Nakahara S, Motomura K, Koyama H, Inaji H. Repeat lumpectomy for ipsilateral breast tumor recurrence after breast-conserving treatment. Oncology. 2011;81(5–6):381–6.
Tuttle TM, Jarosek S, Habermann EB, Yee D, Yuan J, Virnig BA. Omission of radiation therapy after breast-conserving surgery in the United States: a population-based analysis of clinicopathologic factors. Cancer. 2012;118:2004–13.
Goldhirsch A, Wood WC, Coates AS, Gelber RD. Thürlimann B, Senn HJ, et al. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer. Ann Oncol. 2011;22:1736–47.
Nishimura R, Osako T, Okumura Y, Hayashi M, Toyozumi Y, Arima N. Ki-67 as a prognostic marker according to breast cancer subtype and a predictor of recurrence time in primary breast cancer. Exp Ther Med. 2010;1:747–54.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–502.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 Index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
Mamounas EP, Tang G, Fisher B, Paik S, Shak S, Costantino JP, et al. Association between the 21-gene recurrence score assay and risk of locoregional recurrence in node-negative, estrogen receptor-positive breast cancer: results from NSABP B-14 and NSABP B-20. J Clin Oncol. 2010;28:1677–83.
Millar EK, Graham PH, O’Toole SA, McNeil CM, Browne L, Morey AL, et al. Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol. 2009;27:4701–8.
Nguyen PL, Taghian AG, Katz MS, Niemierko A, Raad RFA, Boon WL, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 Is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol. 2008;26:2373–8.
Ishitobi M, Okumura Y, Arima N, Yoshida A, Nakatsukasa K, Iwase T, et al. Breast cancer subtype and distant recurrence after ipsilateral breast tumor recurrence. Ann Surg Oncol. 2013. doi:10.1245/s10434-012-2825-1.
Acknowledgments
We thank Dr. Takuji Iwase and Dr. Takehiro Tanaka for critical reading of the manuscript. This study was supported in part by Grants-in-Aid for Scientific Research from the Japanese Breast Cancer Society. Dr. Tetsuya Taguchi received a research grant from Takeda and Chugai. Other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
About this article
Cite this article
Ishitobi, M., Okumura, Y., Nishimura, R. et al. Repeat lumpectomy for ipsilateral breast tumor recurrence (IBTR) after breast-conserving surgery: the impact of radiotherapy on second IBTR. Breast Cancer 21, 754–760 (2014). https://doi.org/10.1007/s12282-013-0454-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-013-0454-6